Epinephrine is a commonly administered vasopressor in cardiac arrests. Does the evidence support this intervention?
According to the most recent data from the 2016 Cardiac Arrest Registry to Enhance Survival (CARES) database, roughly about 60,000 adults presented as non-traumatic Outside-of-Hospital Cardiac Arrest (OHCA). Of these individuals, 29% survived to hospital admission, 10.8% survived to hospital discharge, 9% survived with a Cerebral Performance Index (CPC) score of 1 or 2 indicating good neurologic outcome, and 62.8% suffered in-hospital mortality.
Many factors affect the return of spontaneous circulation (ROSC) and neurologically meaningful recovery in individuals suffering from cardiac arrest. It has been previously established that quality of chest compressions, uninterrupted continuous compression, and early defibrillation in V-fib/V-tach arrests improve the ability to achieve ROSC. However, other interventions we routinely perform in cardiac arrest resuscitation, such as administration of vasopressor and advanced airway, are not backed up by strong evidence.
Epinephrine is a commonly administered vasopressor in cardiac arrests. Epinephrine is a nonselective alpha and beta agonist. It exerts chronotropy and inotropy effects via alpha 1 and beta receptors. Alpha 1 receptor activation can cause coronary vasoconstriction, while beta receptor activation can cause coronary artery vasodilation. Although the chronotropy and inotropy provided by epinephrine are in theory beneficial to a patient in cardiac arrest, research has shown that the alpha 1 mediated vasoconstriction is what truly benefits these patients by driving up the coronary perfusion pressure (Aortic Diastolic Pressure - Right Atrial Pressure). However, epinephrine is not without its adverse effects. The chronotropy and inotropy also increases the myocardial oxygen demand and by nature it can lead to ventricular arrhythmias. Just as we use albuterol to temporize our hyperkalemic patients, through action at the beta receptors, epinephrine can lead to hypokalemia. The vasoconstrictive effects on microcirculation can lead to complete occlusion and end organ ischemia. It has even been theorized that epinephrine can lead to platelet aggregation, further limiting, rather than improving, perfusion. Yet, epinephrine remains our primary vasopressor in cardiac resuscitation.
In the late 1800s, many researchers and scientists studied and published the physiology of epinephrine as an adrenal extract. A landmark study on epinephrine and cardiac arrest in dogs by Crile and Doyle was published in 1906. In 1974, the first ACLS guidelines were published, and many studies reviewing the guidelines have since been published.
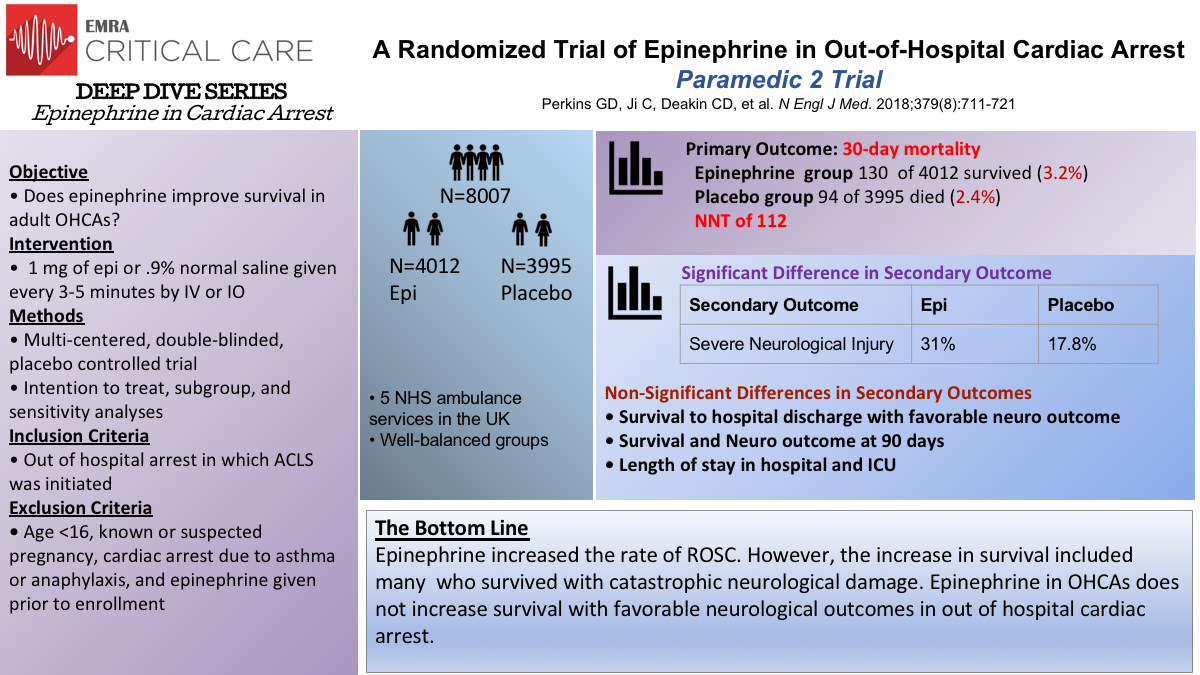
PARAMEDIC 2
The PARAMEDIC 2 trial, published in 2018, was a randomized double blinded study in the United Kingdom of patients with OHCA who either received standard parenteral epinephrine or saline placebo and standard care. They found that at 30 days, 3.2% of patients who received epinephrine vs. 2.4% of patients who received placebo were alive. Although 30 day survival was significantly different between epinephrine and placebo, there was no significant difference in neurologically intact survival.
