Ch. 16 - Physician Shortage and Physician Workforce Challenge
Ryan Koski-Vacirca; Nathan VanderVinne, DO, MPH; Bradley Burmeister, MD
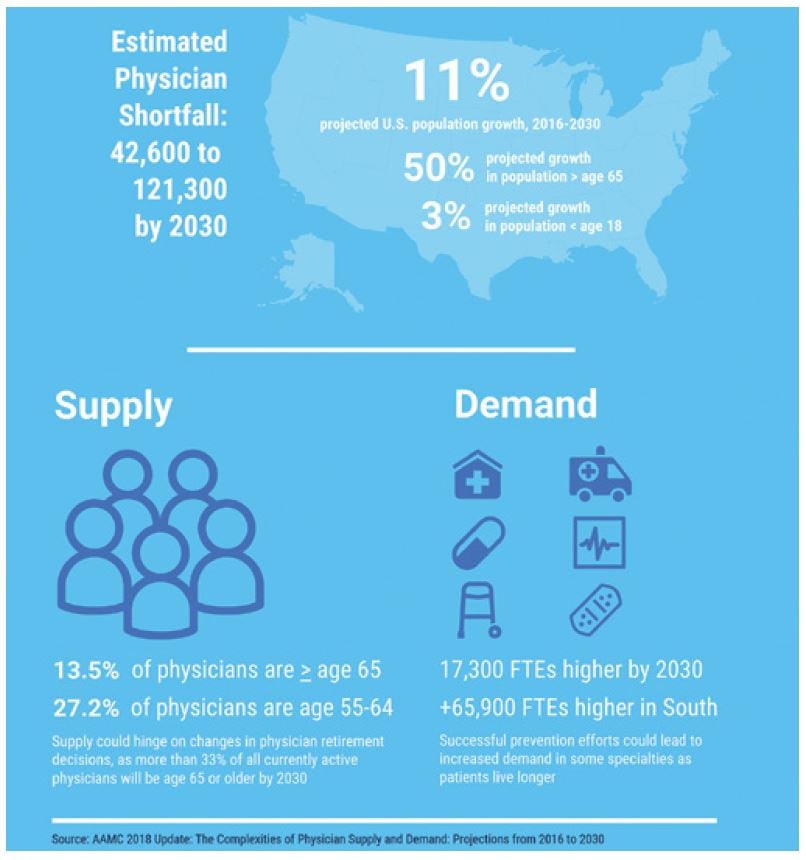
A report by the Association of American Medical Colleges predicts a shortfall between 42,600 and 121,300 physicians by the year 2030 in the face of growing demand from an aging population.1 Within emergency medicine, there has been a recent increase in the number of residents, residencytrained emergency physicians and APPs entering the workforce; however, demand is still expected to outpace supply, especially in rural areas.
Physician workforce shortages represent an increasing challenge facing the United States.
Demographics Changes
Population growth and aging continue to be the main drivers of the projected physician shortage. The 2018 AAMC study indicates that during the period of 2016–2030, the U.S. population is projected to grow by almost 11%, increasing from about 324 million to 359 million. Under the current rate of workforce growth over the same period, overall physician supply is expected to increase by 7% to 846,600. While improving, this rate of physician growth will represent a 3% decline in the physician-to-population ratio by 2030.1
The medical system will face new strains as a result of its own population health success and an aging population. The past few decades have seen an improvement in overall public health secondary to reducing excess body weight, improving control of blood pressure, cholesterol and blood glucose levels, and reducing the prevalence of smoking.1 With these improvements, people are expected to live longer with more comorbidities. The proportion of Americans age 65 and older will grow faster than other groups, increasing by more than 50%. Older adults also contribute to the trend in increasing ED visits; recent analysis of ED visits from 2006–2014 found that the 18.4% increase in overall ED visits was mainly driven by patients age 50 and older, with chronic illnesses or Medicaid insurance.2 The longevity associated with improved population health will result in greater demand for services by 2030.
