The emergency department observation unit (EDOU) is a specialized unit designed for efficient, ongoing medical treatment, assessment, and reassessment of patients before the appropriate decision can be made to either discharge or admit.1 Since the 1960s, EDOUs have been increasingly utilized to avoid unnecessary admissions, optimize inpatient bed capacity, improve emergency department (ED) throughput, and overall deliver more efficient care; all resulting in significant national and hospital cost savings.2 However, since observation services are billed as outpatient services, EDOU expansion may increase out-of-pocket costs for patients, particularly Medicare beneficiaries.1-2 As there is significant speculation, controversy, and media attention surrounding these issues, this literature review aims to explore financial impacts of EDOUs at the hospital and patient levels.
Review of Literature
Emergency Department Observation Units: A Clinical and Financial Benefit For Hospitals
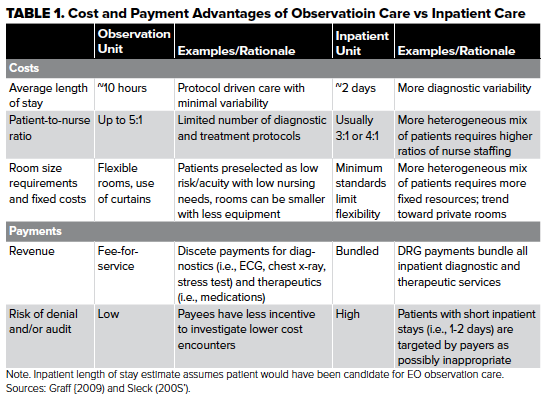
The authors of this literature synthesis present financial arguments and evidence supporting the expansion of EDOUs in hospitals nationwide. According to the authors, EDOUs help hospitals maximize profit margins by billing via a fee-for-service outpatient model, in contrast to the lower reimbursing bundled diagnosis-related groups offered for inpatient services. Moreover, since admissions tend to be costly for hospitals, EDOUs can conserve scarce ED resources and maximize profitability by diverting appropriate patients away from inpatient beds. Additionally, optimizing inpatient bed capacity creates opportunities to manage more profitable cases like elective surgeries, further increasing profit margins. As pressure continues to mount on clinicians and administrators to deliver higher quality care at lower costs, EDOUs help maximize efficiency and profitability of EDs and hospitals. The authors conclude that hospitals with the ED volume to justify the operational costs of establishing an EDOU should consider the return on investment of doing so.3
Factors Associated With Prolonged Observation Services Stays And The Impact Of Long Stays On Patient Cost
The authors performed bivariate analyses and hierarchical linear modeling of Healthcare Cost and Utilization Project data to determine the additional costs of prolonged observation services stays to Medicare beneficiaries. Notably, under Medicare Part A in 2012, inpatients paid no coinsurance for up to 60-day stays after meeting a $1,156 deductible per admission, whereas patients admitted to observation paid 20% coinsurance per treatment with multiple treatments often being the norm (see Table 2). The authors found that Medicare patients in observation services stays were charged $10,373 on average, with stays of 48 to 72 hours and over 72 hours associated with a 42% and 61% increase in costs, respectively. Additionally, medications administered while under observation are not covered as they would be for inpatients or by Medicare Part D, further contributing to increased out-of-pocket costs. The authors conclude that the cost share for observation services stays under 24 hours is on average less than the Medicare Part A deductible amount, but stays longer than 24 hours may raise out-of-pocket costs.4
Protocol-Driven Emergency Department Observation Units Offer Savings, Shorter Stays, And Reduced Admissions
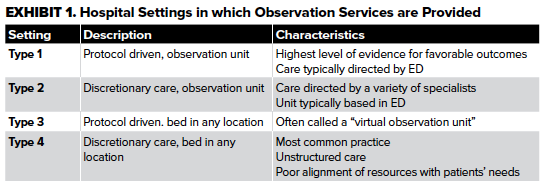
The authors highlight the differences between 4 common approaches to observation services, and discuss the myriad of advantages of providing observation care in a type 1 unit (see Exhibit 1), a dedicated observation unit with well-defined protocols for specific symptoms and diagnoses. Specifically, the benefits include:
- 17% to 44% decreased likelihood of admission following observation care
- 23% to 38% shorter length-of-stays in the hospital
- $950 million in annual national cost savings
As of 2013, two-thirds of hospitals in the United States do not have a dedicated observation unit, and most patients who receive observation services in these hospitals do so in a type 4 unit. As type 1 units offer the most benefits from both clinical and financial standpoints, the authors argue that policymakers should consider monetary incentives for hospitals to employ observation care in type 1 units, as they best align ED resources with patient needs, have shorter length-of-stays, and have lower hospital costs and lower patient copayments compared to other observation settings.5
What Is An Observation Stay? Evaluating The Use Of Hospital Observation Stays In Medicare
The authors of this observational cohort study investigated the extent to which observation stays are used and billed for acute, unscheduled conditions as intended by the Centers for Medicare and Medicaid Services (CMS). The study found that 63% of observation stays were billed under the 0761 revenue code, which is generally used for chronic or episodic conditions as opposed to acute, unscheduled care for patients awaiting discharge or admission. In addition, conditions that involved short-term treatments including maintenance chemotherapy and epidural spinal injections were more likely to be coded as 0761. The rampant use of the 0761 revenue code for observation stays may have unintended cost sharing consequences under Medicare Part B, as no cap exists for patient out-of-pocket costs that would be subsequently incurred. The authors argue that these aberrant billing practices highlight providers’ lack of understanding of policy pertaining to observation stays. Therefore, CMS should provide more guidance regarding the appropriate use of observation stays and whether they should be billed under an alternative mechanism.6
Summary of Literature
EDOUs create an additional disposition option for patients who are too sick for discharge but not sick enough for inpatient admission. By admitting these patients to EDOUs, emergency physicians conserve much-needed ED resources and maximize profit margins with significant cost savings to EDs, hospitals, and national health spendings.1-3 However, as observation services are billed as outpatient services, the high costs of prolonged observation stays are often shifted to patients, disproportionately affecting Medicare beneficiaries.4 As many EDOUs are unstructured and functioning suboptimally, there is a need for protocol-driven observation care that makes financial sense not only to hospitals but also to patients.5 Further guidance from the CMS is also needed to standardize billing practices for observation stays and contain patient out-of-pocket costs.6
Looking Forward/What's Next
As EDOUs are rapidly expanding and cementing their place in United States health systems, the observation of appropriate patients in a dedicated EDOU is becoming increasingly recognized as “best practice.”1 However, EDOUs increase cost sharing for Medicare beneficiaries, as they are billed for outpatient services and are increasingly more likely to be readmitted to the EDOU versus inpatient.7 However, more recent research suggests that same may not be true for the commercially insured, leaving much to considered regarding health equity and disparities.8-11 Therefore, hospitals must adapt to strategically deliver observation services that are both clinically and economically sound, likely through EDOUs, for their patient populations. More research, policymaking, and evidence-based guidelines are needed to standardize their usage and billing, optimize their function, and alleviate cost-sharing burdens on Medicare beneficiaries and others in a manner that is just and equitable.
