Tricuspid annular plane systolic excursion (TAPSE) can provide a point of care ultrasound assessment of right ventricular function.
Although there are many emerging applications for this measurement, it has been most extensively studied for the evaluation of right ventricular (RV) function in the setting of suspected or diagnosed pulmonary embolism (PE).
The RV, being much less muscular than the left ventricle (LV), cannot handle rapid increases in afterload well.1 PEs do exactly this, increasing afterload by decreasing the number of channels through which blood can leave the RV into the lungs. Worse than that, previously normal physiologic responses can cause harmful consequences in the setting of PE--such as hypoxia-mediated vasoconstriction of pulmonary arterioles.1 Generally, this response acts to shunt blood to oxygenated alveolar units, but in the case of PE, can be harmful by further increasing afterload to an already stressed RV. The interdependence of the ventricles also means that PE can lead to a spiraling decline through other mechanisms. The decreased output from the RV means less blood delivered to the left side of the heart, and consequently, cardiac output can be compromised--including to the coronary vasculature supplying the RV itself. This can further compromise RV function.1 Another consequence of ventricular interdependence is that an overfilled RV can impede LV filling through pressure exerted through the interseptal wall, and again lead to underfilling and decreased output from the LV.1 It would be great if we could detect the patients with PE who are experiencing RV stress before we see changes to their hemodynamics--and that is why we are talking about TAPSE.
The RV is different from the LV in that more of its contractile motion is in a longitudinal plane. This is a consequence of the RV having more myofibers oriented in an apex-to-base direction than the LV which has a more complex and oblique crisscrossing network pattern.2 This is important for TAPSE, as this ultrasound technique measures the change in height of the RV throughout the cardiac cycle and uses this as a surrogate for RV output.
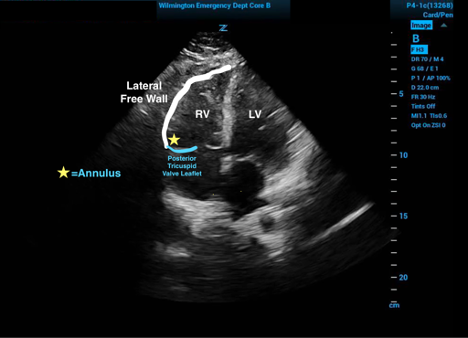
To obtain the TAPSE measurement one must first obtain an echocardiographic four-chamber view of the heart. The M-mode tracer should then be placed in the (posterior) tricuspid annulus just against the free ventricular wall. The waveform generated in M-mode will then produce a tracing of the up and down movement of the base of the heart.3
Figure 1. Relevant cardiac anatomy in the four-chamber view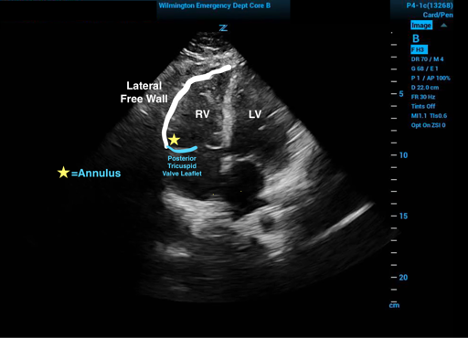
The measured difference of the distance between the peak and trough of this tracing will produce the TAPSE value. Care must be used to place the measurement points on the same side of the tricuspid valve (typically towards the top of the screen) so as to not include the thickness of the valve itself (see Figure 2). This value corresponds to the change in right ventricular height during a cardiac cycle.3
Figure 2. M Mode with tracer spike in the RV posterior tricuspid valve leaflet annulus showing the change in RV height throughout the cardiac cycles with both measurement points on the same side of the valve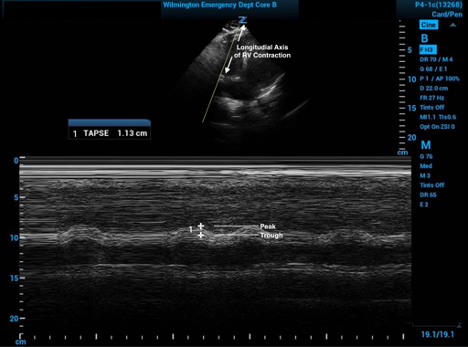
Limitations and Considerations
One limitation of using TAPSE is a lack of a consensus for cutoff values to be used. The patient in Figure 2 has an abnormal TAPSE by just about any published cutoff, but there are some that will fall into a gray zone. The range in retrospective studies that have correlated with RV dysfunction as well as increased mortality attributable to acute PE are generally 15mm-20mm.6-11 A joint abnormal cutoff established by the American Society of Echocardiography and the European Association of Cardiovascular Imaging is ≤ 16mm.12 One must take care when placing the M-mode tracer spike, as small misplacement and poor placement of the angle of the M-mode cursor can translate to large differences in measurement.