Other factors reducing the physician supply is the trend toward physicians working reduced hours and changes in the retirement age. Between 2002 and 2016 there was a trend toward physicians of all ages working fewer hours. If this trend continues, by 2030 there will be 32,500 fewer full time equivalent physicians in the national supply. In addition to fewer hours worked, changes in retirement decisions could dramatically alter the medical landscape. Currently more than one-third of all active physicians will be 65 or older before 2030. Physicians between age 65 and older account for 13.5% of the active workforce, and those ages 55–64 make up nearly 27.2% of the active workforce.1
Emergency Medicine Challenges
The overall physician supply-demand mismatch affects the ED; however, there has been a dramatic increase in the number of emergency physicians entering the workforce in the past decade. Compared to primary care, the physician shortage is less severe for EM; however, the high volumes of the ED make it more sensitive to health system challenges. Emergency physicians make up less than 5% of all doctors, but they handle a quarter of all acute care encounters.3 Already carrying a disproportionate burden of acute care visits, emergency physicians have learned to do more with less: more ED visits with simultaneously fewer EDs remaining open to see patients. According to the American Hospital Association, 12.5% of all EDs and hospitals closed between 1994 and 2014, with a decrease from 4,960 to 4,408 EDs nationwide. Over this same time there was a massive 51.2% increase in ED visits, reaching 136 million visits by 2014. To make matters worse, the hospitals that closed were more likely to be safety-net hospitals serving a higher share of impoverished populations.4
Emergency medicine has risen to the challenge with a large influx of both residency positions and APPs to serve the community needs. Between 2000 and 2010, the number of emergency physicians increased by 44.6%, more than any other specialty.5 Estimates of active physicians vary by source, but more recent data suggests the number of practicing emergency physicians (including EM trained, family medicine, and internal medicine practicing EM) grew from 39,061 in 20086 to 44,253 in 20147 — another 13% increase. The proportion of nonemergency physicians comprising the EM workforce has fallen over time as EM residency-trained, board-certified physicians enter the workforce, dropping from 31% to 14.3%. Authors from a 2016 workforce study estimate that by 2023 there will be enough board-certified emergency physicians to care for all ED patients in the U.S. To arrive at this projection, the study accounted for 2,050 emergency medicine residents entering the workforce each year and a 1.7% attrition rate, for a net gain of approximately 1,283 board-certified physicians per year.8
EM training programs have increased in the past decade, and the specialty continues to be a popular selection for graduating medical students. Heeding the concerns of a physician shortage, community hospitals, private health care systems, industry groups and academic medical centers have established new graduate medical education programs. As of the 2018 Match, EM has become the fourth largest specialty for U.S. allopathic medical school seniors and third largest specialty for matched osteopathic applicants.9 In 2009, there were 149 allopathic residency programs, and as of 2019, there are 240 ACGME-accredited residencies. It’s important to note that many of these “new” programs are osteopathic residencies transitioning into the allopathic match through the Single Accreditation
process.10 Through this merger, which began in 2014 and will be complete in 2020, the ACGME Review Committee for Emergency Medicine has accredited at least 49 programs to leave the AOA match and join the NRMP match.11
FIGURE 16.1. Physician Workforce Supply and Demand Outlook to 2030
Other factors contributing to the strain on EM physicians mirror the challenges faced in other parts of the health care system. The projected shortage of primary care specialties — between 14,800 to 49,300 physicians by 20301 — will exacerbate health care access issues, especially for Medicaid patients. With the increased difficulty in seeking primary care in a timely manner, Medicaid patients are likely to increase ED usage in response.12 In addition to a lack of available services outside the ED, the large increase in the number of Medicaid enrollees from the ACA expansion will also increase ED volume, as this group has been shown to be one of the main drivers of increased ED use.13 Other health system issues contributing to ED crowding and strain include the increased availability
and use of advanced testing, medical complexity of patients14 and intensity of visits,15,16 and burdensome governmental regulations.
Women in the Workforce
There is a tremendous gender underrepresentation of women in emergency medicine. In 2015, women represented 34% of all physicians, but only 26.6% of emergency physicians.17
While the proportion of women in emergency medicine is increasing over time, it is not to the same degree as medicine as a whole. In 2018, 48.8% of medical school matriculants were female, but only 37.3% (2015 data) of EM residents, suggesting that female medical school graduates are less likely to pursue emergency medicine training.18
Women experience disparities in income, promotions, and leadership.19 Mean overall salary was $278.631 (SD +/-$68.003). The mean (+/- SD) salary of women was $19,418 (+/-$3,736) less than men (p < 0.001), even after adjusting for race, region, rank, years of experience, clinical hours, core faculty status, administrative roles, board certification, and fellowship training.20 Similarly, only 15% of department chair/vice chair are female.
A set of best practices for employment was developed by EM leaders in 2014 to advance women.21 The recommendations pertain to recruitment, support, advisory, and oversight on recruitment strategies. They are based in the belief that physicians should not have to choose between their careers and their families. The recommendations for employers include:
- Ensure unbiased recruitment and hiring, along with parity in advancement and compensation among employees.
- Support networking and mentorship opportunities
- Implement family-supportive practices that further the professional advancement and retention of employees who have childcare and other dependent care responsibilities.
- Create a culture in which family-supportive policies are visible, easily accessible, evident at recruitment, and used without fear of penalty or stigma
- Support physicians during significant life events (eg, pregnancy, childbirth, adoption, major medical illness).
- Support the needs of pregnant and postpartum women with flexible scheduling options and adequate lactation facilities.
