Want to contribute to our POCUS FTW series? Find out how.
piHPI: 51F, presents w/ 1 week of R hip pain
VS: T 36.4C HR 107 BP 136/87 RR 22 O2sat 100% RA
The patient is a 51-year-old female who reports 7 days of gradually worsening pain in her right hip that radiates down her leg. She denies any history of trauma or fall, and denies any clear aggravating or alleviating factors. On review of systems, the patient reports generalized malaise, fatigue, headache, and myalgias/chills. The patient has a history of hypertension and hyperthyroidism, and her only medication is methimazole. Her vitals are notable for mild tachycardia. Her physical exam is remarkable for a cold right foot without palpable pulses. A CT angiogram of her right leg demonstrates occlusions of her hepatic, splenic, superior mesenteric, right renal, and right femoral arteries, with infarcts of the bilateral kidneys, spleen, and liver. The patient’s labs are notable for platelets of 38.
On hospital day (HD) 1, the patient underwent a right lower extremity thrombectomy. Shortly after her procedure, the patient became hypotensive, lethargic, with newfound word-finding difficulty and right-sided weakness. The patient was intubated, and stroke imaging revealed multiple organizing infarcts with occlusions of her left ICA, MCA, and ACA vessels. Of note, a skin exam at that time showed a large left breast mass with an enlarged left axillary lymph node, which was concerning for breast cancer. The working diagnosis at this time was hypercoagulability secondary to Thrombotic Thrombocytopenic Purpura (TTP) due to the patient’s reported fevers and thrombocytopenia, versus hypercoagulability from an undiagnosed malignancy.
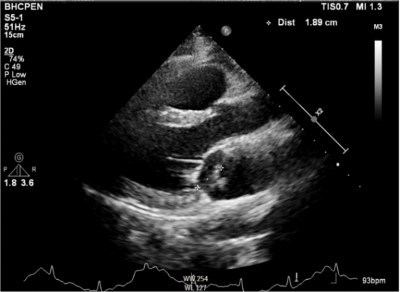
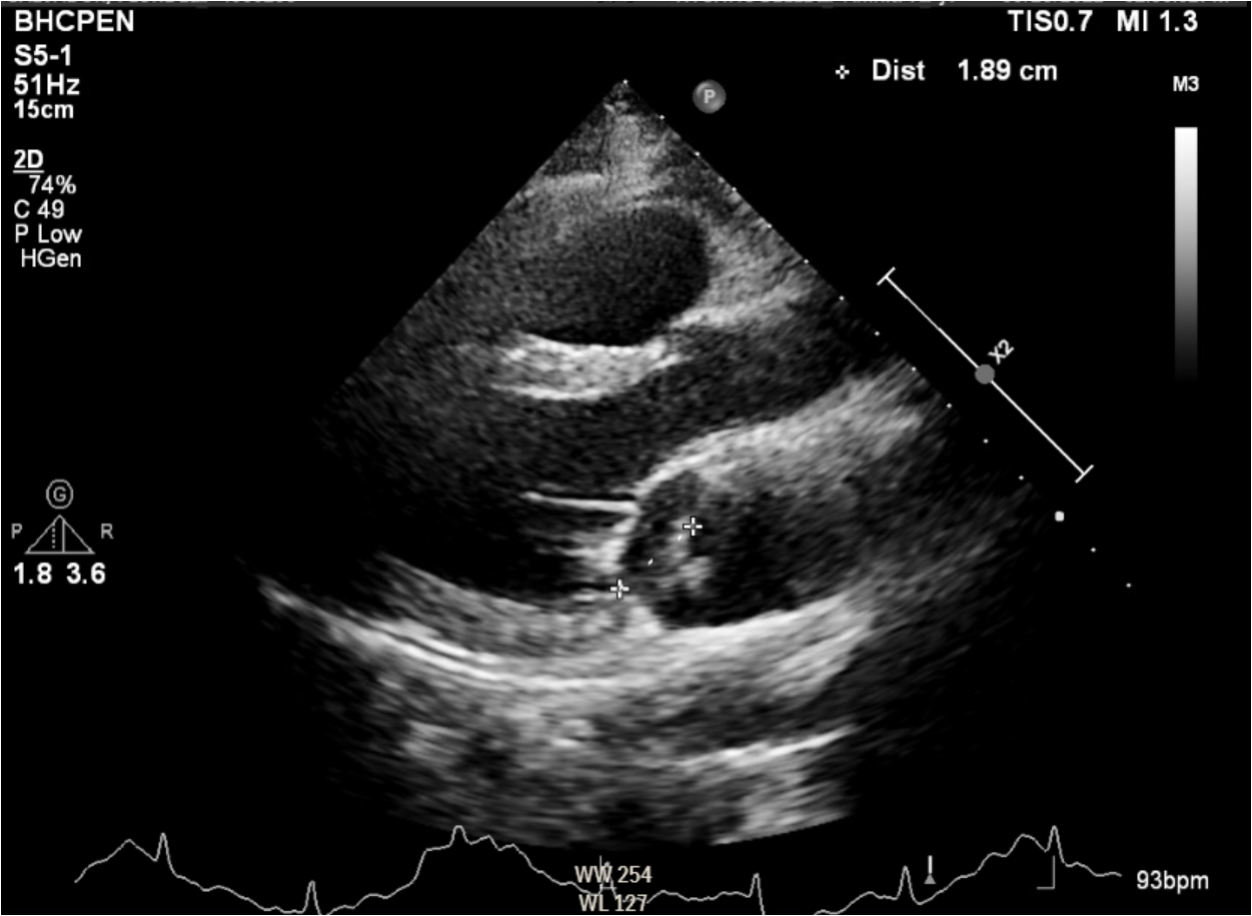
On HD 2, The patient developed a fever to 104.5 and was given broad-spectrum antibiotics. At this time, a transthoracic echocardiogram (TTE) was pursued (images below). The bedside TTE done by an emergency medicine resident in the CCU revealed a 1.9-cm vegetation adherent to the mitral valve as well as severe mitral regurgitation, suspicious for infective endocarditis.
Over the next several days, the patient’s vasopressor requirement improved, she was extubated, and her mental status improved as she became more interactive and able to respond to questions.
On HD 22, the patient underwent successful mitral valve replacement surgery. A biopsy of the patient’s breast mass revealed invasive ductal carcinoma of the breast, for which outpatient follow-up was arranged. On HD 37, the patient was discharged in stable condition to a stroke rehabilitation center.
Case discussion
Endocarditis is defined as an infection of the endocardial surface of the heart and most often refers to an infection of one or more of the heart valves. It is a difficult yet important diagnosis to make early in a patient’s course, as in the United States the in-hospital mortality rate is as high as 18-23%.1,2 Echocardiography is the main imaging modality used within Duke’s criteria to help diagnose endocarditis, and both the American Heart Association and the European Society of Cardiology recommend that a TTE be the initial step when infective endocarditis is first considered.3,4,5