Other Recommended Literature
-
- Wiler, J.L., Ross, M.A. and Ginde, A.A. (2011), National Study of Emergency Department Observation Services. Academic Emergency Medicine, 18: 959-965. https://doi.org/10.1111/j.1553-2712.2011.01151.x
- https://www.acep.org/by-medical-focus/observation-medicine/observation-services-toolkit/
- /siteassets/new-pdfs/preps/state-of-the-art---observation-units-in-the-ed---prep.pdf
- Ali NJ, Jesus J, Smulowitz PB. Observation Care: Ethical and Legal Considerations for the Emergency Physician. J Emerg Med. 2016;50(3):527-33.e1. doi:10.1016/j.jemermed.2015.11.019
- Wright B, Martin GP, Ahmed A, Banerjee J, Mason S, Roland D. How the Availability of Observation Status Affects Emergency Physician Decisionmaking. Ann Emerg Med. 2018;72(4):401-409. doi:10.1016/j.annemergmed.2018.04.02
Editor’s note: The literature is full of studies that can impact the operations of a health care system. This series from the Admin & Ops Committee examines recent papers and the potential implications for emergency medicine. Find additional literature reviews on their committee page at emra.org.
EMRA Administration & Operations Committee Links, Guides and Opportunities
- Check out what's happening with our group at the EMRA A&O landing page.
- Looking to gain a mastery of this and other relevant operational knowledge? Consider applying for EMRA's ED Directors Academy scholarship.
References
- Napolitano, J.D., Saini, I. Observation Units: Definition, History, Data, Financial Considerations, and Metrics. Curr Emerg Hosp Med Rep 2, 1–8 (2014). https://doi.org/10.1007/s40138-013-0038-y
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323. doi:10.1377/hlthaff.2011.0926
- Baugh CW, Venkatesh AK, Bohan JS. Emergency department observation units: A clinical and financial benefit for hospitals. Health Care Manage Rev. 2011;36(1):28-37. doi:10.1097/HMR.0b013e3181f3c035
- Hockenberry JM, Mutter R, Barrett M, Parlato J, Ross MA. Factors associated with prolonged observation services stays and the impact of long stays on patient cost. Health Serv Res. 2014;49(3):893-909. doi:10.1111/1475-6773.12143
- Ross MA, Hockenberry JM, Mutter R, Barrett M, Wheatley M, Pitts SR. Protocol-driven emergency department observation units offer savings, shorter stays, and reduced admissions. Health Aff (Millwood). 2013;32(12):2149-2156. doi:10.1377/hlthaff.2013.0662
- Powell WR, Kaiksow FA, Kind AJH, Sheehy AM. What Is an Observation Stay? Evaluating the Use of Hospital Observation Stays in Medicare. J Am Geriatr Soc. 2020;68(7):1568-1572. doi:10.1111/jgs.16441
- Kangovi S, Cafardi SG, Smith RA, Kulkarni R, Grande D. Patient financial responsibility for observation care. J Hosp Med. 2015;10(11):718-723. doi:10.1002/jhm.2436
- Adrion ER, Kocher KE, Nallamothu BK, Ryan AM. Rising Use Of Observation Care Among The Commercially Insured May Lead to Total And Out-Of-Pocket Cost Savings. Health Aff (Millwood). 2017;36(12):2102-2109. doi:10.1377/hlthaff.2017.0774
- Sabbatini AK, Wright B, Hall MK, Basu A. The cost of observation care for commercially insured patients visiting the emergency department. Am J Emerg Med. 2018;36(9):1591-1596. doi:10.1016/j.ajem.2018.01.040
- Goldstein JN, Schwartz JS, McGraw P, Hicks LS. "Implications of cost-sharing for observation care among Medicare beneficiaries: a pilot survey". BMC Health Serv Res. 2019;19(1):149. Published 2019 Mar 7. doi:10.1186/s12913-019-3982-8.
- Goldstein JN, Zhang Z, Schwartz JS, Hicks LS. Observation Status, Poverty, and High Financial Liability Among Medicare Beneficiaries. Am J Med. 2018;131(1):101.e9-101.e15. doi:10.1016/j.amjmed.2017.07.013