Underrepresented Minorities in the Workforce
Black, Hispanic, and Native American physicians continue to make up a small proportion of physicians, experiencing little progress over the past two decades with representation in medicine as a whole or in EM specifically. Although 30% of the U.S. population identifies as under-represented minorities, only 9% of EM physicians self-identify that way. Because emergency physicians treat a disproportionately large percentage of Medicaid enrollees — who are majority under-represented groups — this representation gap is particularly important for our specialty.22,23 Equally importantly, new data continue to support the conclusion that representation in the health care workforce improves health outcomes for under-represented patients:24 ACEP and EMRA have institutionally prioritized diversification of the EM workforce, holding a diversity summit in 2016 and introducing an ACEP Leadership Development Advisory Committee in 2018 charged with mentorship of under-represented ACEP members. Similarly, ACEP revised a policy statement in November 2017 endorsing the diversification of hospital staffing.25 For the past several years, EMRA has worked to compile a list of diversity-oriented visiting elective scholarships available for current medical students.26
Rural Emergency Medicine
Rural America is particularly affected by the shortage of emergency physicians. Research following new doctors found that 4 of every 5 new physicians start working in areas that already have a high supply, leaving rural areas perpetually underserved.27 While 21% of the U.S. population lives in rural areas, only 12% of emergency physicians practice there. Not only is the density of emergency physicians lowest in rural settings (10.3 urban vs. 5.3 large rural vs. 2.5 small rural), but also the percentage of emergency physicians with residency training in emergency medicine is lower as well. Rural physicians who identify as having emergency medicine as a specialty are less likely to have formal emergency medicine training (31% vs. 57%), be board certified (43% vs. 59%) or to have
graduated in the past 5 years (8% vs. 19%).7
Importantly, new data show that while 64% of all emergency medicine practitioners in urban counties are emergency physicians, only 45% of practitioners in rural counties are. Rural counties make up the difference largely with non-emergency trained physicians: non-emergency physicians make up 12% of EM clinicians in urban counties, but more than 28% of EM clinicians in rural counties. The percentage of EM clinicians who are advanced practice providers is relatively similar between urban and rural counties at 24.1% and 26.8%, respectively.28
There have been several initiatives to help recruit physicians to rural areas. Of particular effectiveness are rural rotations in residency training. Not only do rural offer unique training opportunities, but they also increase the likelihood of EM residents returning to rural areas. Additional recruitment strategies including loan repayment programs, signing bonuses, telemedicine, and recruiting residents from rural communities for training have shown some benefit in increasing the penetration of board certified physicians in rural communities.28
Finally, the number of EM resident spots has increased significantly in the past decade. The AAMC and others continue to predict a physician shortfall of more than 40,000 by 2030, which has spurred community hospitals, private health care systems, and academic medical centers to establish new GME programs. To this end, in 2017, 152 more EM residency spots were available than the year prior, for a total of 2,047.
Financial Incentives for Geographic Redistribution and Diversity
Governmental loan assistance programs can help improve the uneven geographic distribution of emergency physicians, but these opportunities are limited. One such example is the HRSA loan repayment program, the National Health Service Corps,28 which recruits physicians to work in health professional shortage areas in return for repayment of education loans up to $25,000 per year. Currently the NHSC covers primary care physicians including geriatrics, obstetrics/gynecology, pediatrics, internal, and family medicine, but it excludes emergency medicine. Similarly, the Indian Health Service offers a loan repayment program that repays up to $40,000 in student loans for a 2-year service commitment to practice in health facilities serving American Indian and Alaska Native communities with the greatest staffing needs.
Another option is the Public Service Loan Forgiveness Program, established in 2007. This is a federal program that, after 10 years of qualifying monthly payments, forgives the remaining student loan debt for employees of certain public and nonprofit institutions. Many hospitals or EM employers in the U.S. are for-profit corporations; this loan incentivizes physicians working at federal, state, or tribal government organizations and nonprofits (ie, many teaching hospitals). To be eligible, physicians need to enroll in specific payment plans that include Pay As You Earn, Income-Based Repayment, and Income-Contingent Repayment. The original loans must be federal loans from the Direct Loan Program.
Other ways in which the government could offset the financial burden of medical education in general as a method to increase the diversity of those entering medicine include resident loan forbearance and deferment and the tax deductibility of student loan payment. Given the long range planning for the PSLF, it is worth noting that recent federal legislation such as the Promoting Real Opportunity, Success, and Prosperity through Education Reform (PROSPER) Act introduced by Rep. Virginia Foxx in 2017 would have potentially eliminated the program, among other changes. The PROSPER Act did not pass the House, but often bills that are initially unsuccessful are reintroduced multiple times. Similarly, the PSLF was proposed to be eliminated in the 2019 budget by President Donald Trump; however, this was not enacted.
Physician Workforce Study — Unfunded Mandate of the ACA
Section 5101 of the Affordable Care Act created the National Health Care Workforce commission with the intent to provide data and impartial advice to Congress. Since passage of the ACA, the workforce has remained unfunded. Although no specific amount of funding is required, previous budget requests have been along the lines of $3 million. The commission members were appointed in 2010; however, federal appropriations laws prohibit the workforce from meeting until it’s funded by Congress. Without funding a single unbiased source of data to detail workforce needs, the challenges of how to allocate resources and determine how best to improve our workforce will remain difficult.
WHAT’S THE ASK?
- Understand the demographic, lifestyle, and health care changes that are resulting in workforce challenges.
- Advocate for policies that address the underlying causes of physician workforce challenges, including workforce diversity, student loan forgiveness programs, etc.
- Mentor rising students to encourage entry into — and sustained careers in — emergency medicine.




