Editor's note: The literature is full of studies that can impact the operations of a health care system. This series from the Admin & Ops Committee examines recent papers and the potential implications for emergency medicine. Find additional literature reviews on their committee page at emra.org.
Syncope is a complex presenting chief complaint spanning several physiologic systems. Its differential includes several "can't miss" etiologies, making diagnosis and disposition sometimes difficult for the emergency provider.
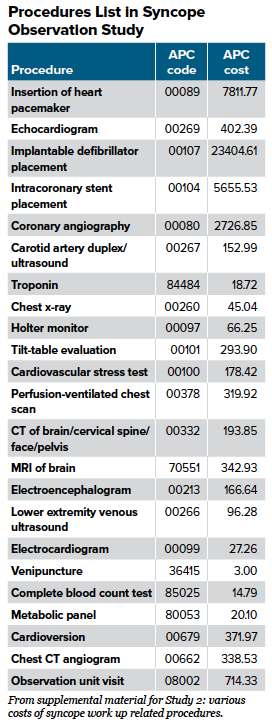
Per The Framingham Study, the estimated incidence of syncope is approximately 6.2 per 1000 person years, accounting for approximately 1% of all ED visits in the United States.1,2 It is estimated that syncope workup and management costs the U.S. healthcare system an annual $2.4 billion.3 The development of ED Observation Units, or EDOUs, have allowed patients and hospitals alike to seek specialized care that is less costly and, in some instances, just as efficient at diagnostics as a full hospitalization. The literature review below will focus on patient-centered outcomes in EDOUs for syncope.
Review of Literature
Syncope Evaluation in the Emergency Department Study (SEEDS): a multidisciplinary approach to syncope management. (Circulation, 2004)
This prospective, single-center study randomized patients in an intermediate-risk group for syncope (met by pre-determined clinical features) into admission versus EDOU for syncope. Notably, the intermediate group contained patients with high-risk features - 43% had a history of CAD, and 57% had an abnormal ECG. In phase 1, patients were randomized to standard care in the ED versus syncope unit - which was equipped with 24-hr telemetry monitoring, TTE, orthostatic BP qhr, and tilt-table testing. The latter group had a higher diagnosis rate (meaning diagnosis for the etiology of syncope). At 2 years, nearly all metrics measured between the two groups were equal - namely, probability of survival at 2 years, recurrent syncope at 2 years, and probability of being free of a syncopal event. The authors conclude that a dedicated syncope observation unit leads to decreased hospital and patient costs and shortened stays, while not affecting all-cause mortality or recurrent syncope.
Randomized clinical trial of an emergency department observation syncope protocol versus routine inpatient admission. (Ann of Emerg Med, 2014)
This randomized control trial of 124 patients across 5 EDs compared an ED observation protocol to inpatient admission for adults over 50 presenting with syncope. The observation unit led to shorter hospital stays (29 versus 47 hours) and serious outcomes were equivalent at both 3 month and 6 months. Zooming in on patient-centered outcomes, there was no significant difference found in patient satisfaction between the two groups. Notably, this paper estimates an average cost for syncope hospitalization at approximately $2420, compared to a mean cost of EDOU observation status of $1400.
Comparison of 1-Day Emergency Department Observation and Inpatient Ward for 1-Day Admissions in Syncope Patients (J Emerg Med, 2016)
Several texts presented above provide evidence for the benefits of EDOU admissions for syncope - notably cost savings and equivalent patient centered outcomes. This study, however, sheds light on a metric that may correlate with patient satisfaction, presuming that patient satisfaction correlates with having a formal diagnosis at time of discharge.
This retrospective cohort study analyzed 351 ED patients admitted to either the hospital or the EDOU for syncope workup. Importantly, none of the EDOU patients had serious etiologies of syncope compared to 38% of admitted inpatients (who tended to be older with more comorbidities, and thus more likely to have serious etiologies of syncope.) Additionally, EDOU patients were much more likely to be discharged without a diagnosis. In this regard, this study points to a potential flaw of EDOU observation workups for syncope, in that patients may be less likely to receive a formal etiology of their syncope compared to their admitted counterparts.
- Role of emergency department observation units in the management of patients with unexplained syncope: a critical review and meta-analysis (Clin Exp Emerg Med, 2017)
This systematic review of EDOU for syncope analyzed a total of six studies - four observational and two RCTs. The authors make a point to comment favorably on the SEEDS trial, included in their analysis and outlined above, for this trial demonstrated that a dedicated syncope workup unit in the ED led to a higher diagnosis rate than hospitalization. The authors comment on two of the main drawbacks to current literature on this subject that require a closer look - namely, who qualifies as ‘intermediate risk’ syncope and would thus benefit from an observational stay as opposed to a full hospitalization, and what qualifies a syncope observational unit (as tilt-table testing is not practical nor cost-effective for most hospital systems). Similar to most of the individual studies analyzed, little weight is placed on patient-centered metrics such as patient satisfaction.
Summary of Literature
There have been limited high-quality papers investigating the role of EDOUs for syncope, but the evidence suggests that they lead to lower healthcare costs and shorter hospital stays. In addition, long-term serious outcomes do not appear significantly different between those admitted to hospital versus observation units.
Looking Forward/What's Next
It is unclear whether observation units have as much diagnostic value as a full hospitalization in the differentiation of syncope, and this is likely based, in large part, on the degree of complex testing available to the observation unit. There is little evidence in the literature evaluating patient satisfaction in observation stays versus full hospital stays. Further research should emphasize bounce-backs, or repeat visits, between those admitted to a full hospitalization versus syncope observation unit. Nevertheless, this review demonstrates the utility of observation units, for syncope but also much more broadly a diverse array of chief complaints, in reducing both patient and hospital cost and achieving shorter length of stays.
Looking ahead, syncope risk stratification tools may further aid emergency providers in determining disposition for patients who present with syncope. A recent systematic review of nine syncope risk stratification tools found the Canadian Syncope Risk Score to have statistically significant high likelihood ratios. See references for this paper to check out the Canadian Syncope Risk Score.
EMRA Administration & Operations Committee Links, Guides and Opportunities
- Check out what's happening with our group at the EMRA A&O landing page.
- Looking to gain a mastery of this and other relevant operational knowledge? Consider applying for EMRA's ED Directors Academy scholarship.
References
- Schappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1997. Vital Health State 13 1999;i-iv, 1-39.
- Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med. 2002; 347: 878-85.
- Moya A et al. Task Force for the Diagnosis and Management of Syncope. Eur Heart J. 2009 Nov; 30(21):2631-71.
- MA Ross et al. State of the art: emergency department observation units. Critical Pathways in Cardiology 2012 Sept; 11(3):128-138.
- Win K Shen et al. Syncope Evaluation in the Emergency Department Study (SEEDS): a multidisciplinary approach to syncope management. Circulation. 2004 Dec 14;110(24):3636-45
- Sun et al. Randomized clinical trial of an emergency department observation syncope protocol versus routine inpatient admission. Ann Emerg Med. 2014 Aug;64(2):167-75.
- Sweanor et al. Multivariable risk scores for predicting short-term outcomes for emergency department patients with unexplained syncope: a systematic review. Acad Emerg Med. 2020 Dec.
- Grossman et al. Comparison of 1-day Emergency Department Observation and Inpatient Ward for 1-day Admissions in Syncope Patients. J Emerg Med. 2016 Feb;50(2):217-22.
- Numeroso et al. Role of emergency department observation units in the management of patients with unexplained syncope: a critical review and meta-analysis. Clin Exp Emerg Med. 2017 Dec; 4(4):201-217.



