Cardiac tamponade is a critical emergency department diagnosis, but it can be a difficult diagnosis to make based on physical exam alone.
Clinical signs of tamponade are often late findings and can be evidence of physiologic decompensation. For those patients with large pericardial effusions but no exam findings of tamponade, bedside ultrasound can be an important tool for identifying tamponade physiology.
Clinical Signs
Clinical signs of tamponade appear late and are not sensitive enough to be relied on for diagnosis. Beck’s Triad is the classically taught presentation of tamponade, and includes hypotension with narrowed pulse pressure, jugular venous distention, and muffled heart sounds. However, 27-43% of tamponade patients are actually hypertensive at presentation because of sympathetic surge, and fewer than 20% of patients demonstrate all elements of Becks Triad.1,2 Only half of patients with ultrasound findings of tamponade will have even one of the elements of the triad.1 These physical exam findings also lack specificity. JVD, for example, can be related to other etiologies such as volume overload, valvulopathies, and chronic conditions such as pulmonary hypertension.1
Ultrasound Signs
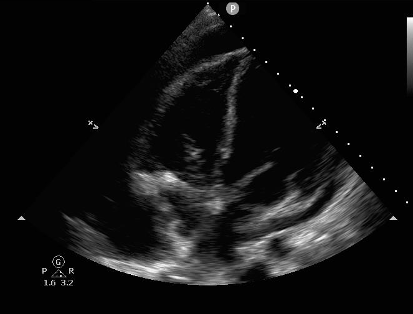
Ultrasound exam for cardiac tamponade must logically start with identification of a pericardial effusion. Emergency medicine physicians have shown that they can use point of care ultrasound with high sensitivity and specificity to find effusion.3 Acute effusions, such as in trauma, can be significant even when very small. If the pericardial space does not have time to stretch and accommodate the new fluid, pressure will rise quickly as it is inversely related to the volume the fluid occupies. The identification of any pericardial effusion in a hypotensive trauma patient should be considered evidence of tamponade until proven otherwise. Chronic effusions, however, can become very large before the development of tamponade physiology.4
Figure 1: Pericardial effusion 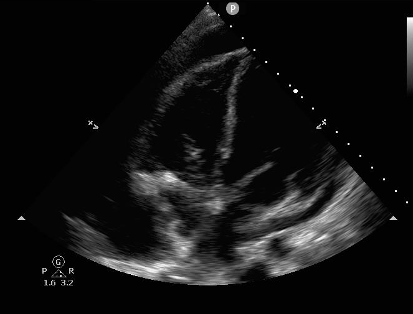
Once a pericardial effusion is identified, the examiner must establish if the effusion is causing tamponade physiology. There are a number of echocardiographic signs of tamponade:
- Right atrial (RA) collapse during cardiac systole
- Right ventricular (RV) collapse during cardiac diastole
- Respiratory flow variation across the mitral valve
- Inferior vena cava (IVC) size and respiratory variability
RA Systolic and RV Diastolic Collapse
During each chamber’s diastole the chamber should relax and fill with blood. Collapse of a chamber during its diastole is a sign that the pressure from a pericardial effusion is inhibiting diastolic filling. This can be seen in the RA during cardiac systole and in the RV during cardiac diastole. In tamponade, the RA often collapses before the RV and is therefore an earlier sign of tamponade and present at lower pericardial volumes.5,6 RV collapse has demonstrated excellent sensitivity and specificity, with some studies showing it to be 100% specific for cardiac tamponade (although these studies are largely from long ago and with small n’s).6-8
There are two methods to establish systolic/diastolic collapse. First, one can record a video clip in either the apical four-chamber view or subxiphoid view and rewind slowly to look at the chambers when the mitral valve is open (diastole) or closed (systole). Second, one can place the M mode marker over the anterior leaflet of the mitral valve to produce the image below (Figure 2). The mitral valve tracing produces an E and A wave during mitral opening, and thus ventricular diastole. Ventricular wall collapse during this peak establishes tamponade.5-8
Like clinical signs of tamponade, echocardiographic signs aren’t perfect. Anything that increases cardiac chamber pressures at baseline, such as pulmonary hypertension, pulmonary embolism, and left to right cardiac shunts, will make RA and RV collapse later findings. Conditions, such as volume depletion, that decrease right intraventricular pressures would do the opposite. Because of this, cardiac chambers may briefly collapse in diastole without tamponade. RA collapse for more than one-third of the cardiac cycle is therefore more specific than transient collapse.9
Figure 2: M Mode tracing of mitral valve demonstrating diastolic right ventricular collapse. Image courtesy of Dr. Sarah Murthi.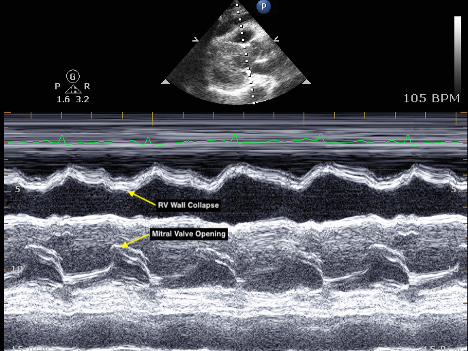
Respiratory Flow Variation across the Mitral Valve
Respiratory flow variation across the mitral valve is the echocardiographic manifestation of the same physiology that produces pulsus paradoxus. A heart in tamponade exhibits increasing ventricular interdependence: because it is enclosed in a relatively fixed pericardium, the dilation of one ventricle must impinge on the other ventricle. The negative thoracic pressure generated by inspiration increases inflow to the RV and causes further impingement on the LV. Cardiac tamponade exaggerates ventricular interdependence by decreasing overall volume in the pericardium, decreasing LV end diastolic volume and flow across the mitral valve during inspiration. Decreased LV end diastolic volume causes pulsus paradoxus, while the decrease in mitral valve flow into the higher pressure LV can be measured by pulse wave Doppler placed in the RV just behind the mitral valve in the apical four chamber view.10 This can be seen in Figure 3.