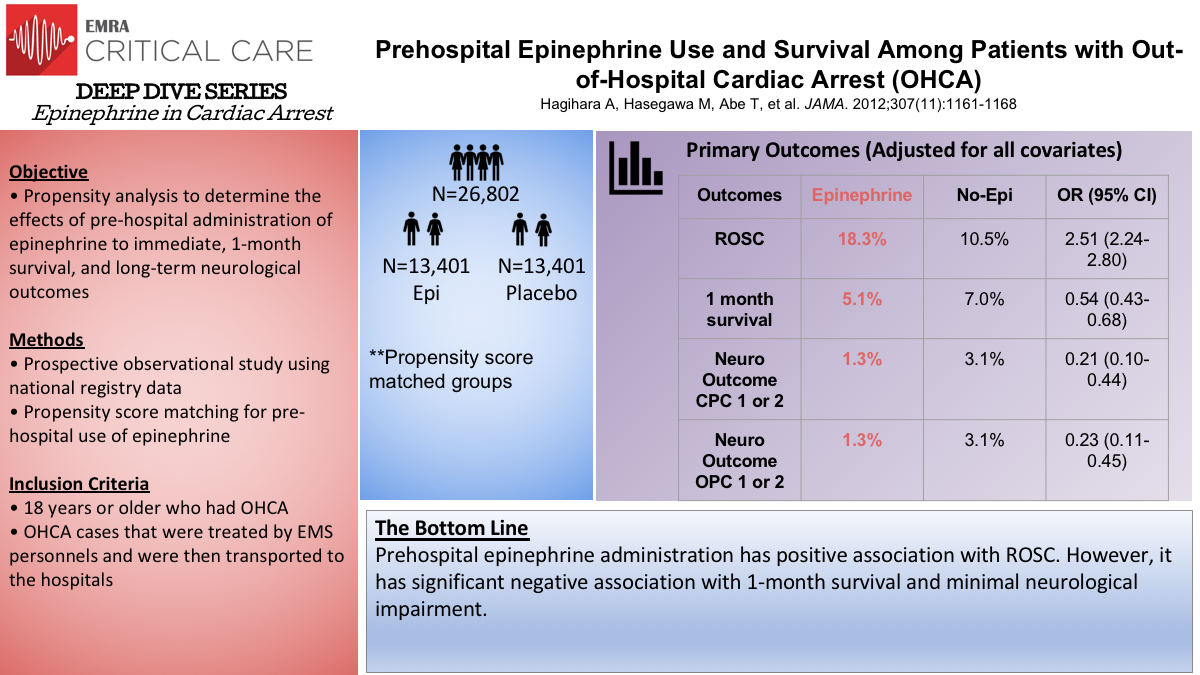
Epi in OHCA: Hagihara et al.
A prospective, non-randomized observational study from Japan by Hagihara et al., compared prehospital epinephrine administration to standard resuscitation without epinephrine. Only recently were Japanese paramedics allowed to place IVs (2004) and administer epinephrine (2006). The authors compared pre- and post-2006 cohorts and performed propensity score matching. In this study, 18.5% of patients who received epinephrine achieved ROSC vs 5.7% who did not receive epinephrine. However, the number of patients with meaningful neurologic survival at 1 month was 1.4% in the epinephrine arm and 2.2% in the no epinephrine arm. Similar to the PARAMEDIC 2 trial, epinephrine increased ROSC but negatively impacted meaningful neurologic survivability.
