Yes, you read that title correctly. This article is about giving your patients bacteria. . . probiotics, that is.
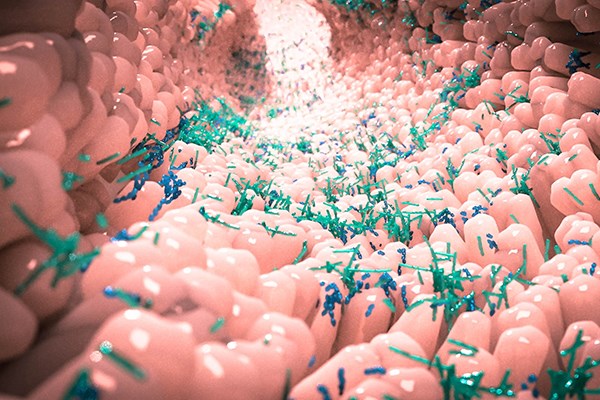
In the ED, we see a lot of complaints that may be responsive to probiotics. Probiotics are "live microorganisms that, when administered in adequate amounts, confer a health benefit on the host".1 In practice, the most common and accepted use of probiotics is as an oral form of a bacteria native to the patient's gut microbiome. They have long been thought of as a nontraditional treatment modality; however, research on the role of probiotics and the microbiome has exploded in recent years.
The role of the microbiome is becoming more and more apparent. It has been shown to be associated with several autoimmune conditions and is now accepted as the likely pathology of many functional bowel disorders, including irritable bowel disease (IBS). It also plays a major role in metabolism and obesity. The role of the microbiome from birth is highlighted by the increased rates of asthma, allergies, and gastrointestinal disorders with cesarean births. There is even evidence supporting the practice of introducing a mother's vaginal secretions to their baby's skin after a cesarean birth in an effort to influence the microbiome of the infant.2 The role of the microbiota is further evidenced by the increasing use of fecal microbiota transplant, now approved for chronic Clostridium difficile (C. diff) colitis and soon to be approved for inflammatory bowel disease.
Another way to alter the microbiome is the use of probiotics. They have been used for centuries and studied since the early 1900s, with the first commercially developed probiotics becoming available in 1935.3 The original theory was that by introducing "good" bacteria species into the gastrointestinal (GI) tract, the growth of beneficial colonies of flora would be promoted. This view has since been superseded by the modern theory on probiotics, which suggests more of an immunomodulatory role. However, let's address some evidence-based applications of probiotics in the ED.
Antibiotic-Associated Diarrhea
The most common and perhaps most well-studied use of probiotics is for the prevention of antibiotic-associated diarrhea. The literature has demonstrated clear benefit with probiotic use for both adults and children to reduce the risk for both C. diff and non-clostridial diarrhea. This applies to both admitted and discharged patients.4
C. diff is a well-known and feared complication of antibiotic use. The concept of using probiotics for C. diff prophylaxis has been suggested for inpatient and critically ill patients for several years. Some moderate-quality evidence suggests this is helpful, with the most benefit for those at higher risk (>5%) of contracting C. diff.
There was some discussion in the medical community after a 2018 study published in Cell suggested that patients taking probiotics may not restore their normal flora after antibiotic exposure as quickly as those not taking probiotics.5 Critics of probiotics cited this as evidence of futility, while supporters suggested it may actually serve as evidence for the immunomodulator theory. While the question of mechanism does warrant further investigation, the study was a small, mechanistic study that enrolled only 21 patients and is unable to overturn the clear trend toward benefit observed in over 20 randomized controlled trials. Therefore, we should continue to give every patient to whom we prescribe antibiotics a probiotic until the mechanism of action can be better understood.
Gastroenteritis/Gastritis
There is strong evidence that diarrhea associated with pediatric gastroenteritis improves more rapidly when the child receives probiotics in addition to oral rehydration therapy.6,7 The literature regarding probiotics in adults with gastroenteritis is inconclusive at this time, but it should be stated that no studies have found any increased risk of complications with the use of probiotics.
There is some evidence to suggest that probiotics aid in Helicobacter pylori clearance when used in combination with triple or quadruple therapy. For other causes of gastritis, the data is unclear. There have been innumerable animal and in vitro studies suggesting a benefit in gastritis, but the studies in humans so far have focused on H. pylori.
Hepatic Encephalopathy
Patients with hepatic encephalopathy (HE) are traditionally given rifaximin and lactulose therapy. Rifaximin works by destroying gut bacteria that produce ammonia, which is thought to be the cause of HE. Following this theory, probiotic use would be implicated as a potential benefit. Not surprisingly, several studies have shown that probiotics compared to placebo (with or without lactulose) improve symptom resolution in HE. No studies have shown mortality benefit, however.8 In this, it would be reasonable to add probiotics to lactulose/ rifaximin therapy in patients with HE.
