Elderly patients with chest wall injuries have a mortality rate up to 13% - attributed in part to the effects of pain. EAST guidelines offer a range of analgesic options, but ultrasound-guided serratus anterior plane block may be another technique in the EM arsenal.
Case
A 54-year-old man presented to the ED with a chief complaint of left chest wall pain. He reported that he was in a bar fight several days ago, and since then had persistent pain in his left chest where he was struck. The pain is worsened with deep inspiration and coughing. He denied any other injuries, and a review of systems revealed no other complaints.
Vital signs were blood pressure 173/94, heart rate 95, respiratory rate 18, temperature 98.9°F, and pulse oximetry 95% on room air. Physical exam revealed clear lung sounds bilaterally. The patient’s left lateral chest wall was tender, but there was no crepitus, ecchymosis, or deformities. No other injuries were identified. Imaging revealed lateral nondisplaced fractures of the left 3rd and 4th ribs only.
Background
Chest wall injuries are a common injury in the United States, with rib fractures being a typical manifestation. The Eastern Association for the Surgery of Trauma (EAST) estimates that rib fractures account for 10% of patients hospitalized for trauma. Elderly patients with multiple rib fractures, in particular, have a mortality of 3-13%, leading many protocols to necessitate intensive care unit (ICU) admission for such patients.1 A large degree of mortality is attributed to chest wall pain impacting respirations and cough, leading to pulmonary complications such as pneumonia, and thus management is directed toward adequate analgesia.
EAST guidelines recommend using several pain control modalities, including oral and parenteral medications as well as regional anesthesia. Regional anesthesia is associated with reduced opioid use and improved pulmonary toilet, which can be particularly desirable in elderly patients prone to delirium and post-rib fracture pneumonia.1-4 However, the described techniques include methods such as epidural anesthesia or thoracic paravertebral blocks (TPVB), which emergency physicians are not routinely trained to perform and thus are not readily available in the ED.
One potential alternative is the ultrasound (US)-guided serratus anterior plane block (SAPB). The SAPB was first described in 2013 as a way to anesthetize the chest wall for breast surgery.5 Since then, it has been adopted for many other purposes, including analgesia after chest wall trauma.6,7,8 Small studies have found non-inferiority between the SAPB and thoracic epidural anesthesia or TPVB for traumatic rib fractures; with SAPB also avoiding the undesirable sympathetic effects of neuraxial anesthesia.7,8 Additionally, there are no contraindications in patients with coagulopathy or on antiplatelet/anticoagulant therapy, and SAPB is relatively easy to perform by an emergency physician trained in US-guided procedures.
Performing the Block
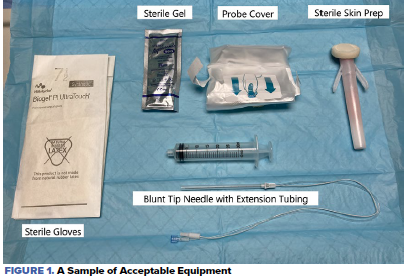
A sample of acceptable equipment is displayed in Figure 1. The patient is placed ideally in the lateral recumbent position, with the hemithorax to be anesthetized up. After sterile preparation of the skin, a high-frequency linear US transducer in the transverse orientation is placed in the middle to the posterior axillary line, at the level of the 4th and 5th ribs. (Note: some sources suggest the 5th and 6th ribs, but as anesthetic will spread along a fascial plane, a plane block requires less precise infiltration).9
Physicians should choose the local anesthetic most appropriate to the desired duration of effect. Our experience with the indications for SAPB would typically require a longer-acting anesthetic such as bupivacaine. The maximum dose of anesthetic should be calculated for each patient in order to avoid local anesthetic systemic toxicity (LAST). Even when below the maximum dose, patients should be placed on a cardiac monitor, with pulse oximetry and IV access, as well as ready access to intralipid emulsion.
Key structures to identify are the latissimus dorsi muscle, the serratus anterior muscle, the 4th and 5th ribs, and the underlying pleural line as demonstrated in Figure 2. The block will principally anesthetize the lateral cutaneous branches of the intercostal nerves, which penetrate both above and below the serratus anterior muscle.
Enter the skin with the needle in-plane with the probe orientation. The needle should be advanced until the tip is visualized in the plane between the latissimus dorsi and serratus anterior muscle, or alternatively may be placed below the serratus anterior muscle, above the ribs. Some operators have suggested angling the needle toward the rib, as a “backstop” to prevent the needle from violating the pleura should the patient cough or move. Ideally, with the help of a second operator and after aspiration to avoid intravascular injection, a small amount of anesthetic is injected to confirm the position of the needle tip, often termed “hydrodissection.” If the anechoic fluid appears to flow backwards towards the needle, this suggests the tip is placed in the muscle belly and needs to be adjusted. If appropriately placed, fluid will advance away from the needle tip, with clear separation of the lats and serratus anterior, as in Figure 3. Once the placement is confirmed, the remainder of the anesthetic may be slowly injected, with periodic gentle aspiration.10,11,12
In addition to LAST, performers of the SAPB should evaluate the patient afterward for signs of pneumothorax, which can quickly and easily be done with high accuracy with ultrasound at the point of care. One case report suggested that pneumothorax may be less likely when placing an anesthetic above the serratus anterior muscle, with the trade-off that the patient may experience less relief; however, there are no high-quality studies yet to confirm this.13 There have also been concerns raised regarding blockade of the long thoracic nerve during SAPB interfering with its identification during axillary dissection in surgery, but this would likely be less important when performed for non-surgical chest wall pain.14

What’s Next
US-guided regional anesthesia is relatively new in the ED, partially due to several real and perceived barriers to its use, such as increased time to perform the block, or lack of familiarity with nerve identification and nerve block technique. Helpful to the emergency physician is the recent American College of Emergency Physicians’ (ACEP’s) policy paper supporting the use of ED US-guided nerve blocks.15 Ongoing research and educational training initiatives for UGRA in EM training programs will help to alleviate subspecialty resistance, which is often cited as a barrier for performing more common blocks such as the fascia iliaca compartment block for hip fractures.16 As training in US-guided procedures during residency becomes more commonplace, more and more physicians will be familiar with the basic procedural tenets to accomplish UGRA.