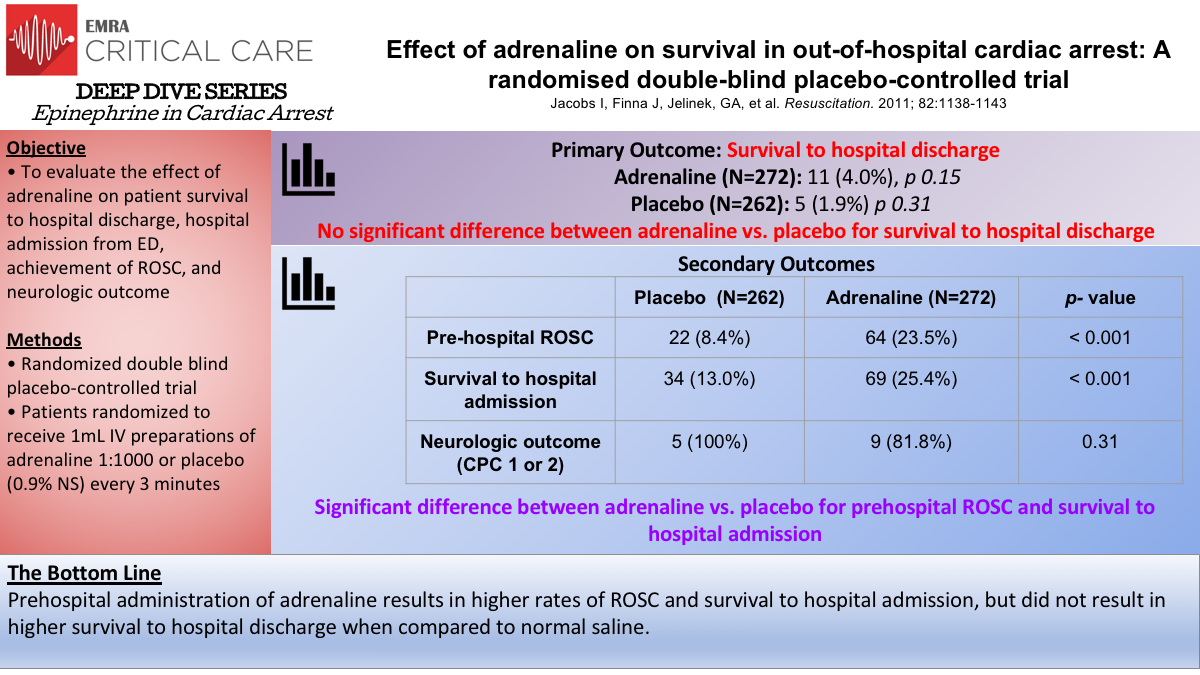
Epi in OHCA: Jacobs et al.
Similarly, the Jacobs trial from 2011, was a double blind randomized placebo controlled trial in Western Australia, comparing 1 mL aliquots of 1:1000 epinephrine to 1 mL aliquots Normal Saline placebo. In this study, 23.5% of patients receiving epinephrine achieved ROSC vs 8.4% of patients receiving placebo. Survival to hospital discharge was 4.0% in epinephrine group vs 1.9% in the placebo group. Of these patients, all but 2 in the epinephrine group, had neurologically meaningful survival.
