Preeclampsia is a life-threatening obstetric condition on a spectrum of hypertensive disorders in pregnancy. Can you determine which rare complicating factor is at play in this case?
Case
A 38-year-old G1P0 right-hand dominant female at 34 weeks and 3 days gestation with a history of hyperlipidemia presents to the ED at 7:15 pm as a stroke alert for expressive aphasia since 2 pm while eating dinner with family. Family describes it as “word salad." In addition, the patient complained of a left-sided headache shortly after the aphasia and dysarthria started. No history of hypertension, cardiac disease, diabetes, or pregnancy complications. The patient is being managed by Maternal-Fetal Medicine (MFM) given her advanced maternal age. The patient only takes prenatal vitamins. No alcohol, tobacco, drug use during pregnancy.
Upon the patient's arrival to the emergency department, Neurology and Obstetrics are at bedside evaluating the patient given she presents as a stroke alert in the third trimester. The patient is found to be hypertensive to 220/115 with a heart rate of 80 on arrival to the ED. On physical exam, the patient is well appearing. She has profound expressive aphasia and dysarthria with an inability to follow commands. No other neurological deficits noted (5/5 strength, no limb ataxia). NIH stroke scale (NIHSS) of 4 for level of consciousness (2pt) and best language (2pt) is given. The abdomen is gravid to the subxiphoid process. One plus pitting edema in bilateral lower extremities is noted without calf tenderness.
The patient is given hydralazine 10mg intravenously (IV) times three and magnesium sulfate IV for the presumptive diagnosis of preeclampsia with severe features and blood pressure improves to 164/94 with no change in neurological status.The patient was taken to the OR for an emergent cesarian section secondary to a non-reassuring fetal heart rate. Post-operatively, the patient was taken to the CT suite for the CT of the head without IV contrast in addition to a CT Angiogram (CTA) of the head and neck with intravenous contrast.

Figure 1. CT Head: Focus of hypoattenuation in the left temporo-occipital lobe which is better visualized on the CTA head/neck.
Figure 2. CTA Head
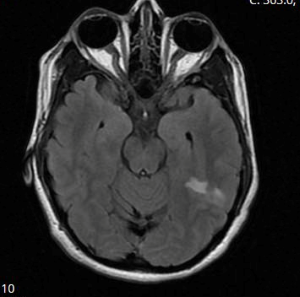
CTA Head Impression
- Moderate to severe diffuse narrowing of the M2 segment of the left middle cerebral artery with diminished contrast opacification of the distal cortical branches relative to the contralateral side. Overall, the significant vascular abnormalities on this study are most suspicious for an underlying process such as reversible cerebral vasoconstriction syndrome.
- Moderate irregular narrowing of the vertebrobasilar circulation which is most pronounced in the left posterior cerebral artery.
Discussion
Preeclampsia is a life-threatening obstetric condition on a spectrum of hypertensive disorders in pregnancy. Preeclampsia with severe features presents with signs of end-organ damage - which includes cerebral insult. Posterior Reversible Encephalopathy Syndrome (PRES) and Reversible Cerebral Vasoconstrictive Syndrome (RCVS) are considered to be two rare complications of preeclampsia. This discussion highlights preeclampsia and these two rare complications as well as the clinical and radiological difficulty in diagnosing these two conditions. After reviewing these conditions, you - the reader - will have the opportunity to decide if the patient suffered from a cerebrovascular accident, PRES, or RCVS.
Preeclampsia
Preeclampsia is a hypertensive disorder of pregnancy diagnosed after 20 weeks of gestation and up to 4 weeks postpartum. It is theorized to be caused by maternal and fetal vascular dysfunction. Diagnosis is by an elevated blood pressure greater than 140 systolic and/or greater than 90 diastolic OR proteinuria greater than 0.3g in 24 hours.
Risk factors include advanced maternal age, chronic kidney disease, twin gestation, antiphospholipid antibodies, first pregnancy, past medical history or family history of preeclampsia, BMI >26.1, or a nulliparous state.
Clinical features of preeclampsia include headache, visual changes, epigastric/RUQ pain, elevated blood pressure, peripheral edema, pulmonary edema, altered mental status, and lab abnormalities (acute kidney injury (AKI), AST/ALT elevation, Uric acid elevation, and proteinuria).
Preeclampsia is managed with blood pressure maintenance with antihypertensives such as labetalol, hydralazine, nifedipine, or methyldopa. To prevent the progression of preeclampsia to eclampsia (above findings + seizures), seizure prophylaxis is achieved through magnesium sulfate with an initial 4 gram loading dose IV followed by a 2 gram per hour IV infusion to maintain magnesium level between 4.8 to 8.4 for 24hrs postpartum - and delivery if emergent.
Reversible Posterior Leukoencephalopathy Syndrome
A clinical radiographic syndrome of heterogenous etiologies that are grouped together because of similar findings on neuroimaging studies - Posterior Reversible Encephalopathy Syndrome (PRES), Reversible Posterior Cerebral Edema Syndrome, Posterior Leukoencephalopathy Syndrome, Hyperperfusion Encephalopathy, or Brain Capillary Leak Syndrome. Despite the name, the syndrome is not always reversible and it is not confined to either the white matter or posterior regions of the brain — though it is unclear why there is primary involvement of posterior brain regions.