Another potential limitation of TAPSE is that it is not direct evidence of PE and instead only of RV dysfunction. Other pathologies, both acute and chronic, such as pulmonary hypertension and chronic heart failure, may therefore lead to abnormal TAPSE values. You must also consider that in TAPSE, RV function assessed is only in one plane, and although there is significant RV contractility in the longitudinal plane, TAPSE does not assess the other planes of contractility. Therefore, TAPSE may not be as accurate in patients with regional differences in their RV function. Luckily, there is good correlation of TAPSE with other RV systolic function measurements that do account for multiple planes.12
Benefits of TAPSE
TAPSE only requires one view of the heart to obtain (apical four-chamber) and therefore can be done quickly.
An additional benefit of TAPSE is the apical four-chamber view is used to assess LV to RV ratio, can be used to assess LV septal flattening (sign of D), and can be used to look for McConnell's sign (right ventricular free wall akinesis sparing the apex), which are other common abnormal echocardiographic changes seen in the setting of PE. TAPSE demonstrates a higher interobserver reproducibility when compared to visual judgment of both increased RV:LV ratio and RV free wall hypokinesis.5
In one ED-based study, a mix of experienced and inexperienced ultrasound users were able to get appropriate views in 98% of patients and showed 0.97 correlation for measurements between the inexperienced and the more experienced operators.
This same study found a sensitivity of 72% and specificity of 66% (using a cutoff of 2.0cm), which was much more sensitive but not as specific as McConnel’s sign or septal flattening. As stated above, TAPSE is obtained with the same view and can be part of a multi-sign evaluation and when combined with McConnel’s sign, septal flattening, RV enlargement, and tricuspid regurgitation seen on four-chamber view with Doppler, has a 100% sensitivity for PE. In patients with either tachycardia or hypotension, the sensitivity of TAPSE alone increased to 94%.5
TAKE-HOME POINTS
- The ultrasound view to assess TAPSE can be achieved in the vast majority of patients by emergency physicians, who can then measure TAPSE quickly and reliably.
- Applied to the right patient population, TAPSE is highly sensitive for RV dysfunction.
- Therefore, TAPSE is a great tool to help find RV strain and risk-stratify your PE patients.
References
- Bryce YC, Perez-Johnston R, Bryce EB, et al. Pathophysiology of right ventricular failure in acute pulmonary embolism and chronic thromboembolic pulmonary hypertension: a pictorial essay for the interventional radiologist. Insights Imaging. 2019;10(18).
- Ho SY, Nihoyannopoulos P. Anatomy, echocardiography, and normal right ventricular dimensions. Heart. 2006;92 Suppl 1(Suppl 1):i2-i13.
- Alam M, Wardell j, Andersson E, Samad B A, Nordlander R. Characteristics of mitral and tricuspid annular velocities determined by pulsed-wave Doppler tissue imaging in healthy subjects. J Am Soc Echocardiogr. 1999;12:618–628.
- Kopecna D, Briongos S, Castillo H, et al., PROTECT investigators. Interobserver reliability of echocardiography for prognostication of normotensive patients with pulmonary embolism. Cardiovasc Ultrasound. 2014;12:29.
- Daley J, Grotberg J, Pare J, et al. Emergency physician performed tricuspid annular plane systolic excursion in the evaluation of suspected pulmonary embolism. Am J Emerg Med. 2017;35(1):106-111.
- Weekes AJ, Johnson AK, Troha D, Thacker G, Chanler-Berat J, Runyon M. Prognostic Value of Right Ventricular Dysfunction Markers for Serious Adverse Events in Acute Normotensive Pulmonary Embolism. J Emerg Med. 2017;52(2):137-150.
- Lobo JL, Holley A, Tapson V, et al., PROTECT and RIETE investigators. Prognostic significance of tricuspid annular displacement in normotensive patients with acute symptomatic pulmonary embolism. J Thromb Haemost. 2014;12(7):1020-1027.
- Pruszczyk P, Goliszek S, Lichodziejewska B, et al. Prognostic value of echocardiography in normotensive patients with acute pulmonary embolism. JACC Cardiovasc Imaging. 2014;7(6):553-560.
- Paczynska M, Sobieraj P, Burzynski T, et al. Tricuspid annulus plane systolic excursion (TAPSE) has superior predictive value compared to right ventricular to left ventricular ratio in normotensive patients with acute pulmonary embolism. Arch Med Sci. 2016;12(5):1008-1014.
- Schmid E, Hilberath JN, Blumenstock G, et al. Tricuspid annular plane systolic excursion (TAPSE) predicts poor outcome in patients undergoing acute pulmonary embolectomy. Heart Lung Vessel. 2015;7(2):151-158.
- Ciurzynski M, Kurnicka K, Lichodziejewska B, et al. Tricuspid Regurgitation Peak Gradient (TRPG)/Tricuspid Annulus Plane Systolic Excursion (TAPSE)- A Novel Parameter for Stepwise Echocardiographic Risk Stratification in Normotensive Patients With Acute Pulmonary Embolism. Circ J. 2018;82(4):1179-1185.
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14.