Figure 3: Respiratory Variability of Mitral Valve Inflow. Image courtesy of Dr. Seyed Hossein Aalaei-Andabili.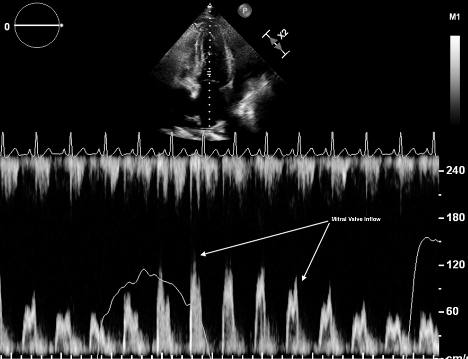
IVC Exam
Cardiac tamponade produces an obstructive shock pattern and will result in a distended IVC with little respiratory variability. This can be identified with an ultrasound view of the IVC. This can be done by first getting a subxiphoid view of the heart and then rotating the probe so the indicator points to the ceiling. Your measurement should take place at least 2 cm from the IVC/RA junction as this has been shown to increase repeatability and correlation with other sites in the IVC for degree of collapse.11 Abnormal findings are a diameter equal to or greater than 2cm and collapsibility of less than 50% upon inspiration.12 It is important to remember that a distended IVC is simply evidence of obstruction to right sided emptying, and cannot distinguish tamponade from other obstructive etiologies such as acute pulmonary embolism. If absent, however, tamponade is unlikely.
Figure 4: Distended IVC with hepatic veins entering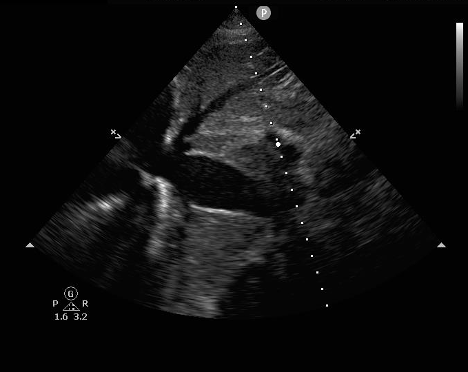
Conclusion
The physical exam findings of cardiac tamponade are often late findings, and bedside ultrasound can be a useful adjunct to identify tamponade in those patients with large effusions. Findings consistent with tamponade include effusion with RA/RV collapse, respiratory variability of flow across valves, and an engorged IVC. The presence of these factors should prompt management of tamponade even in the absence of clinical changes.
References
- Stolz L, Valenzuela J, Situ-LaCasse E, et al. Clinical and historical features of emergency department patients with pericardial effusions. World J Emerg Med. 2017;8(1):29-33.
- Argulian E, Herzog E, Halpern DG, Messerli FH. Paradoxical hypertension with cardiac tamponade. Am J Cardiol. 2012;110(7):1066-1069.
- Mandavia DP, Hoffner RJ, Mahaney K, Henderson SO. Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001;38(4):377-382.
- Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349(7):684-690.
- Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66(4):493-496.
- Singh S, Wann LS, Schuchard GH, et al. Right ventricular and right atrial collapse in patients with cardiac tamponade--a combined echocardiographic and hemodynamic study. Circulation. 1984;70(6):966-971.
- Armstrong WF, Schilt BF, Helper DJ, Dillon JC, Feigenbaum H. Diastolic collapse of the right ventricle with cardiac tamponade: an echocardiographic study. Circulation. 1982;65(7):1491-1496.
- Singh S, Wann LS, Klopfenstein HS, Hartz A, Brooks HL. Usefulness of right ventricular diastolic collapse in diagnosing cardiac tamponade and comparison to pulsus paradoxus. Am J Cardiol. 1986;57(8):652-656.
- Argulian E, Messerli F. Misconceptions and facts about pericardial effusion and tamponade. Am J Med. 2013;126(10):858-861.
- Ginghina C, Beladan CC, Iancu M, et al. Respiratory maneuvers in echocardiography: a review of clinical applications. Cardiovasc Ultrasound. 2009;7:42.
- Wallace DJ, Allison M, Stone MB. Inferior vena cava percentage collapse during respiration is affected by the sampling location: an ultrasound study in healthy volunteers. Acad Emerg Med. 2010;17:96–99.
- Himelman RB, Kircher B, Rockey DC, Schiller NB. Inferior vena cava plethora with blunted respiratory response: a sensitive echocardiographic sign of cardiac tamponade. J Am Coll Cardiol. 1988;12(6):1470-1477.