Occlusion of the Artery of Percheron leading to isolated bilateral thalamic infarcts is a rare and difficult diagnosis in emergency medicine. Learn the symptoms that can help keep it top of mind.
Case
A 34-year-old male presents to the emergency department with the complaint of syncope. His only relevant known medical history is hypertension, and family states that about an hour prior to arrival, he was standing on his porch when he had a syncopal episode. His vital signs are normal except for slightly elevated blood pressure, and his exam reveals no signs of trauma. His neurologic exam demonstrates bilateral ptosis and a decreased level of arousal, though the family notes he had several beers prior to passing out. You figure he may just be intoxicated and sleepy, so you plan for typical syncope-plus-head trauma orders while you let him metabolize his beers. At this time, his family member mentions that he has had a mechanical heart valve since childhood for an unknown reason and does not take his warfarin.
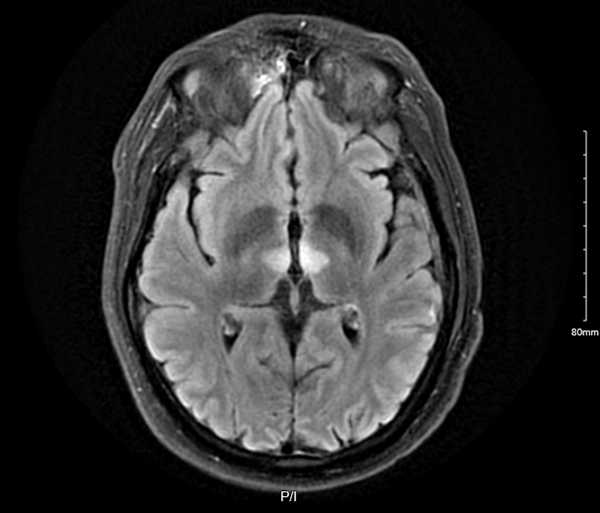
His presentation of acute encephalopathy, now in the setting of a significant risk factor, prompts you to consult neurology for concern of possible stroke. The CT head and angiogram are unremarkable, but an MRI is subsequently obtained and shows acute, isolated infarcts of the bilateral thalami. The neurologists question you on how this patient’s presentation correlates to the imaging findings.
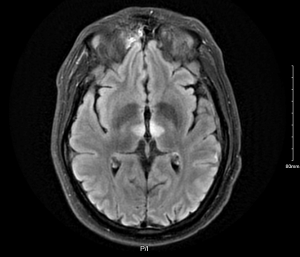
Figure 1. Imaging reveals acute, isolated infarcts of the bilateral thalami
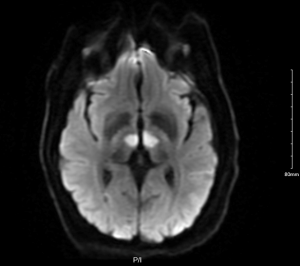
Figure 2. Imaging reveals acute, isolated infarcts of the bilateral thalami
Differential
While the differential for acute encephalopathy is broad, the differential for sudden-onset depressed mental status is conveniently narrower. Common causes include: traumatic brain injury; neurovascular pathology such as thromboembolic events and hemorrhage; seizure, particularly nonconvulsive status epilepticus, or a postictal state; intoxication from alcohol, opiates, benzodiazepines, etc.; and hypoglycemia.1 This is in contrast to a slowly developing encephalopathy that would be expected with etiologies such as infection, certain electrolyte disturbances such as hypercalcemia, or endocrine pathology,2 where the likely clinical course would be several days of symptoms leading to a progressively developing encephalopathy that finally prompts presentation to the emergency department. Few of these would be likely in this patient’s case. His immediate presentation rules out anything more indolent, and his history, exam, vitals, and CT make an acute ischemic event one of the more likely etiologies.
Regarding the findings on the patient’s MRI, bilateral thalamic infarction has a limited differential. It would, logically enough, need to occur in the setting of a symmetric process such that the typical unilateral thromboembolic infarct that we are taught to think of with a subcortical lesion is not enough to explain the bilaterality. A basilar artery infarct or cerebral venous sinus thrombosis could theoretically cause these findings, though these are much more likely to be asymmetric and affect additional vascular territories. Non-vascular lesions of the bilateral thalami include Wernicke's encephalopathy, Wilson’s disease, Creutzfeldt-Jakob disease, osmotic myelinolysis, and bilateral malignancies,3,8 though these all have their own history and associated findings that make them unlikely in this case and, again, would not occur as rapidly as in this patient. One relatively unknown pathology that could be responsible for this patient’s acute encephalopathy and his surprising MRI finding is infarction via the Artery of Percheron.
