ARTICLE: Peter-Derex L, Philippeau F, Garnier P, et al. Safety and efficacy of prophylactic levetiracetam for prevention of epileptic seizures in the acute phase of intracerebral hemorrhage (PEACH): a randomized, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2022;21:781-791.
OBJECTIVE
To assess whether prophylactic levetiracetam would reduce the risk of early seizures in patients with intracerebral hemorrhage
BACKGROUND
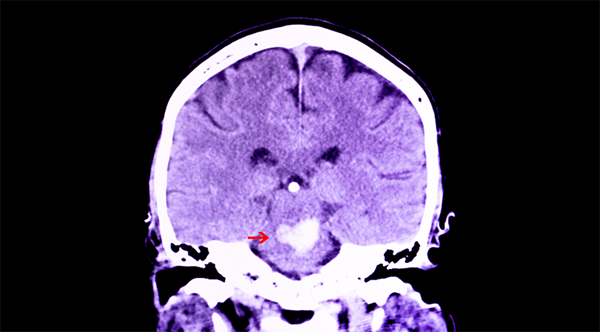
Spontaneous (non-traumatic) intracerebral hemorrhage (ICH) is associated with high patient morbidity and mortality. An early complication of the acute phase of ICH are epileptiform seizures, which occurs in up to 30% of patients when diagnosed with continuous EEG (cEEG).1 Seizures after ICH have been associated with worsening intracranial midline shift and worse functional outcomes.2 While it is the standard of care to reverse anticoagulation, there are no medical treatments for intracerebral hemorrhage that have proven to be beneficial.3 Current data regarding the efficacy of seizure prophylaxis has been controversial, with some studies suggesting that seizure prophylaxis after ICH prevents seizures4,5 while other studies have found lack of efficacy in seizure prophylaxis.6,7 As such, current clinical guidelines do not recommend the use of prophylactic antiseizure medication in acute ICH.
A more recent systematic review and meta-analysis of seizure prophylaxis following ICH found that seizure prophylaxis following ICH was not associated with seizure prevention in adults, but recommended additional analysis with randomized controlled trials in high-risk patients and with various antiepileptic drugs.8 This study attempts to fill this void in the literature.
METHOD AND DESIGN
Double-blind, randomized, placebo-controlled trial completed in the stroke units of one secondary and two tertiary hospitals in France. This study took place between June 1, 2017, and April 14, 2020, at which time recruitment was interrupted due to the COVID-19 pandemic and enrollment of the study was stopped due to cessation of funding.
Patients were randomly assigned (1:1) to receive levetiracetam or matching placebo. Participants, those involved in clinical care, and investigators were blinded to treatment allocation. The treatment group received levetiracetam 500 mg IV every 12 hrs for 48 hrs, then 500 mg every 12 hrs orally for 30 days followed by a 2-week taper (250 mg every 12 hrs for 7 days, then 250 mg daily for 7 days). The placebo group received a matching placebo dosed identically to the treatment group.
Continuous EEG was done within 24 hours of randomization and after treatment initiation for at least 48 hours.
Analysis for all outcomes, except for the safety analysis, was done according to a modified intention-to-treat principle (all patients who were randomly assigned to treatment and who had a cEEG performed). The safety analysis was performed in the intention-to-treat population.
Inclusion Criteria
- Adult patients, aged 18 years or older, with a spontaneous supratentorial ICH diagnosed by CT or MRI presenting within 24 hours of symptom onset
Exclusion Criteria
- NIHSS greater than 25
- ICH secondary to trauma, vascular malformation, hemorrhagic transformation of ischemic stroke, or tumor
- Current use of antiseizure drugs or history of epilepsy
- Pregnancy or breastfeeding
- Previous history of severe depression or psychotic disorder
- Known terminal illness
- Known allergy or hypersensitivity to levetiracetam
- The occurrence of an epileptic seizure between inclusion and initiation of treatment
Primary Outcome
- At least one clinical seizure within 72 hours of inclusion, or of at least one electrographic seizure recorded on cEEG
Secondary Outcomes
- The number of seizures, total duration of seizure, or occurrence of interictal paroxysmal patterns recorded on cEEG
- The number of clinical seizures within 72 hours, early (day 0 to day 30), and late (day 30 to 12 months) clinical seizures
- Change in NIHSS
- Change in modified Rankin Score (mRS)
- Quality of life assessed by the Stroke Impact Scale
- Change in intracerebral hemorrhage volume and mass effect as defined as midline shift at 72 hours
- Secondary safety outcomes (frequency of side effects related to treatment, anxiety and depression evaluated with the Hospital Anxiety and Depression Scale, and all-cause mortality)
RESULTS
Fifty patients were enrolled; 24 were assigned to the levetiracetam group and 26 were assigned to the placebo group. However, 19 patients assigned to the treatment group and 23 patients assigned to the placebo group were included in statistical analysis. There were significant baseline differences between the two groups. Participants randomized to the treatment group were older, more likely to have diabetes or hypertension, more were on anticoagulation before ICH, and had a higher prestrike mRS compared to participants randomized to the placebo group. The ICH location was more often lobular and baseline volume was lower in the treatment group.
