Pneumocephalus, or the presence of air in the brain cavity, is an uncommon but potentially fatal condition that must be evaluated and treated right away in the ED. Air accumulation under pressure within the skull cavity can result in tension pneumocephalus, which may require emergency surgery. This complication may be brought on by injuries, surgeries, or, less frequently, infections or neoplasms that affect the paranasal sinuses or skull.
Health-care personnel caring for patients after head trauma or neurosurgical procedures must be knowledgeable about the causes, clinical manifestations, diagnostic techniques, and management approaches of tension pneumocephalus.
Case
We present a case of a 48-year-old male with past medical history of hypertension and Rathke's cleft cyst. The patient, post-transsphenoidal resection approximately 4 weeks prior, presented to the ED for evaluation of left lower extremity weakness, a symptom he noted he had not had before that day. The patient noted that these symptoms started approximately 3 to 4 hours prior to presentation. He noted that his left leg felt “heavy.” His symptoms were associated with 10/10 headache, nausea, and 2 episodes of non-bilious, non-bloody vomiting.
The patient’s family also noted a change in his mental status, noting he had been increasingly confused over the past week, although there were no signs of slurred speech. Of note, the patient stated his post-op course was complicated by rhinorrhea and diabetes insipidus. He was readmitted to the hospital 2 weeks after the procedure and was diagnosed with a CSF leak; a procedure to stem the leak was performed. Otherwise, he had no history of head trauma, syncope, seizure-like activity, or stroke.
Physical exam revealed a patient who was alert and awake in moderate distress, and seemingly mildly confused. Vital signs were remarkable for BP of 144/100mmHg and HR of 102bpm. The rest of the patient’s vital signs were unremarkable. They included RR of 20 bpm, oxygen saturation of 100% on room air, and temperature of 97.2. The patient’s cardiac and pulmonary exams were within normal limits. His neurological exam was significant for an NIHSS of 1 due to his left leg drift, intact extraocular movement with no visual deficits, gaze preference, facial drooping, tongue deviation, with intact and equal sensation throughout.
Laboratory findings on the CBC, inflammatory markers, and urinalysis were noted as WBC of 24,500 per microliter (4,800–10,800 per microliter), neutrophile count of 88% (36-66%), and ESR and CRP of 3 millimeters per hour (0–20 millimeter per hour) and 18.7 milligrams per liter (0–3 milligrams per liter), respectively. Coagulation panel showed a PT of 10.3 with an INR of 0.88 and a PTT of 25.6. The electrolyte panel was noted for sodium-139, potassium-3.3, and glucose-108. Urinalysis was remarkable for a WBC of 0-5/HPF and an RBC of 0-5/HPF. It also contained no bacteria.
The patient was noted to have extensive pneumocephalus throughout the subdural and subarachnoid space, and prominent right-sided subdural pneumocephalus resulting in the leftward mass effect with leftward sub-falcine herniation, with no intracranial hemorrhage.
Due to imaging findings and the patient’s presentation, which included signs of elevated intracranial pressure, management of the patient required neurosurgical intervention. The case was discussed with the patient’s neurosurgical team. They noted pneumocephalus is a complication of neurosurgical procedures and advised that the patient be transferred to their facility for continued management.
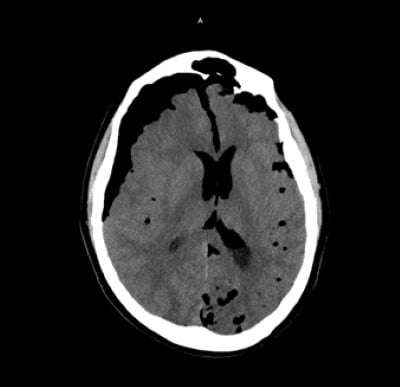
Image 1
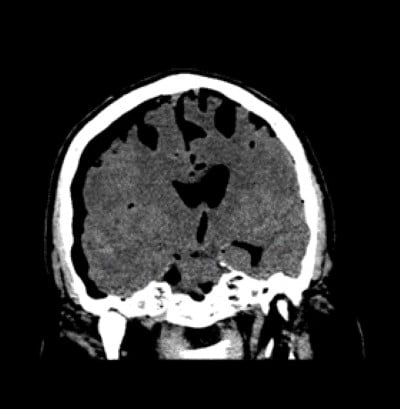
Image 2
Prior to transfer, the patient was placed on high-flow oxygen, given antiemetics, and provided with other interventions that were noted to improve symptoms. During the patient’s admission, the team initially opted for conservative management. However, after approximately 36 hours, repeat imaging showed no decrease in pneumocephalus and revealed a suprasellar/skull base defect. This finding prompted an endoscopic endonasal transsphenoidal approach for repair of suprasellar/skull base defect using naso-septal flap. The patient was discharged home 2 weeks after the procedure with no further complications.