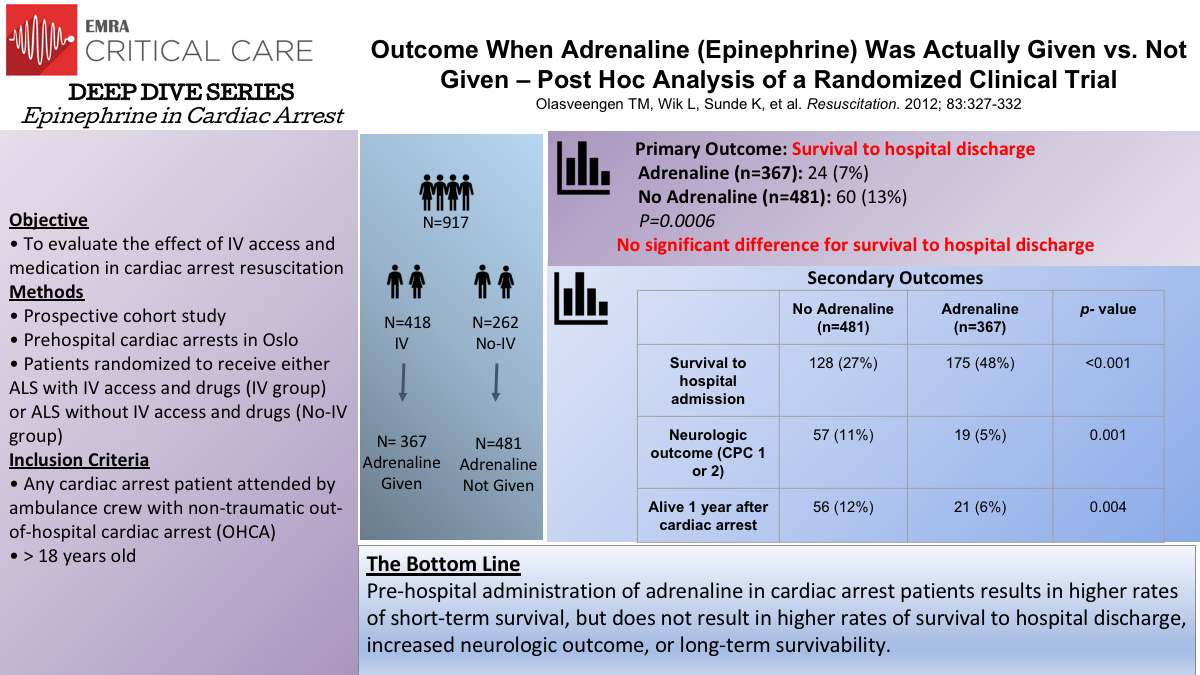
Post-hoc Analysis: Olasveengen et al.
In a Norwegian study by Olasveengen et al., a post hoc analysis was completed on patients from a prior study. Achievement of ROSC was analyzed in patients who received epinephrine vs those who did not receive epinephrine. These groups were further subdivided into presenting rhythms: shockable vs non-shockable rhythms (V-fib or pulseless V-tach vs PEA or asystole). Although more patients in the epinephrine group were more likely to be admitted to the hospital, patients in the epinephrine group were less likely to be discharged from the hospital and less likely to be discharged with favorable neurologic outcome. However, results were confounded by the observation that patients in the epinephrine group were more likely to be defibrillated and intubated as well as to receive longer resuscitative efforts.
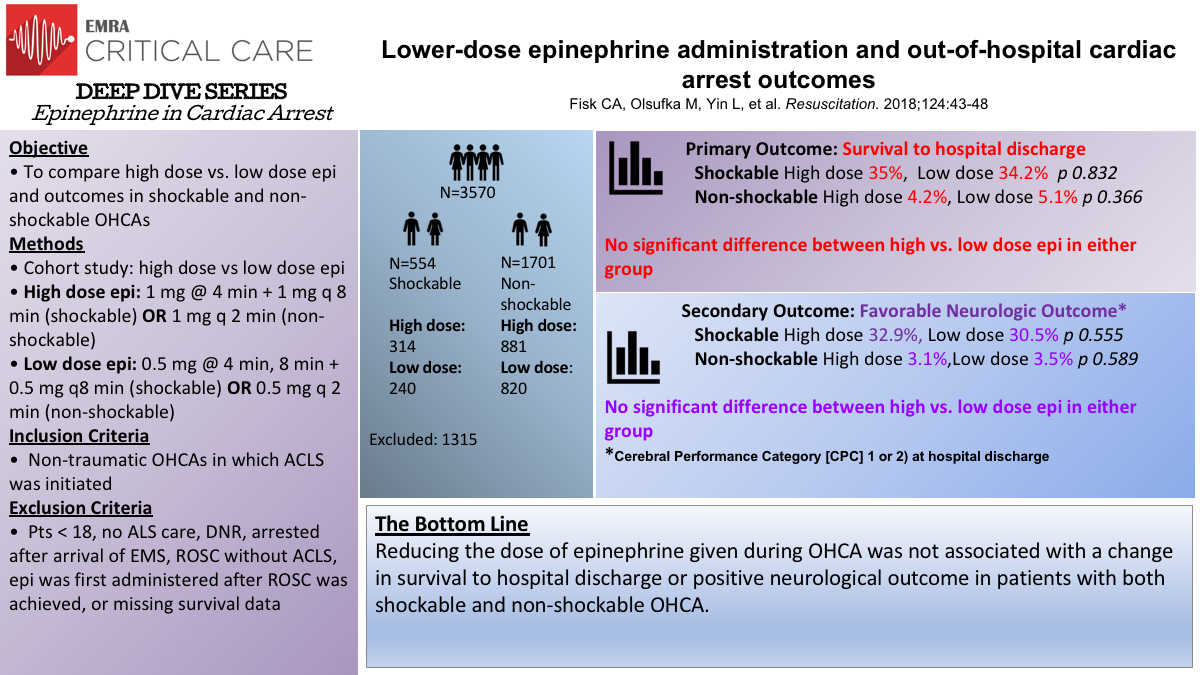
Lower-Dose Epi: Fisk et al.