The use of SAPB blocks in the ED is currently a topic of ongoing research, with several studies registered on ClinicalTrials.gov. With emergency physicians becoming more familiar with this block, it can be adopted for other painful chest wall conditions, such as herpes zoster, chest wall abscesses or lacerations, and thoracostomy tube placement.17
Case Conclusion
After obtaining patient consent, a left-sided SAPB with 10mL of 0.5% bupivacaine and 20mL of sterile normal saline was performed under US guidance. No complications were noted, and on re-evaluation 10 minutes after the procedure, the patient-reported complete relief of his pain. He was discharged home with recommendations for continued over-the-counter analgesic medicines and clear return precautions. A follow-up phone call revealed high patient satisfaction with effective pain relief in the subsequent 10-12 hours.
HCA Healthcare disclaimer
"This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities."
References
- Galvagno SM, Smith CE, Varon AJ, et al. Pain management for blunt thoracic trauma. Journal of Trauma and Acute Care Surgery. 2016;81(5):936-951. doi:10.1097/ta.0000000000001209
- Rose P, Ramlogan R, Sullivan T, Lui A. Serratus anterior plane blocks provide opioid-sparing analgesia in patients with isolated posterior rib fractures: a case series. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2019;66(10):1263-1264. doi:10.1007/s12630-019-01431-7
- Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. Journal of Orthopaedics and Traumatology. 2009;10(3):127-133. doi:10.1007/s10195-009-0062-6
- Parris R, Scobie B. Epidural analgesia/anaesthesia versus systemic intravenous opioid analgesia in the management of blunt thoracic trauma. Emergency Medicine Journal. 2007;24(12):848-849. doi:10.1136/emj.2007.054999
- Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. 2013;68(11):1107-1113. doi:10.1111/anae.12344
- Kunhabdulla NP, Gupta R, Gautam SK, Gaur A, Agarwal A. Serratus Anterior Plane Block for Multiple RibFractures. Pain Physician. 2014;5;17(5;9). doi:10.36076/ppj.2014/17/e651
- Bhalla PI, Solomon S, Zhang R, Witt CE, Dagal A, Joffe AM. Comparison of serratus anterior plane block with epidural and paravertebral block in critically ill trauma patients with multiple rib fractures. Trauma Surgery & Acute Care Open. 2021;6(1). doi:10.1136/tsaco-2020-000621
- Khalil AE, Abdallah NM, Bashandy GM, Kaddah TA-H. Ultrasound-Guided Serratus Anterior Plane Block Versus Thoracic Epidural Analgesia for Thoracotomy Pain. Journal of Cardiothoracic and Vascular Anesthesia. 2017;31(1):152-158. doi:10.1053/j.jvca.2016.08.023
- Mayes J, Davison E, Panahi P, et al. An anatomical evaluation of the serratus anterior plane block. 2016;71(9):1064-1069. doi:10.1111/anae.13549
- Farag E, Mounir-Soliman L, Brown DL. Serratus anterior block. In: Brown's Atlas of Regional Anesthesia. 6th ed. Philadelphia, PA: Elsevier; 2021:207-210.
- Blanco R, Barrington MJ. Pectoralis and Serratus Plane Nerve Blocks. NYSORA. https://www.nysora.com/regional-anesthesia-for-specific-surgical-procedures/thorax/pectoralis-serratus-plane-blocks/. Published March 22, 2021. Accessed May 27, 2021.
- Avila J. 5 Minute Sono – Serratus Anterior Block. Core Ultrasound. https://www.coreultrasound.com/serratus/. Published June 19, 2020. Accessed May 27, 2021.
- Desai M, Narayanan MK, Venkataraju A. Pneumothorax following serratus anterior plane block. Anaesthesia Reports. 2020;8(1):14-16. doi:10.1002/anr3.12034
- Miller B, Pawa A, Mariano E. Problem with the Pecs II block: the long thoracic nerve is collateral damage. Regional Anesthesia and Pain Medicine. 2019;44(8):817-818. doi:10.1136/rapm-2019-100559
- Ultrasound-Guided Nerve Blocks. ACEP. https://www.acep.org/patient-care/policy-statements/ultrasound-guided-nerve-blocks/. Accessed May 27, 2021.
- Wilson CL, Chung K, Fong T. Challenges and Variations in Emergency Medicine Residency Training of Ultrasound-guided Regional Anesthesia Techniques. AEM Education and Training. 2017;1(2):158-164. doi:10.1002/aet2.10014
- Goldsmith AJ, Liteplo AS, Shokoohi H. Ultrasound-guided serratus anterior plane block for intractable herpes zoster pain in the emergency department. J Emerg Med. 2020;59(3):409-12.