Nearly 6.7 million Americans over the age of 20 have been diagnosed with heart failure.1 It is estimated that more than 2,500 people with heart failure receive a Left Ventricular Assist Device (LVAD) in the United States.2
Given the increasing prevalence, it is imperative that emergency medicine physicians know how to adequately triage and treat LVAD patients. This article will cover the basics of LVADs and provide a framework to ensure effective treatment of patients with a LVAD.
Indications for LVAD
Not every heart failure patient may qualify for a LVAD. As there can be a long wait on the heart transplant list, LVAD technology has been created and reformed to provide patients with durable mechanical support that enables out of hospital care while they wait for a new heart.3 Some patients who don’t qualify for transplant live with their LVADs as “destination therapy.”
LVAD Components
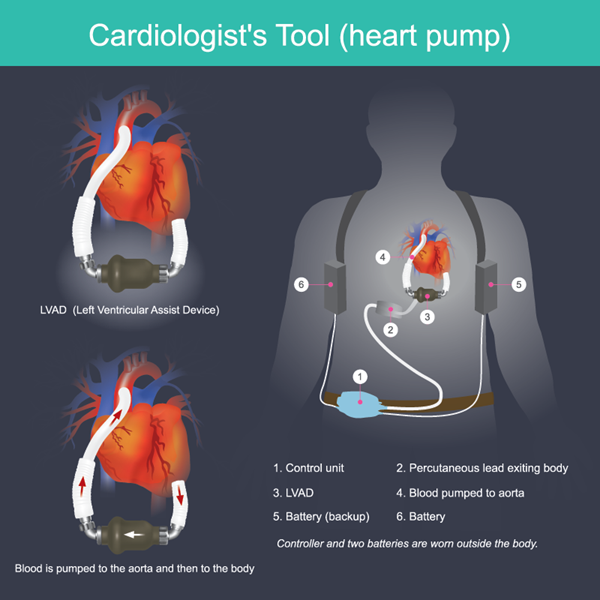
There are three types of LVADs with which an EM physician should be familiar: the HeartMate II (Thoratec/St. Jude/Abbott), HVAD (HeartWare/Medtronic), and HeartMate 3 (Abbott). Each of these devices function similarly and have similar components that one should be able to understand and manage.
There are 4 main components of the LVAD:
- Pump
- Driveline
- System controller
- Power supply
The inflow cannula allows blood into the pump and the outflow allows blood to bypass the LV and enter the aorta to distribute blood to the rest of the body.
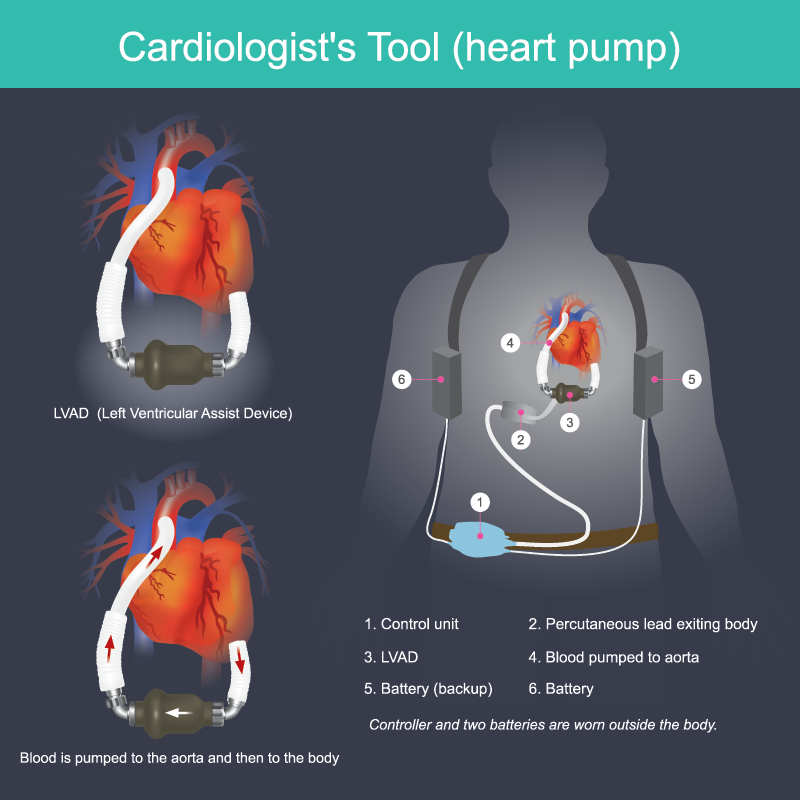
Figure 1: LVAD components 4,5
- Pump
The job of the LVAD pump is fairly intuitive: it bypasses the intrinsic contractility of the LV via the inflow cannula and the motor propels blood into the aorta via the outflow cannula. - Driveline
This is only part of the LVAD that is outside of the patient’s body (aside from the battery). The driveline connects the pump to the system controller and power supply. - System Controller
The system controller serves as the main display for battery life, alarms, and additional device metrics. - Power Supply
The power supply is the battery pack for the LVAD. It includes batteries and also a power cord that plugs directly into the wall.