The syndrome is most commonly seen in hypertensive encephalopathy, eclampsia, and with the use of cytotoxic and immunosuppressant drugs (cisplatin, cyclosporine). It is also noted to be most common in women and all age groups are susceptible. Other conditions noted to be associated with RPLS include AKI, CKD, Sepsis, MultiOrgan Dysfunction, autoimmune diseases, and organ transplantation.
RPLS is characterized by an insidious onset of constant, nonlocalized headache unrelieved by analgesia, confusion or decreased level of consciousness, visual changes, and seizures associated with the posterior cerebral white matter edema seen on neuroimaging.
The pathogenesis is unclear, but it is thought that sudden blood pressure elevation causes cerebral autoregulation to exceed the upper limit and the arterioles dilate resulting in cerebral hyperperfusion, breakdown of the blood brain barrier and the extravasation of fluid and blood products into parenchyma. Cerebral ischemia can in turn occur due to focal vasoconstriction/vasospasm and hypoperfusion and resultant cytotoxic edema OR hydrostatic vasogenic edema and microcirculatory compression. This edema can increase cerebral perfusion pressure.
Preeclampsia and cytotoxic therapies may lead to capillary leakage and blood brain barrier disruption, axonal swelling, and trigger vasogenic edema. In preeclampsia, secretion of trophoblastic cytotoxic factors from poorly perfused fetal unit may provide an initial stimulus and result in elevated markers of endothelial damage. Some even suggest that RPLS could be considered an indicator of eclampsia- even when the other features of eclampsia (hypertension, proteinuria) are not present.
Diagnosis is by neuroimaging with symmetrical (subcortical) white matter edema in the posterior cerebral hemispheres - particularly the parieto-occipital regions- and it is usually not confined to a single vascular territory. RPLS can be picked up on CT, but it is best depicted by MRI. CTA and MRA studies have documented irregular vascular narrowing in medium to large-sized vessels in some groups. Resolution of neuroimaging findings is expected within days to weeks - suggesting edema rather than infarction.
Blood pressure should be lowered within two to six hours with easily titratable parenteral agents like nicardipine or labetalol - with the maximum initial fall not exceeding twenty-five percent of presenting value. Most seizures should be treated with phenytoin - except in the setting of eclampsia where treatment with magnesium and delivery of the baby and placenta are sufficient.
Prognosis in most case series and reports suggest that RPLS is fully reversible within a period of days to weeks and radiologic improvement lags behind clinical recovery. Rarely do patients survive with permanent neurologic disability.
Reversible Cerebral Vasoconstriction Syndrome
Also known as Call-Fleming Syndrome, Postpartum cerebral angiopathy, and CNS pseudovasculitis; Reversible Cerebral Vasoconstrictive Syndrome (RCVS) is a rare condition that occurs as the result of a sudden, transient, diffuse dysregulatory constriction of intracranial vessels producing the main feature of recurrent sudden, severe, and disabling headaches that are characterized as "thunderclap". Other symptoms associated with RCVS include vomiting, photophobia, phonophobia, visual changes, hemiplegia, ataxia, dysarthria, aphasia, and seizures.
Some risk factors proposed to cause these multifocal arterial vasoconstriction and dilations include preeclampsia and eclampsia, childbirth, hypercalcemia, vasogenic tumors, prescription and over the counter medications, and illicit drugs that cause vasoconstriction.
RCVS is most commonly found among women between the ages of 20 and 50 and is underdiagnosed because it mimics common conditions like migraines. PRES has a very similar presentation and is found in 10-38% of RCVS patients.
Routine blood tests, inflammatory markers, and cerebrospinal fluid analysis are typically normal in RCVS. CTA and MRA can identify seventy percent of cases by revealing diffuse reversible cerebral vasoconstriction that appear as "string of beads" on angiography with complete resolution within 1-3 months. Initial MRI is normal during the first week in 30-70% of cases; 10% of patients have MRI abnormalities consistent with PRES.
Currently, there is no approved treatment. Verapamil, nimodipine, and other calcium channel blockers may help reduce the intensity and frequency of the headaches. Triptans and ergot derivatives are contraindication as they have vasoconstrictive actions.
Prognosis is usually full recovery in most patients to permanent brain damage in others. All symptoms normally resolve within 3 months and may only last a few days.
Case Conclusion
A viable, 1660 g female infant was delivered with reassuring APGAR scores and transferred to the neonatal intensive care unit, where she did very well. The patient's creatinine and hemoglobin and hematocrit improved over the days while maintaining excellent urinary output.
Patient improved rapidly to where she felt she was back at baseline and was discharged home without home services on aspirin 81 mg, labetalol 100 mg twice daily, and Procardia XL 90 mg daily. Patient was scheduled for neurology follow-up.
Summary
Given the history and hospitalization course that this young primigravida female endured, it is quite possible these 3 processes are not independent and exclusive, but in fact a continuum of related processes. Our patient possibly experienced preeclampsia while at home that progressed to reversible cerebral vasoconstriction syndrome and PRES. The imaging performed as part of the broader work-up seem to reveal findings of both RCVS and PRES. We know these 2 conditions are likely associated with one another and are also associated with preeclampsia. Re-imaging and follow-up are necessary in order to establish the final diagnosis.