Irritable Bowel Syndrome
Probiotics have overwhelmingly been shown to improve symptoms in functional bowel disorders. Specifically, they have been studied in the context of IBS in adults and chronic diarrhea in children.9 This is in line with what we now understand as an underlying pathophysiologic factor in IBS- small intestinal bacterial overgrowth (SIBO). Despite what you may have been taught, IBS is not purely psychosomatic or anxiety-driven, though these factors may still play a role in amplification of symptoms. Rifaximin has recently been approved for treating IBS with diarrhea, again supporting a mechanistic role for probiotics to address an underlying pathology of bacterial overgrowth. Treating these patients can sometimes be frustrating or disheartening because we have little to offer them and their condition is rarely emergent. Prescribing probiotics to this group of patients will likely improve their symptoms in the long run and allow you to offer something new, instead of simply discharging them with instructions to "stay well-hydrated and try an anti-diarrheal".
Dose, Duration, Type
Unfortunately, the best dose, duration, and type of probiotics for the aforementioned conditions is not yet understood. There are 4 main classes of bacteria commonly found in probiotics:
- Lactobacillus/ Bifidobacterium species (the most numerous gut flora)
- Saccharomyces boulardii
- Bacillus and other soil-based or spore-forming bacteria
- Escherichia coli
An additional challenge is that probiotics are not as regulated as pharmaceuticals, meaning that the contents and amount within each dose can vary. In individual studies, there are some suggestions about using different strains of bacteria for certain benefits, but no single strain has consistently demonstrated superiority.
Another constraint for inpatients receiving probiotics is the hospital's formulary. Most hospitals have few, if not only one probiotic selection available. With no data to support any particular bacteria, this can be simplified by default use of the probiotic your hospital has on formulary.
Regarding dosing, the highest dose available is safe if the patient can tolerate it. Most commercial brands have between 1-20 billion colony-forming units per capsule. The number of bacteria in the gut is estimated to be in the trillions, so even a "large" commercial dose (20 billion CFU) would have a small impact on the overall GI flora.
Safety
Probiotics are overwhelmingly safe. In the vast majority of studies with a placebo control, the control group had equal (and often more) adverse events that the probiotic group. Occasionally, certain strains are ineffective in relieving a patient's diarrheal symptoms. In that case, switching to another strain is often successful. There have been a few isolated case reports of bacteremia from probiotics, but these occurred exclusively in either severely immunocompromised patients or those with a known defect to the GI mucosa. While exceedingly rare in practice, this minimal risk can be mitigated by withholding probiotics in severely immunocompromised patients, such as those actively undergoing chemotherapy induction.
Conclusion
Probiotics are no longer a pseudoscience or "alternative" practice. They should be part of every physician's armamentarium. One evidence-based practice that you can start tomorrow is to prescribe probiotics with every antibiotic script that you write for a patient at risk for antibiotic-associated diarrhea. In addition, there are several conditions that we see often in the ED that may benefit and are unlikely to be harmed from probiotic administration: gastroenteritis, peptic ulcer disease, hepatic encephalopathy, and IBS.
References
1. Food and Agriculture Organization of the United Nations. Guidelines for the Evaluation of Probiotics in Food. Ontario, Canada: 2002.
2. Dominguez-Bello MG, De Jesus-Laboy KM, Shen N, et al. Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat Med. 2016;22(3):250-253.
3. Rettger LF, Levy WN, Weinstein L, Weiss JE. Lactobacillus acidophilus and its therapeutic application. New Haven, Connecticut: Yale University Press; 1935.
4. Pattani R, Palda VA, Hwang SW, Shah PS. Probiotics for the prevention of antibiotic-associated diarrhea and Clostridium difficile infection among hospitalized patients: systematic review and meta-analysis. Open Med. 2013;7(2):e56-e67.
5. Zmora N, Zilberman-Schapira G, Suez J, et al. Personalized Gut Mucosal Colonization Resistance to Empiric Probiotics Is Associated with Unique Host and Microbiome Features. Cell. 2018;174(6):1388-1405.e21.
6. Smith M. Probiotics Fail in Kids’ Acute Gastroenteritis. MedPageToday. May 7, 2018.
7. Allen SJ, Martinez EG, Gregorio GV, Dans LF. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev. 2010;11:CD003048.
8. Dalal R, McGee RG, Riordan SM, Webster AC. Probiotics for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;2:CD008716.
9. Hungin APS, Mitchell CR, Whorwell P, et al. Systematic review: probiotics in the management of lower gastrointestinal symptoms – an updated evidence‐based international consensus. Aliment Pharmacol Ther. 2018;47(8):1054-1070.