Discussion
Tension pneumocephalus is difficult to diagnose and treat; therefore, a thorough understanding of its cause, clinical manifestation, and management is required. Although this complication is uncommon, it is important for emergency physicians to maintain a high index of suspicion when evaluating patients who have recently undergone neurosurgical procedures, have a history of head trauma, or have had sinus surgery.
Reducing intracranial pressure quickly is the main objective in the management of tension pneumocephalus in order to stop further neurological damage. Early patient stabilization is greatly aided by non-invasive techniques like oxygen delivery and head elevation. By producing a concentration gradient that favors the passage of nitrogen out of the cranial cavity, high-flow oxygen treatment aids in the resorption of intracranial air.
Surgery, such as craniotomies and burr holes, is frequently required to release trapped air and treat the underlying cause of tension pneumocephalus. Depending on the site and severity of pneumocephalus, neurosurgical competence is crucial in choosing the best surgical strategy. The particular clinical situation will determine if burr holes or craniotomies are the best option. A careful risk-benefit analysis is crucial.
It is impossible to overestimate the importance of imaging in the diagnosis and treatment of tension pneumocephalus. When it comes to locating and diagnosing intracranial air, CT scans continue to be the gold standard, offering vital information for surgical planning. Even while MRI might provide more information, particularly in situations involving soft-tissue pathology, it is typically regarded as secondary to CT in the acute context.
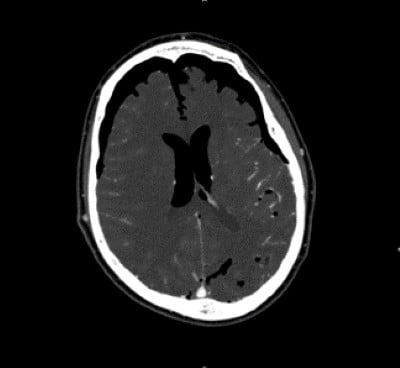
Image 3
A comprehensive approach to patient care is necessary to minimize long-term consequences and prevent complications. If tension pneumocephalus results from trauma, concurrent injuries need to be treated right away. In addition, treating any underlying infections or leaks of CSF fluid is critical to avoiding recurrent pneumocephalus.
Tension pneumocephalus continues to be linked to a considerable rate of morbidity and mortality, even with improvements in diagnostic techniques and treatments. In some instances, neurological effects such as localized neurological dysfunction and cognitive deficiencies may not go away. Thus, rehabilitation and long-term follow-up are essential elements of the total care plan.
Conclusion
Tension pneumocephalus is an uncommon but sometimes fatal complication of head injuries, brain surgeries, or sinus surgeries. Neurological decline must be avoided in order to maximize patient outcomes, and prompt diagnosis and treatment are crucial. Management of tension pneumocephalus necessitates a multidisciplinary strategy that includes imaging tests, critical care management, and neurosurgery experience.
Further investigation into enhanced methods of diagnosis, approaches to therapy, and long-term prognosis is essential to improving our comprehension of tension pneumocephalus. Health-care practitioners must keep an open mind and maintain a high index of suspicion for tension pneumocephalus in pertinent clinical circumstances as our understanding of the condition advances. Further cooperation between researchers and physicians will improve our capacity to identify, treat, and eventually avoid tension pneumocephalus.
References
Lasoff DR, Wardi G, Sloane C. Mount Fuji Sign: Tension Pneumocephalus in the Emergency Department. J Emerg Med. 2019 Oct;57(4):569-570. doi: 10.1016/j.jemermed.2019.06.051. Epub 2019 Sep 24. PMID: 31561929.
Derakhshani A, Livingston S, William C, Lieberman S, Young M, Pacione D, Dehkharghani S. Spontaneous, Intrasphenoidal Rupture of Ecchordosis Physaliphora with Pneumocephalus Captured During Serial Imaging and Clinical Follow-Up: Pathoanatomic Features and Management. World Neurosurg. 2020 Sep;141:85-90. doi: 10.1016/j.wneu.2020.05.220. Epub 2020 May 31. PMID: 32492548.



