A common use for point of care ultrasound in the emergency department is estimation of cardiac function, often expressed by the left ventricular ejection fraction (LVEF).
Emergency physicians have been shown to be accurate at visual estimation of the LVEF without quantitative measurements.1,2 However, there is still value in a quick and easy quantitative measurement of the LVEF. Objective measurements can be helpful for early learners who aren’t yet confident in visual LVEF estimation, they are easier to communicate with consultants and colleagues, and they can be compared to previous values. The E-Point Septal Separation (EPSS) is an easy measurement to obtain that is accurate in estimating the LVEF.
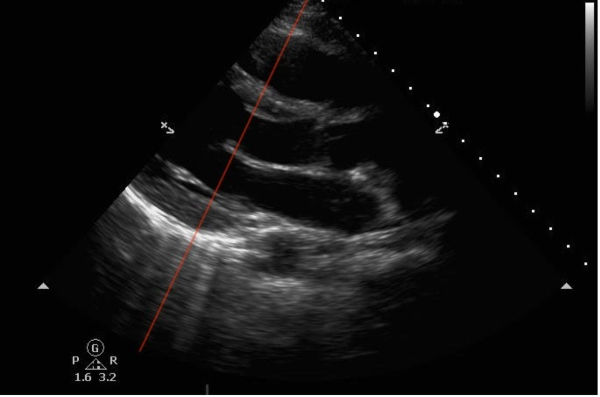
EPSS is measured in the parasternal long axis view (PLAX) of the heart, which gives a view of the left ventricle and is often used to assess its function. EPSS is obtained by placing the M-mode tracer over the distal tip of the anterior leaflet of the mitral valve, as in the image below.
Figure 1: Red line showing correct M-mode cursor placement in PLAX view. (Images via Dr. Salerno)
The mitral valve waveform on M-mode contains two peaks. The first, larger peak is called the "E-point" and corresponds to the maximal mitral valve opening in early LV diastole. The second, smaller peak is called the "A-point" and corresponds to atrial contraction later in LV diastole. In a normally functioning heart, the mitral valve should open with the leaflet hitting or coming very near to the interventricular septum at the E-point. Thus, a healthy heart will have a very small distance between the E-point and the interventricular septum, and this distance is called the E-Point Septal Separation (EPSS). Therefore, EPSS is negatively correlated with LVEF.
An EPSS > 7 mm is evidence of reduced LVEF. Of note, EPSS ≥ 13 mm correlates with severely decreased function, with an estimated LVEF of ≤ 35%.3 In the image below, EPSS is 8.8 mm, indicating abnormal systolic function.
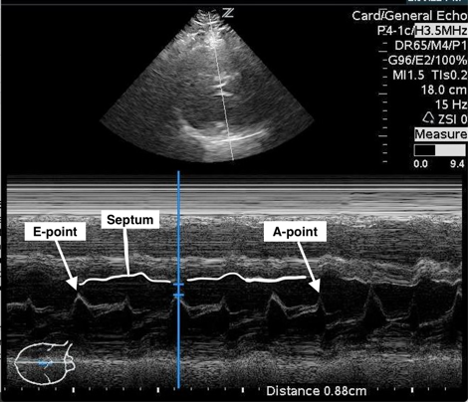
Figure 2: Measurement of EPSS (blue calipers) with labels of E-point, A-point and partial tracing of septal wall (Images via Dr. Salerno)
For most patients, EPSS gives a good estimation of heart function. One study derived the following equation: LVEF = 75.5 – (2.5 x EPSS) with a correlation of r= 0.80.4 A second study derived a similar equation and correlation and demonstrated 100% sensitivity of an EPSS measurement > 7mm for detecting severely reduced EF (<30%).5
There are some patient populations in which EPSS may give an inaccurate estimate of cardiac function. Patients with mitral stenosis have poor opening of their mitral valve even with otherwise adequate cardiac function, and may have a falsely high EPSS measurement despite normal function. Similarly, patients with aortic regurgitation may also have poor forward anterior leaflet movement and will have a falsely high EPSS measurement while possibly having a preserved LVEF. Patients with atrial fibrillation will lack an A-point due to lack of coordinated atrial contraction, and will have beat-to-beat variability in EPSS due to the same discoordination.6 To improve estimations in these patients averaging several measurements of EPSS is required.
In the absence of these conditions, EPSS gives a reliable, fast, quantitative measure of cardiac function that can help verify emergency physicians’ visual estimations and be used to communicate the degree of cardiac dysfunction to other consultants and colleagues.
References
- Ünlüer Erden E, et al. Visual estimation of bedside echocardiographic ejection fraction by emergency physicians. West J Emerg Med. 2014;15(2): 221.
- Moore CL, et al. Determination of left ventricular function by emergency physician echocardiography of hypotensive patients. Acad Emerg Med. 2002;9(3):186-193.
- Ma O, Mateer JR, Reardon RF, Joing SA. Emergency Ultrasound, Third Edition. McGraw Hill Education. 2014.
- Silverstein JR, Laffely NH, Rifkin RD. Quantitative estimation of left ventricular ejection fraction from mitral valve E-point to septal separation and comparison to magnetic resonance imaging. Am J Cardiol. 2006;97(1):137-140.
- McKaigney CJ, Krantz MJ, La Rocque CL, Hurst ND, Buchanan MS, Kendall JL. E-point septal separation: a bedside tool for emergency physician assessment of left ventricular ejection fraction. Am J Emerg Med. 2014;32(6):493-497.
- Massie BM, Schiller NB, Ratshin RA, Parmley WW. Mitral-septal separation: New echocardiographic index of left ventricular function. Am J Cardiol. 1977;39(7):1008-1016.