Patients presenting to the emergency department with undifferentiated shock have a high mortality rate and often pose a diagnostic challenge early in their course.1
The Rapid Ultrasound for Shock and Hypotension (RUSH) Exam is a protocolized ultrasound exam that can be done in minutes to narrow your differential and identify the etiology of a patient's shock.
The Exam
The RUSH Exam can be remembered by the HI-MAP mnemonic (your goal is to increase the patient's MAP): Heart, IVC, Morrison's Pouch (and complete the FAST), Aorta, and Pneumothorax. The exam should be undertaken in the HI-MAP order and should be done in a timely manner at bedside in the ED. Just as for the E-FAST in traumatic hypotension, the idea isn’t to get detailed measurements but to perform a rapid, goal-directed evaluation of potential causes of shock.
Heart
The cardiac exam can be done in a variety of views, but the parasternal long axis (PLAX) and apical four-chamber (AP4) are optimal and are the views described in the original RUSH Exam paper.2 This goal-directed exam should look for specific causes of shock. An effusion in the setting of shock would suggest tamponade. Poor squeeze would suggest cardiogenic shock while a hyperdynamic left ventricle would suggest hypovolemic or distributive shock. However, it is important to remember that both pulmonary embolism and tamponade also frequently present with a hyperdynamic left ventricle.3 Finally, the exam should evaluate for RV enlargement or signs of RV strain that would suggest a PE. (Read the other entries in the Advanced Critical Care Ultrasound Series for further information on the Signs of Tamponade, EPSS for quantification of LV function, and TAPSE for RV dysfunction.) Although these additional measurements can be helpful, they should not distract you from an efficient RUSH Exam.
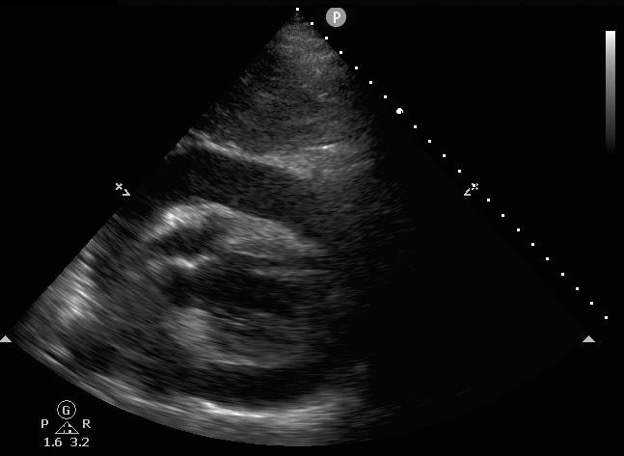
Figure 1: Pericardial Effusion on Ultrasound
IVC
The IVC component of the RUSH Exam, like the cardiac component, should rely on qualitative rather than quantitative measurements for efficiency. The IVC should be viewed near the hepatic arteries, ~2cm from its insertion into the right atrium, in both the longitudinal and transverse planes.4 A large, engorged IVC with minimal respiratory variation would suggest obstructive shock or volume overload, while a small, collapsing IVC would suggest hypovolemic or distributive shock.
In mechanically ventilated patients, the positive pressure breaths will enlarge, rather than collapse, the IVC. Nevertheless, it is the overall size and respiratory variation that should be assessed rather than specific ratios of IVC measurements.
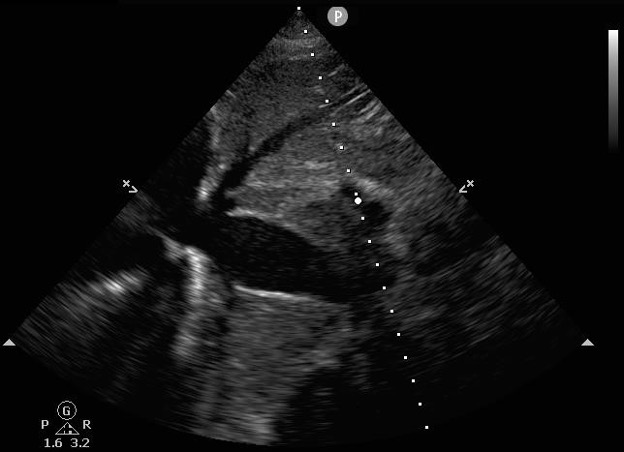
Figure 2: Dilated IVC on Ultrasound. Minimal variation of IVC size with spontaneous breathing would further suggest obstructive shock or volume overload
Morrison's Pouch (and other views)
Free fluid in the abdomen can suggest a number of etiologies for shock, including ruptured ectopic pregnancy, hemorrhage from trauma or intraperitoneal AAA rupture, or simply ascites associated with chronic medical problems. Just as in the FAST Exam, this step of the RUSH Exam includes the RUQ, the LUQ, and suprapubic views.

Figure 3: Free Fluid around the Liver Tip
Aorta
Aortic catastrophes are particularly emergent etiologies of shock that are important to catch without the delays that can be associated with more advanced imaging. The aorta should be scanned transversely from just below the heart to just past the iliac bifurcation.2 A continuous longitudinal view adds further information and visualizes the whole abdominal aorta but was not described in the original paper. Identification of a dissection flap or an aneurysm (aorta >3cm) in the context of shock should prompt an immediate consultation with a surgeon.