ED EVALUATION OF PATIENTS WITH LVAD PHYSIOLOGY
C-ABCDEs of LVAD Management
The initial assessment of the LVAD patient is the same as any other in the emergency department, with a few caveats. The first call should be to the LVAD coordinator (most patients/families know the direct access phone number to their LVAD coordinator), and this should be done simultaneously while evaluating the classic “ABCDE” of emergency medicine. The rest of the assessment is the same with a few additions that are specific to LVAD management.
Table 1. ED Assessment of LVAD Patient3
|
WHAT TO ASSESS |
WHAT TO LOOK FOR |
|
|
C |
Call the LVAD coordinator |
Confirm with patient/family |
|
A |
Appearance Auscultation |
Alert, warm, well-perfused Smooth hum |
|
B |
Battery Blood pressure |
Charged and connected to main power source MAP 70-90 |
|
C |
Controller |
Alarms Cool (not overheated) Device metrics at baseline |
|
D |
Driveline |
Intact, no evidence of damage or infection |
|
E |
Echo (bedside) EKG |
Compare with prior echo: baseline ventricular size, tamponade physiology, AV disease and RV size/function |
A: Appearance & Auscultation
As soon as LVAD patients are placed in a room, one can perform a quick visual assessment. Specifically, things to look for include making sure they are awake, alert, warm and well-perfused. During your ED assessment of ABCs, you can check for the typical mechanical whirr of the LVAD device.
B: Battery & Blood Pressure
While the patient is being hooked up to the monitor and you are performing your initial ABCs, it is imperative that the LVAD is connected to a main power source. At the same time, one should quickly obtain a blood pressure. LVAD patients have minimal or zero pulsatility. Thus, a MAP is the most reliable measure of perfusion pressure. Goal MAP should be between 70 and 90 mmHg. LVAD patients are preload-dependent and afterload-sensitive.6
C: Controller
There are several reasons that an LVAD would alarm such as low battery, concern for a disconnection, or any other similar malfunction. The alarms to be concerned about include those regarding changes in pulsatility and flow. See Figure 2 for a broad differential for these variations.