Primary Outcome
There was a statistically significant difference between groups, as only 3 of 19 patients (16%) of the treatment group had electrographic seizures compared to 10 of 23 patients (43%) in the placebo group (OR 0.16, 95% CI 0.03-0.94, p=0.043).
Secondary Outcomes
The treatment group had fewer seizures during 48 hours cEEG (rate ratio 0.07, 95% CI 0.01-0.38; P=0.0021) and shorter median duration of seizures (67 s [IQR 46-300] vs. 780 s [IQR 380-1980]; p=0.028) compared to placebo group, which was statistically significant. No other differences in secondary outcomes were statistically significant.
LIMITATIONS
- Recruitment was prematurely interrupted after a total of 50 patients out of 104 planned had been included due to cessation of funding, therefore the study was underpowered, and any conclusions must be interpreted with caution. This limitation may also have limited the authors’ ability to demonstrate the effect of prophylactic levetiracetam on functional outcomes.
- Due to the small sample size, there were multiple differences in the baseline characteristics between the two groups as mentioned in the results section. This makes it very difficult to determine if the difference in outcomes is due to the intervention or to underlying differences between the groups.
- The imaging modalities on admission and at 72 hours follow-up were not standardized (CT scan or MRI were performed at the discretion of the treating clinician).
- No combined video monitoring was performed with cEEG, so no data are available about potential subtle clinical manifestations during electrographic seizures
- cEEG was recorded for 48 hours, so subclinical seizures before or after recording cannot be excluded
- Levetiracetam dosing was not adjusted for age, weight, or additional medication and serum concentrations were not analyzed, so dosing may not have been adequate to suppress seizures in the treatment group
- Results pertain to patients with mild to moderate ICH and may not be generalizable to patients with severe ICH
EM TAKE-AWAYS
While this study did find a statistically significant difference in the number and duration of seizures between treatment and placebo groups, these seizures were only identified on cEEG. It is unclear whether these acute subclinical seizures are clinically relevant and affect long-term outcomes. Interestingly, the change in the mRS, NIH Stroke Scale, or Stroke Impact Scale between the two groups was not significant. Furthermore, this study is not appropriately powered to change clinical practice guidelines to uniformly recommend the use of levetiracetam as seizure prophylaxis in patients with ICH. However, if there is an adequately powered study that demonstrates improvement in functional outcomes in patients with ICH with the administration of levetiracetam, the ED will be the most likely site of drug initiation. Continued discussions should be had with neurology and neurosurgery groups about prophylaxis and its initiation in the ED.
REFERENCES
- De Herdt V, Dumont F, Henon H, et al. Early seizures in intracerebral hemorrhage. Neurology. 2011;77:1794-1800.
- Vespa PM, O’Phelan K, Shah M, et al. Acute seizures after intracerebral hemorrhage. Neurology. 2003;60:144-46.
- Langhorne P, Fearon P, Ronning OM, et al. Stroke unit care benefits patients with intracerebral hemorrhage: a systematic review and meta-analysis. Stroke. 2013;44:3044-49.
- Passero S, Rocchi R, Rossi S, et al. Seizures after spontaneous supratentorial intracerebral hemorrhage. Epilepsia. 2002;43:1175-80.
- Christie C, Daggubati L, Patel N, et al. Effect of newer eneration anticonvulsant prophylaxis on seizure incidence after spontaneous intracerebral hemorrhage. Would Neurosurg. 2020;141:e461-5.
- Messé SR, Sansing LH, Cucchiara BL, et al. Prophylactic antiepileptic drug use is associated with poor outcome following ICH. Neurocrit Care. 2009;11:38-44.
- Naidech AM, Garg RK, Liebling S, et al. Anticonvulsant use and outcomes after intracerebral hemorrhage. Stroke. 2009;40:3810-5.
- Tran QK, Bzhilyanskaya V, Afridi LZ. Preventing seizure occurrence following spontaneous intracerebral hemorrhage: a systematic review and meta-analysis of seizure prophylaxis. Seizure. 2021;87:46-55.