This patient had a complicated medical course with a significant amount of initial diagnostic uncertainty, and her echocardiogram was not performed until after her acute change in mental status. The ED did well in recognizing a limb emergency in a patient who could have otherwise been initially perceived as low-acuity. Once several arterial thrombi with associated infarcts were found, some diagnostic anchoring occurred, with a focus on TTP and malignancy given the patient’s thrombocytopenia and breast mass. Endocarditis was not considered at this time given the patient did not have a documented fever and had no obvious risk factors for endocarditis.
To Probe or Not to Probe
Because endocarditis carries an exceptionally high in-hospital mortality rate, early diagnosis is instrumental in promoting good outcomes.1 An earlier consideration of endocarditis with bedside TTE in this patient could have resulted in earlier recognition and treatment.6 Patients with unexplained thrombotic events should therefore prompt consideration of septic emboli, and point-of-care echocardiography in the emergency department is a meaningful initial step in the evaluation of these patients. While even formal TTE only carries a sensitivity of up to 75%, it is a fast and cheap screening test, and positive findings can significantly expedite the diagnosis and treatment.
Limitations
While TTE is generally recommended as first-line imaging when endocarditis is suspected, it is only up to 75% sensitive, and cannot be used to rule out the diagnosis.7 If suspicion is high and TTE is non-diagnostic, a transesophageal echocardiogram (TEE) should be pursued.
References
1. Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falcó V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF, Utili R, Wang A, Woods CW, Cabell CH. International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) Investigators. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;5(5):463–473.
2. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Durack DT, Lukes AS, Bright DK. Am J Med. 1994;96(3):200.
3. Prendergast BD. Diagnosis of infective endocarditis. BMJ 2002; 325(7369):845–846.
4. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015; 36(44):3075–3128.
5. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2015; 132(15):1435–1486.
6. Seif D, Meeks A, Mailhot T, Perera P. Emergency department diagnosis of infective endocarditis using bedside emergency ultrasound. Crit Ultrasound J. 2013 Feb 11;5(1):1.
7. Recommendations for the practice of echocardiography in infective endocarditis. Habib G, Badano L, Tribouilloy C, Vilacosta I, Zamorano JL, Galderisi M, Voigt JU, Sicari R, Cosyns B, Fox K, Aakhus S, European Association of Echocardiography. Eur J Echocardiogr. 2010;11(2):202.