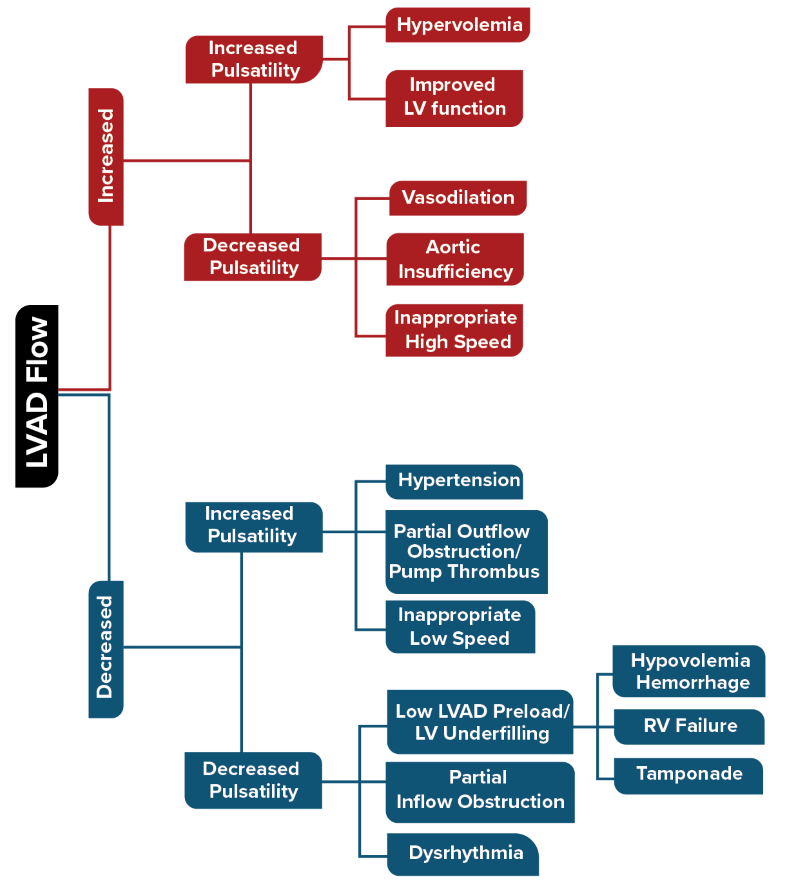
Figure 2. Causes of variable LVAD flow and subsequent pulsatility3
D: Driveline
The driveline should be intact without evidence of infection at the abdominal wall site. An X-ray or CT is also helpful to assess for internal fracture or infection contributing to a patient's presentation.
E: Echo & EKG
For LVAD patients who are hypotensive with unclear etiology, a bedside echo is helpful to ascertain the primary concern and further hone a differential. The echo should start with the parasternal axis view to assess for over- versus under-distension. If possible, additional important views include a short-axis view of the AV and an apical 4chamber view. The differential for both situations is similar to that of a non-LVAD patient. Figure 3 provides a differential for LVAD complications based on echo.