Artery of Percheron
The Artery of Percheron is a rare anatomical variant of vascular supply to the thalami. Normal vascular supply is through the posterior cerebral artery (PCA) just as it branches off from the basilar artery, where both PCAs send off perforating arteries that supply their respective thalamus.4,5 The Artery of Percheron is a variant where the perforating arteries to both thalami (the paramedian segment specifically) arise from a single arterial trunk that comes off only one PCA6,7 and are in the same vascular territory. This anatomy explains how a single embolic event can infarct such specific bilateral structures without involving broader vascular territories as would be expected in a larger basilar artery infarct.
Thalamus
The thalamus is a gray matter structure above the midbrain and beneath the lateral ventricles. It is composed of many different nuclei, and the various nuclei serve as the relay centers for sensory information coming back to the brain or for motor information going out to the body. It is also part of the reticular activating system that regulates consciousness and wakefulness, and it plays a role in cognition and behavior. Thus, infarcts to the thalamus can present with a wide range of deficits depending on an individual’s vascular supply and the specific nuclei involved. The paramedian thalamic infarcts from Artery of Percheron occlusion are likely to display deficits in oculomotor function, language, and consciousness.8 This patient, with his low level of arousal and bilateral ptosis, had neurologic findings consistent with thalamic infarct.
Clinical Pearls
Occlusion of the Artery of Percheron leading to isolated bilateral thalamic infarcts is a rare event. Its presence is mainly isolated to case reports in the neurology literature, and no emergency medicine resource appears to make mention of its existence. This is a rare and difficult diagnosis that typically requires MRI for definitive diagnosis. Vigilance is needed to identify the potential of this stroke pattern in patients with altered mental status and few other findings. The prompt recognition of this rare etiology of stroke in a patient with unresolving encephalopathy led to early enough diagnosis for therapeutic intervention.
Case Resolution
The patient had an unremarkable hospital course. He was given tenecteplase due to his presentation within the thrombolytic window and was appropriately anticoagulated for his mechanical valve. Over the subsequent days his level of alertness improved with modafinil, though at the time of his discharge he still had some degree of ptosis and required frequent verbal or physical stimuli to remain fully alert and awake.
Notably, the prognosis for thalamic stroke is considered favorable, though recovery from deficits in level of arousal and behavioral changes have been reported to be worse compared to motor or sensory deficits.3
References
- Traub SJ, Wijdicks EF. Initial Diagnosis and Management of Coma. Emerg Med Clin North Am. 2016;34(4):777-793.
- Karpenko A, Keegan J. Diagnosis of Coma. Emerg Med Clin North Am. 2021;39(1):155-172.
- Bhattarai HB, Dahal SR, Uprety M, et al. Bilateral thalamic infarct involving artery of Percheron: a case report. Ann Med Surg (Lond). 2023;85(9):4613-4618.
- Caruso P, Manganotti P, Moretti R. Complex neurological symptoms in bilateral thalamic stroke due to Percheron artery occlusion. Vasc Health Risk Manag. 2016;13:11-14. Published 2016 Dec 22.
- Mujeeb S, Bruh SR, Elsamaloty H, Colyer WR. Symmetric Bilateral Thalamic Infarcts: A Rare Complication of Cardiac Catheterization. Int J Cardiol. 2008; 7(1).
- Donohoe C, Nia NK, Carey P, Vemulapalli V. Artery of Percheron Infarction: A Case Report of Bilateral Thalamic Stroke Presenting with Acute Encephalopathy. Case Rep Neurol Med. 2022;2022:8385841.
- Garcia-Grimshaw MA, Peschard-Franco M, Gutierrez-Manjarrez FA. Bilateral Thalamic Ischemic Stroke Secondary to Occlusion of the Artery of Percheron. Cureus. 2018;10(5):e2676.
- Rodriguez EG, Lee JA. Bilateral thalamic infarcts due to occlusion of the Artery of Percheron and discussion of the differential diagnosis of bilateral thalamic lesions. J Radiol Case Rep. 2013;7(7):7-14.