Greater occipital nerve block (GONB) has emerged as a promising treatment option for acute headaches in the emergency department (ED).
GONB involves injecting a local anesthetic and/or a steroid into the area surrounding the greater occipital nerve to provide rapid pain relief for patients. Several studies have evaluated the efficacy of the GONB for treating acute headaches in the ED, with positive results for migraines, tension-type and cluster headaches. The benefit of the GONB includes rapid relief of pain, a low risk of adverse effects and the potential to reduce the need for opioid for pain management in the ED. GONB are a safe and effective option for headaches in the ED, providing emergency physicians with a valuable tool for pain management.
Introduction
Headache remains one of the most common chief complaints in the emergency department, accounting for roughly 4 million visits in 2016.1 The most crucial part of ED physicians’ assessment and management is to rule out secondary causes of headaches, such as subarachnoid hemorrhage, hematoma, or meningitis. However, those secondary causes are uncommon and have clear diagnostic and management guidelines in the ED. On the other hand, the diagnostics and management of primary headaches are not clearly outlined. This is evident in patients’ satisfaction with the treatment received in the ED, as a study reported that 20% of patients presenting to the ED were headache free by the time of discharge. Additionally, 64% of the patients had recurrence within 24 hours from discharge.2 Unfortunately, those patients are subject to more unnecessary ED testing.3
A study showed that only 38% of the time, patients were satisfied with their management in the ED.3 On the other hand, 62% of the time, headache physicians were inconsistently satisfied or not satisfied by their patients' management in the ED.3 This was mainly due to the absence of clear management guidelines for migraines in the ED and the wide variety of possible medication combinations, including NSAIDs, acetaminophen, antiemetics, and/or triptans.3 Other issues that ED physicians face are the contraindications some patients might have to some of the medications being used; for instance, the use of triptans in patients with coronary artery disease or the use of prochlorperazine in patients with QT prolongation.
Many studies have been done to check the efficacy of 2nd line management of migraines in the ED. One of the emerging 2nd line treatments is nerve blocks for headaches in EDs, especially with the increased number of point-of-care ultrasound (POCUS) trained ED physicians and fewer systemic side effects from the local blocks. Given its applicability in the ED, we aim to review the latest evidence in treating migraine headaches with GONB.
The Procedure
The greater occipital nerve is a sensory nerve that arises from the medial ramus of C2 spinal nerve and travels between C1 and C2 vertebrae and ascends to pass through the suboccipital triangle towards the occipital bone. As it approaches the occipital bone, the nerve passes between the semispinalis capitis (SSC) and oblique capitis inferior (OCI) muscle and then it pierces the belly of the SSC and aponeurosis of the trapezius muscle.4
Using the linear probe for the procedure, determine the initial point of ultrasound probe placement by palpating the external landmarks, the mastoid process and the odontoid process of the axis which can be palpated just below the occiput while the head is in slight flexion. The probe then is placed obliquely over the area between the two processes with the medial end of the probe being over the odontoid process. The internal landmarks to be identified after the proper probe placement are the SSC and OCI with the occipital nerve running between them (Figure 1).
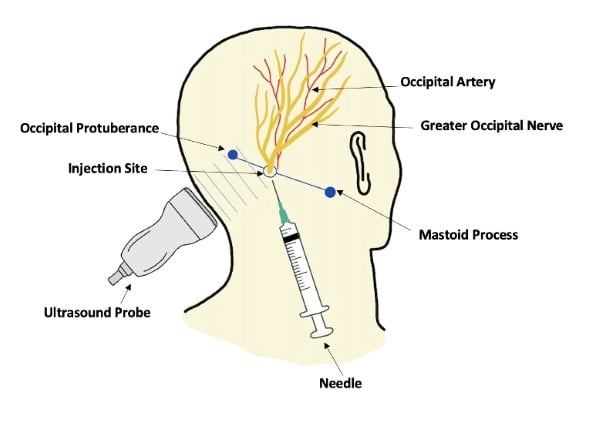
The occipital artery can be used to identify the nerve as it lies lateral to the occipital nerve.5 Once the nerve is identified, cleanse the area, then using a 25-27 gauge needle, inject a small amount of local anesthetic over the site creating a wheel to decrease the patient’s discomfort during the procedure. Afterward, using an inferolateral approach, the block needle is inserted and guided in the same direction of the ultrasound probe until the needle tip is visualized between the SSC and OCI and near the greater occipital nerve. A small amount (2-3 mL) of normal saline can be injected and visualized to confirm the correct needle location just over the nerve. Once confirmed, the local anesthetic can be injected over the target area. The choice of local anesthetic includes either lidocaine 2% (2 mL) or bupivacaine 0.5% (2 mL) with the addition of either dexamethasone 2mg/mL (2mL) or methylprednisolone 40 mg/mL (2mL) with a total injection volume not exceeding 4 mL.6
Discussion
Headaches are a pervasive problem that leads many individuals to seek pain management at the emergency department. These headaches are often excruciating and can cause significant distress and high socioeconomic burden. Among the numerous treatments available for acute headaches in the ED, the GONB has emerged as a promising option, especially for headaches that are refractory to traditional headache medication such as NSAIDs, acetaminophen, and metoclopramide.7 The GON is a sensory nerve that supplies sensation to the scalp and is commonly implicated in tension-type, migraines and cluster headaches.8