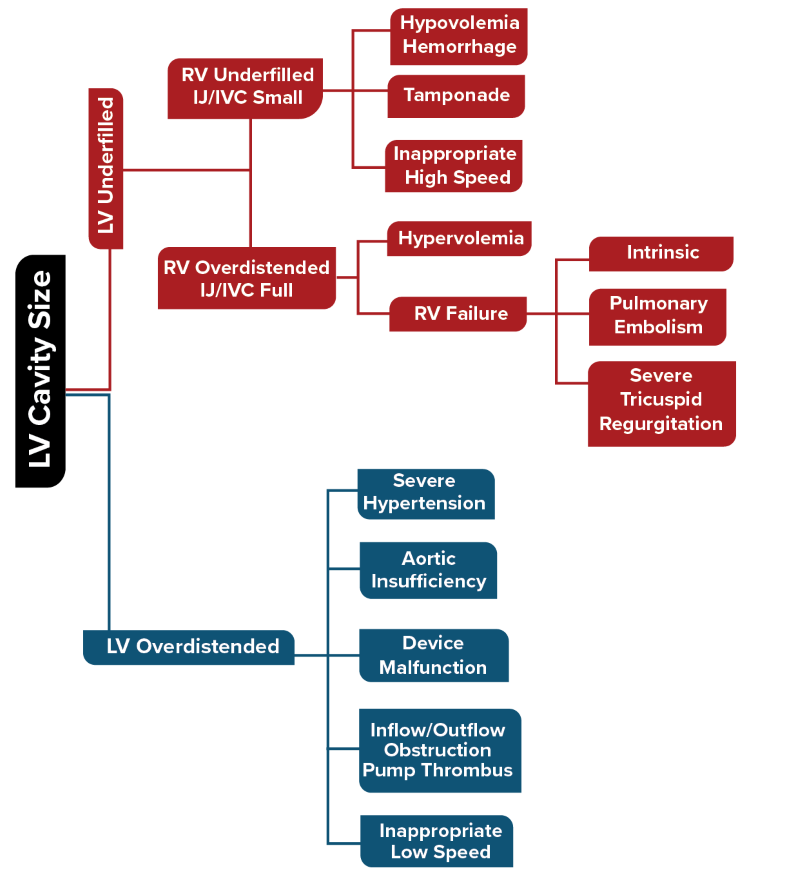
Figure 3. Differential for LVAD complications based on echo findings3
EMERGENT LVAD COMPLICATIONS
Life-threatening complications that every ED clinician should be aware of in LVAD patients can be remembered with this helpful mnemonic: “DEATHS” (outlined below in Table 2). All of these complications are fairly intuitive and can be managed as one would any other ED patient.
Table 2. LVAD emergencies (DEATHS)
|
D |
Driveline complications Device failure |
Fracture: assess with XR, consult cardiac surgery Infection: administer antibiotics Device failure: see below |
|
E |
Embolism |
Anticoagulation |
|
A |
Arrhythmia |
Cardioversion vs. defibrillation, rate control, electrolyte repletion |
|
T |
Thrombus |
Check INR, LDH, echo, consider surgery |
|
H |
Hemorrhage |
Anticoagulation reversal |
|
S |
“Suckdown”6 |
Consider echo, fluids |