A study by Fisk et al. looked into whether a lower dose of epinephrine (0.5 mg) would improve neurologic outcome and survival to discharge compared to the standard 1 mg IV epinephrine dose in non-traumatic OHCA cases. The 1 mg higher dose was given for the first 4 years of the study. In 2012, 0.5 mg was given instead of 1 mg, but at the same time intervals depending on the rhythm. The study was subdivided into shockable vs non-shockable rhythm. For those with a shockable rhythm, survival to hospital discharge was 35% in the higher dose group vs 34.2% in the lower dose group. For those with a non-shockable rhythm, survival was 4.2% in the higher dose vs 5.1% in the lower dose group. It was concluded that lower dose epinephrine neither improved favorable neurologic outcome nor improved survival to discharge.
A recent systematic review and meta-analysis published this year compared epinephrine to placebo in cardiac arrest. Kempton et al. included 5 randomized controlled trials (RCTs). The primary outcome was survival to hospital discharge, with achievement of ROSC being a secondary outcome. Both the Jacobs and Olasveengen study were included in this review. The review concluded that the use of epinephrine in OHCA increased ROSC and survival to hospital admission. However, epinephrine did not improve neurological outcome. It also did not increase the rate of survival to discharge.
While epinephrine use has been shown to increase the chance of ROSC in OHCA, it has not been shown to improve survival to hospital discharge nor neurologic outcome. It is important to recognize that these studies do not necessarily conclude that epinephrine should not be used in cardiac arrest. Rather, they should drive us to further research ways to improve our management of cardiac arrest.
Physiologic approach to cardiac arrest has increasingly been driving practice changes and developing cutting edge methods in resuscitation medicine. Furthermore, we should also consider the ethical question of whether we should emphasize more on neurological outcomes in OHCA cases. Perhaps the importance of these studies is to remind us to step outside of the protocol and to consider individualizing our management approach. Therefore taking us back to the physiology and challenging us to do away with an algorithm that has simplified our management strategy for over 50 years.
References
Fisk CA, Olsufka M, Yin L, et al. Lower Dose Epinephrine Administration and Out Of Hospital Cardiac Arrest Outcomes. Resuscitation. 2018;124:43-48.
Hagihara A, Hasegawa M, Abe T, et al. Prehospital Epinephrine Use and Survival Among Patients with Out-of-Hospital Cardiac Arrest (OHCA). JAMA. 2012;307(11):1161-1168.
Jacobs I, Finna J, Jelinek, GA, et al. Effect of Adrenaline on Survival in Out Of Hospital Cardiac Arrest: A randomised double blind placebo controlled trial. Resuscitation. 2011; 82:1138-1143.
Kempton H, Vlok R, Thang C, et al. Standard Dose Epinephrine versus Placebo in Out of Hospital Cardiac Arrest: A Systematic Review and Meta Analysis. Am J Emerg Med. 2019; 37(3):511-517.
Olasveengen TM, Wik L, Sunde K, et al. Outcome When Adrenaline (Epinephrine) Was Actually Given Vs. Not Given - post hoc analysis of a randomized clinical trial. Resuscitation. 2012; 83:327-332.
Perkins GD, Ji C, Deakin CD, et al. A Randomized Trial of Epinephrine in Out Of Hospital Cardiac Arrest. N Engl J Med. 2018;379(8):711-721.
AHA Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics – 2018 Update. Circulation. 2018;137:e67-e492.
Farkas J. 2015 ACLS Guidelines: What happened to VSE? PulmCrit (EMCrit). Oct. 25, 2015.
Attaran RR, Ewy GA. Epinephrine in resuscitation: curse or cure? Future Cardiology. 2010;6(4).