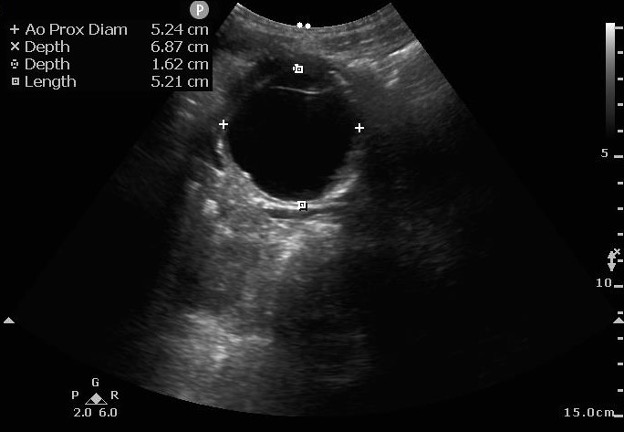
Figure 4: Abdominal Aortic Aneurysm on Ultrasound. Measurements should be done from outside wall to outside wall.
Pneumothorax
Similar to the E-FAST, the final view of the RUSH Exam is the lung views. The RUSH Exam can use the same ultrasound views as the E-FAST and this component is primarily used to identify a pneumothorax by the absence of lung sliding. Normal lung views have shimmering at the pleura with respiration and the "beach sign" on M-mode, while a pneumothorax would be identified by a lack of shimmering at the pleural line and by the "barcode sign" on M-mode.5 This view can also be used to look for B lines (suggesting left-sided heart failure) or consolidation with air bronchograms (suggesting pneumonia and septic shock).
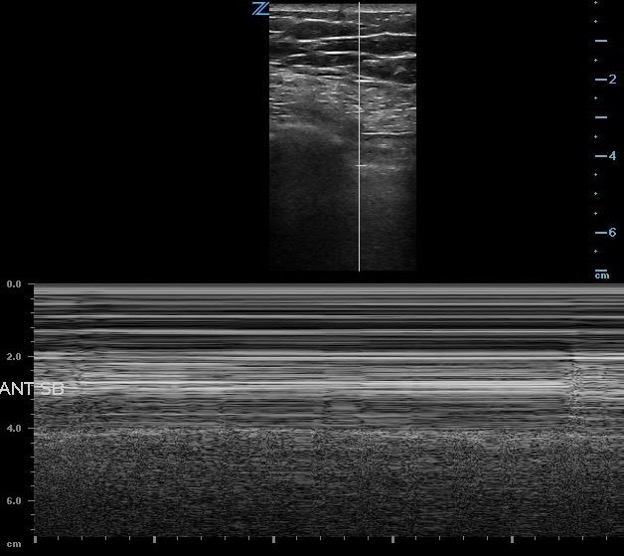
Figure 5: Normal Lung Sliding on M-mode
Evidence
An early RUSH Exam in the ED can help quickly identify the etiology of a patient’s non-traumatic shock. Early identification of critical findings can also lead to rapid definitive management. A number of studies have shown that the RUSH Exam adds value to the ED workup of shock.
A 2004 study by Jones et al. randomized patients in nontraumatic symptomatic shock to receive a standardized ultrasound exam (similar to the RUSH Exam) immediately on arrival to the ED or a delayed ultrasound (after 15 minutes).6 Early standardized ultrasound helped emergency physicians narrow their list of potential diagnoses from a median of nine diagnoses for those who didn't receive the early exam to a median of four for those who did. The physicians were able to identify the correct final diagnosis within 15 minutes of arrival in 80% of patients who got the exam compared to 50% of patients who did not receive the early exam.
Shokoohi et al. followed this study by surveying emergency providers just before and just after providing results of a bedside RUSH Exam. They found that the RUSH Exam decreased diagnostic uncertainty, changed treatment plans in 25% of patients, and increased the proportion of patients with a definitive diagnosis from 0.8% to 12.7%.7
Just as the FAST Exam has become a standard component of the trauma assessment, the RUSH Exam can be a useful addition to your early assessment of non-trauma shock patients. With practice, an efficient exam takes a few minutes and can significantly expedite workup.
References
- Jones AE, Stiell IG, Nesbitt LP, et al. Nontraumatic Out-of-Hospital Hypotension Predicts In-hospital Mortality. Ann Emerg Med. 2004;43(1):106-113.
- Weingart SD, Duque D, Nelson B. Rapid Ultrasound for Shock and Hypotension (RUSH-HIMAPP). EMed Home. 2009.
- Piazza G, Goldhaber SZ. Pulmonary embolism in heart failure. Circulation. 2008;118(15):1598-601.
- Wallace DJ, Allison M, Stone MB. Inferior vena cava percentage collapse during respiration is affected by the sampling location: an ultrasound study in healthy volunteers. Acad Emerg Med. 2010;17(1):96–99.
- Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012;5(1):76-81.
- Jones AE, Tayal VS, Sullivan DM, Kline JA. Randomized, controlled trial of immediate versus delayed goal-directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit Care Med. 2004;32(8):1703-1708.
- Shokoohi H, Boniface KS, Pourmand A, et al. Bedside Ultrasound Reduces Diagnostic Uncertainty and Guides Resuscitation in Patients With Undifferentiated Hypotension. Crit Care Med. 2015;43(12):2562-2569.