Device Failure and Cardiac Arrest
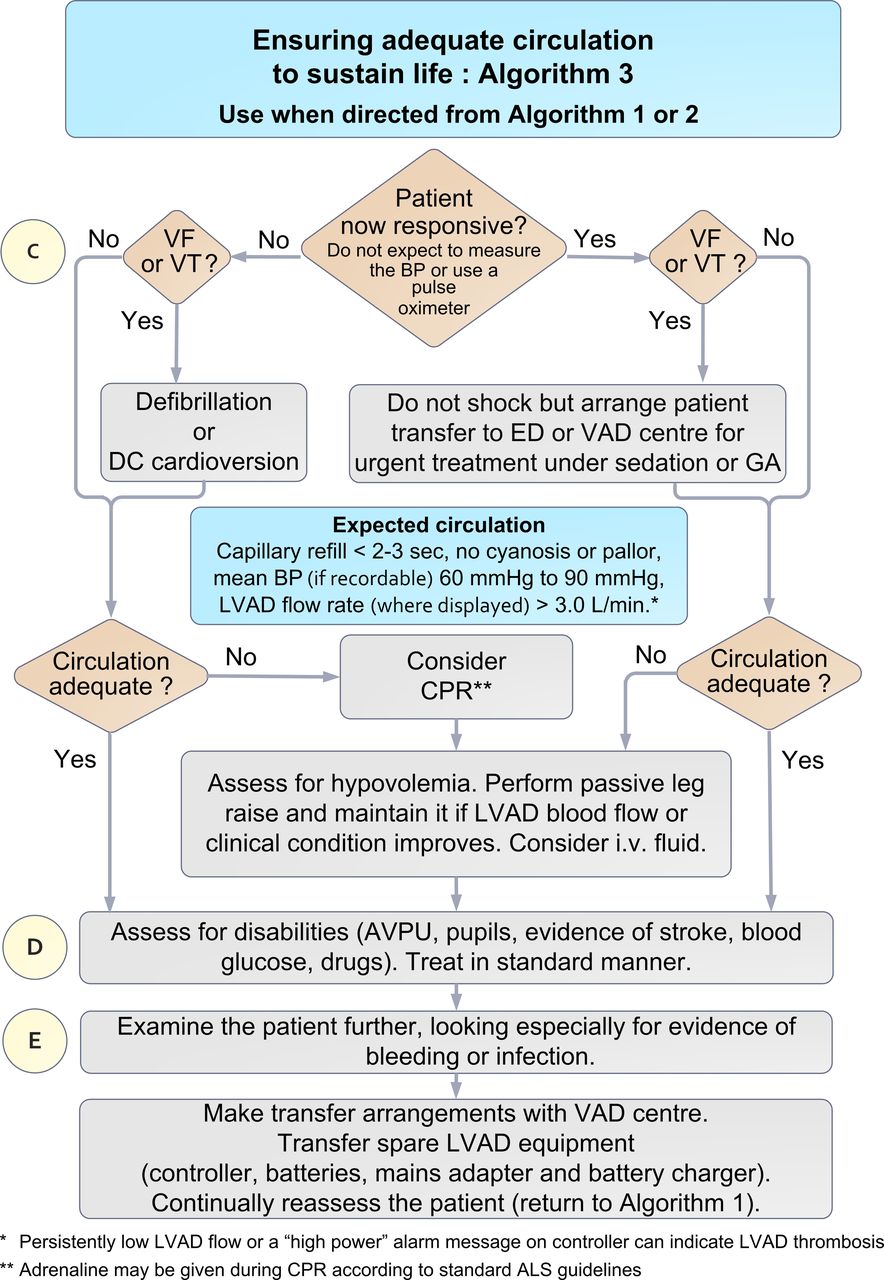
The most important and difficult aspect of LVAD management includes cardiac arrest. Cardiac arrest in an LVAD patient may occur due to device failure, or an alternative cause. As with any other cardiac arrest, compressions should be started immediately, and the LVAD team should be notified emergently as well. The ED team can proceed with standard ACLS protocol while also utilizing an echo to assess for ventricular function.
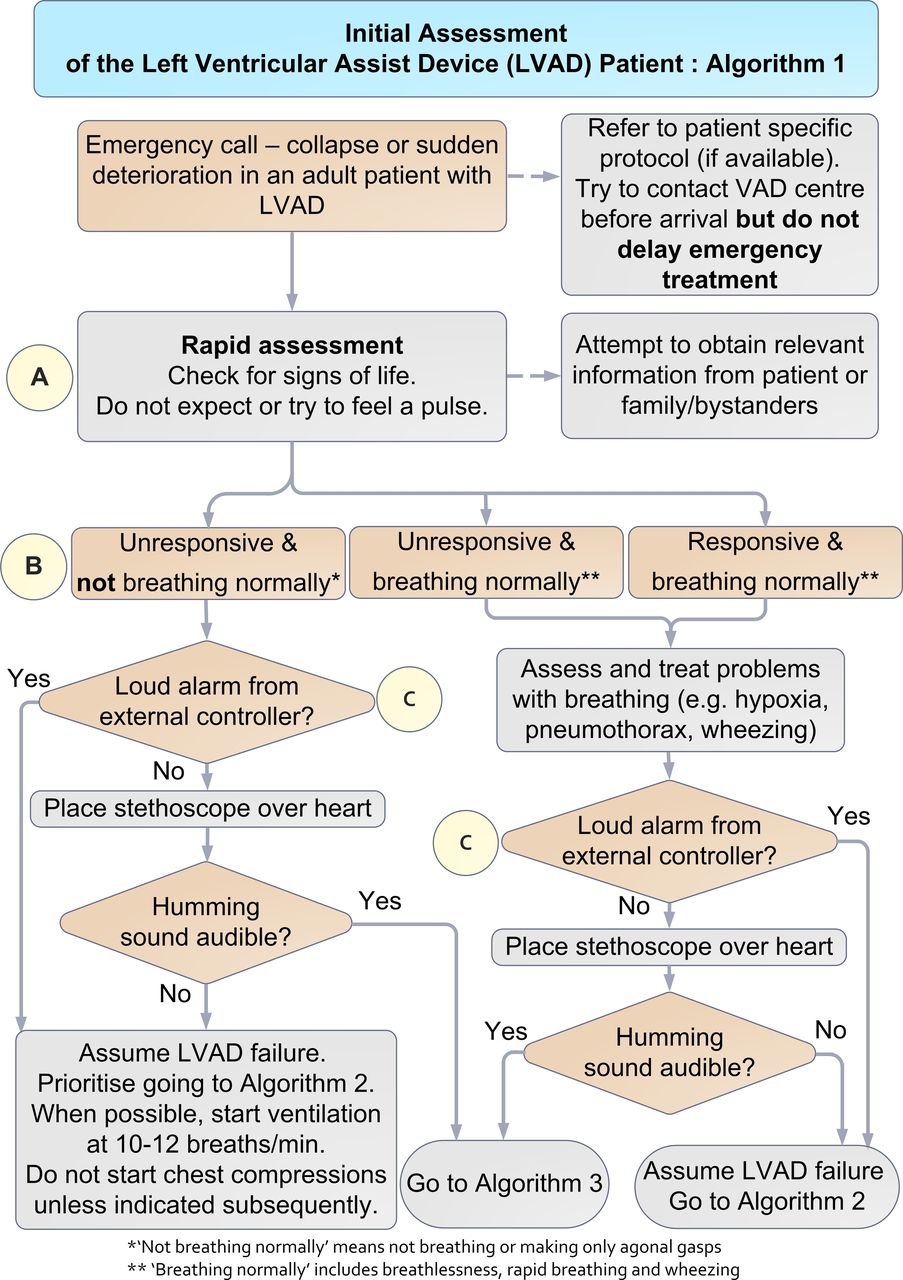
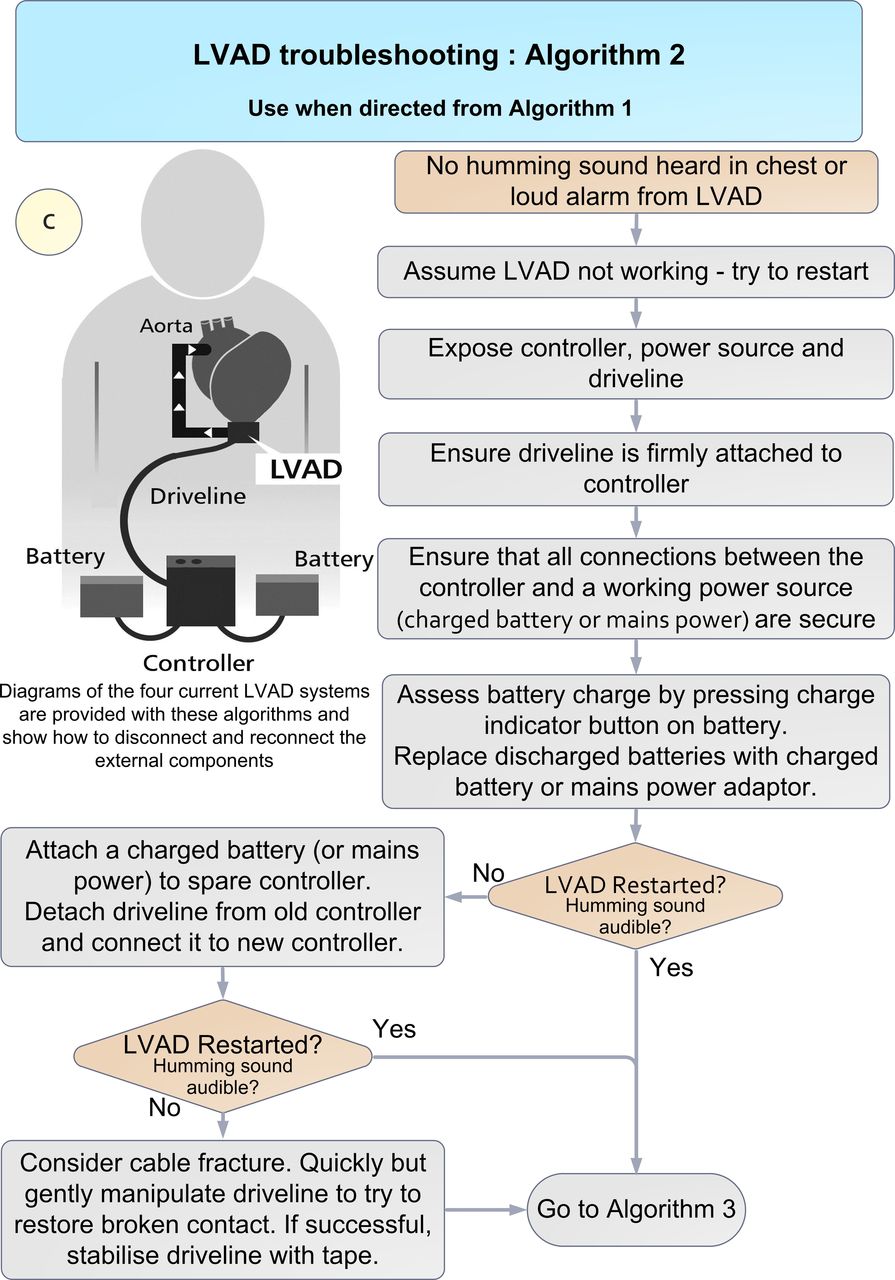
LVAD failure is the most important etiology of cardiac arrest that the ED physician should know how to manage. There are 3 reasons for possible LVAD failure: power, the controller, or driveline. One should check to make sure that all the external LVAD components are appropriately