The GONB is a procedure that targets the trigeminocervical complex in the scalp, which is believed to be responsible for transmitting pain signals in the head.9 Over the years, several studies have examined the efficacy of the GONB in the treatment of acute headaches in the ED. One of these studies found that administering lidocaine as part of the GONB resulted in immediate relief of migraines and effective treatment of cluster headaches, cervicogenic headaches and occipital neuralgia.10 A randomized controlled trial conducted as a double-blinded, placebo-controlled study evaluated the effectiveness of the GONB significantly reduced migraine pain compared to the placebo group, providing much-needed pain relief to those suffering from the condition.11 Similarly, another RCT using bupivacaine in the GONB effectively reduced headache pain intensity and increased the number of headache-free days.12
The GONB is a procedure with numerous benefits that make it a valuable treatment option for acute headaches in the ED setting especially with recent advancements in regional anesthesia. The procedure can be performed quickly and without the need for any oral or intravenous medication. Furthermore, patients often experience rapid pain relief within minutes to hours of receiving the block. It is a safe and well-tolerated procedure with few reported adverse effects. The most common adverse effects are mild and include injection site pain, dizziness and neck pain. Serious adverse effects are rare but may include infection, hematoma and nerve injury.13
Another important benefit of the GONB is its potential to reduce the need for opioid prescriptions for pain management in the ED. Opioids are commonly used for the treatment of acute headaches that are refractory to standard medication, but they come with a significant risk of adverse reactions such as respiratory depression and the potential for addiction. One study showed that the GONB was an effective and safe alternative to opioids for patients with acute headaches. By providing GONB as an alternative treatment, health care providers can help reduce the use of opioids and associated risk factors.14
Conclusion
In conclusion, the GONB is a promising treatment option for acute headaches in the ED setting. It provides rapid pain relief, reduces the need for opioids, and has a low risk of adverse effects. The procedure is easy to perform and can be a valuable tool for emergency physicians in the treatment of acute headaches.
References
- Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: Updated age, sex, and socioeconomic-specific estimates from government health surveys. Headache. 2021;61(1):60–68.
- Minen MT, Loder E, Friedman B. Factors associated with emergency department visits for migraine: An observational study. Headache. 2014;54(10): 1611–1618.
- Minen MT, Ortega E, Lipton RB, Cowan R. American Headache Society Survey About Urgent and Emergency Management of Headache Patients. Headache. 2018 Oct;58(9):1389-1396.
- Cho JCS, Haun DW, Kettner NW, Scali F, Clark TB. Sonography of the normal greater occipital nerve and obliquus capitis inferior muscle. J Clin Ultrasound. 2010;38(6):299–304.
- Fernandes L, Randall M, Idrovo L. Peripheral nerve blocks for headache disorders. Pract Neurol. 2020;
- Austin M, Hinson MR. Occipital Nerve Block. In StatPearls. StatPearls Publishing. 2023.
- Gupta S, Oosthuizen R, Pulfrey S. Treatment of acute migraine in the emergency department. Can Fam Physician. 2014;60(1):47–49.
- Vanterpool SG, Heidel RE, Rejoub LR. Targeting Occipital Headache Pain: Preliminary Data Supporting an Alternative Approach to Occipital Nerve Block. Clin J Pain. 2020;36(4):289–295.
- Bartsch T, Goadsby PJ. The trigeminocervical complex and migraine: Current concepts and synthesis. Curr Pain Headache Rep. 2003;7(5):371–376.
- Terzi T, Karakurum B, Üçler S, İnan LE, Tulunay C. Greater occipital nerve blockade in migraine, tension-type headache and cervicogenic headache. J Headache Pain. 2002;3(3):137–141.
- Inan LE, Inan N, Karadaş Ö, Gül HL, Erdemoğlu AK, Türkel Y, Akyol A. Greater occipital nerve blockade for the treatment of chronic migraine: A randomized, multicenter, double-blind, and placebo-controlled study. Acta Neurol Scand. 2015;132(4), 270–277.
- Zhang H, Yang X, Lin Y, Chen L, Ye H. The efficacy of greater occipital nerve block for the treatment of migraine: A systematic review and meta-analysis. Clin Neurol Neurosurg. 2018;165:129–133.
- Ashkenazi A, Levin M. Greater occipital nerve block for migraine and other headaches: Is it useful? Curr Pain Headache Rep. 2007;11(3):231–235.
- Floyd SB, NcGarby S, Cordero Romero S, Garrison S, Walker K, Hendry W, Moschella PC. Emergency Department Alternatives to Opioids: Adapting and Implementing Proven Therapies in Practice. Int J Environ Res Public Health. 2023;20(2):1206.