connected to a power source and consider manipulating the driveline. See the algorithms for a step-by-step approach to troubleshooting situations.
Algorithm 1-3. Initial assessment of LVAD patient and troubleshooting LVAD issues8
References
- Bozkurt B, Ahmad T, Alexander KM, et al., for Writing Committee Members. Heart Failure Epidemiology and Outcomes Statistics: A Report of the Heart Failure Society of America. J Card Fail. 2023;29(10):1412-1451.
- Stone ME, Pawale A, Ramakrishna H, Weiner MM. Implantable Left Ventricular Assist Device Therapy-Recent Advances and Outcomes. J Cardiothorac Vasc Anesth. 2018;32(4):2019-2028.
- Honasoge A, Hu KM. Emergency Department Evaluation and Management of Patients with Left Ventricular Assist Devices. Emerg Med Clin North Am. 2022;40(4):755-770.
- National Heart Lung and Blood Institute (NIH). Figure A shows the location of the heart and the typical equipment needed for an implantable LVAD. Figure B shows how the LVAD is connected to the heart. 2013;21:41:16. Public domain, via Wikimedia Commons.
- Englert JAR, Davis JA, Krim SR. Mechanical Circulatory Support for the Failing Heart: Continuous-Flow Left Ventricular Assist Devices. Ochsner J. 2016;16(3):263-269.
- Hockstein MA. Continuous-flow left ventricular assist devices: Management in the emergency department. J Am Coll Emerg Physicians Open. 2020;1(4):362-370.
- Kilic A, Acker MA, Atluri P. Dealing with surgical left ventricular assist device complications. J Thorac Dis. 2015;7(12):2158-2164.
- Bowles CT, Hards R, Wrightson N, et al. Algorithms to guide ambulance clinicians in the management of emergencies in patients with implanted rotary left ventricular assist devices. Emerg Med J. 2017;34(12):842-850.