One of the rare but feared complications of oral contraceptive pills (OCPs) containing estrogen is hemorrhage from an enlarging hepatocellular adenoma.
The risk of developing hepatocellular adenomas in the absence of contraceptives is 1 in 1 million. However, the risk increases 30-40 fold with the use of OCPs,1 with the risk of significant bleeding ranging from 25-64%. Additionally, the larger the mass, the larger the risk of bleeding.2 In this case, we present a patient who suffered from the rupture of one of her hepatic adenomas while on Nexplanon® (etonogestrel), a progestin-only oral contraceptive that is implanted subdermally and lasts for up to three years.
Case
An 18-year-old female was referred to the ED from an urgent care facility with severe, constant, unrelenting back pain. On the urgent care provider’s initial assessment, the patient denied any abdominal pain. However, she had an episode of non-bloody, nonbilious emesis immediately upon palpation of her epigastrium.
At the urgent care facility, the patient’s laboratory studies revealed leukocytosis of 22,000 cells/mm3 and hypokalemia, with a potassium level of 2.8 mmol/L. Due to the concerning findings on initial assessment, the patient was transferred to the ED for further evaluation.
Upon the patient’s arrival to the ED, she reported severe abdominal pain that increased upon standing. The patient denied any relevant past medical or surgical history. When specifically asked, she denied any non-steroidal anti-inflammatory drug use, alcohol use, or family history of biliary colic. The patient’s only reported medication was a Nexplanon® implant.
The patient’s vital signs were within normal limits upon initial evaluation. Her exam was remarkable for severe epigastric and right upper quadrant abdominal tenderness with voluntary guarding. The patient's repeat complete blood count (CBC) revealed leukocytosis of 25,000 cells/mm3 with an elevated absolute neutrophil count to 20. Her hemoglobin was found to be 9.2 gm/dL with no baseline for comparison. Comprehensive metabolic panel revealed mild transaminitis with AST and ALT values of 149 IU/L and 176 IU/L, respectively. Potassium was found to be 3.3 mmol/L. In addition, the patient had an elevated alkaline phosphatase of 131 IU/L. Bilirubin was unremarkable. Urine studies revealed red blood cells, and a pregnancy test was negative.
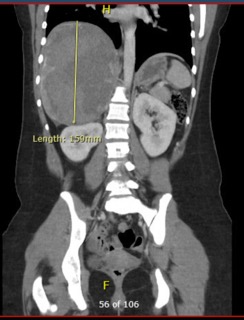
Point-of-care ultrasound of the patient’s right upper quadrant revealed a small amount of intra-abdominal free fluid in the right upper quadrant. Ultrasound did not identify any gallstones, pericholecystic fluid, or gallbladder wall thickening. However, there was an abnormal-appearing echogenicity to the liver (see figures). A stat CT scan of the abdomen and pelvis was ordered for further investigation.



While awaiting the results of the CT scan, the patient’s lactate was found to be elevated at 5 mmol/L. At that time, 2 L of normal saline was initiated.
CT scan results demonstrated a large hemorrhagic mass in the liver with contrast extravasation concerning for ruptured hepatic adenoma (see figures). Repeat CBC in the ED demonstrated a drop in hemoglobin from 9.2 gm/dL to 8.1 gm/dL.
Acute care surgery was consulted for further recommendations. The patient was then admitted to the hospital for serial hematocrit checks with plans to take her to the interventional radiology (IR) suite for embolization.
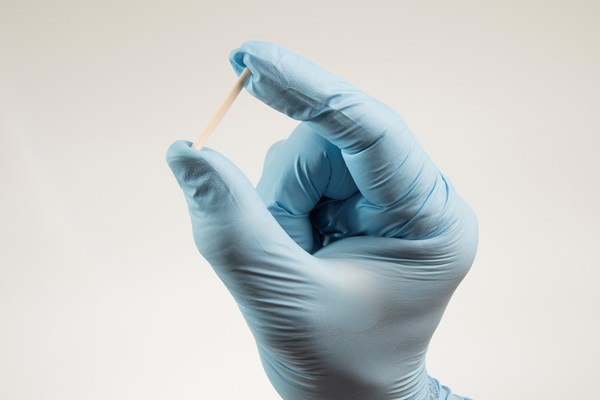
While admitted, the patient underwent Gelfoam® embolization of the right hepatic artery. The patient tolerated the procedure well and transitioned to oral intake prior to discharge the following day, with instructions to follow up with surgical oncology. Chart review performed after the visit revealed that the patient had Nexplanon® implantation four months prior to this incident. No previous history of hepatic adenomas was documented in her previous office visit notes between 2016 and 2020.
Discussion
Ruptured hepatic adenoma is an uncommon diagnosis in the ED and thus not often considered in the initial differential diagnosis for abdominal pain. However, this patient did have one risk factor that should raise every emergency physician’s clinical level of suspicion for this disease process: the use of oral contraceptives.
Hepatic adenomas are known to be either caused or exacerbated by estrogen-containing OCPs. However, this case features a patient who developed liver adenomatosis, defined as more than 3 adenomas, after the implantation of Nexplanon®, a progestin-only contraceptive rod.5
Section 5.7 of the package insert of Nexplanon® includes the following: “It is not known whether a similar risk exists with progestin-only methods like Nexplanon®.”6
We found one other case report in which a patient developed liver adenomatosis with bleeding. However, that patient was previously on an estrogen-containing OCP prior to having Norplant (another progestin-releasing implant) inserted. In this case, though, the patient was not on any contraceptives previously and had Nexplanon® inserted approximately four months prior to her ED visit. The case presentation is in contrast with the common teaching that patients on progestin-only contraception have little to no risk of enlarging hepatic adenomas.
Take-Home Points
As emergency physicians, our role is to manage multiple critically ill patients at any given time. Medication lists are an important part of medical history; yet they sometimes receive no more than a cursory glance, despite the risk of adverse reactions.
When considering young women with abdominal pain, asking about all forms of contraception may be crucial to arriving at the correct diagnosis. Many women, particularly those with implantable devices and not on daily medications, may forget to mention contraceptive use unless specifically asked.
References
- Rooks JB, Ory HW, Ishak KG, et al. Epidemiology of Hepatocellular Adenoma. The Role of Oral Contraceptive Use. JAMA 1979; 242:644.
- Bieze M, Phoa SS, Verheij J, et al. Risk factors for bleeding in hepatocellular adenoma. Br J Surg 2014; 101:847.
- Darney P, Patel A, Rosen K, et al. Safety and efficacy of a single-rod etonogestrel implant (Implanon): Results from 11 international clinical trials. Fertil Steril 2009; 91:1646.
- Daniels K, Abma J. Current Contraceptive Status Among Women Aged 15–49: United States, 2015–2017. NCHS data brief, no 327. Hyattsville, MD: National Center for Health Statistics. 2018.
- Suarez, A. A., Brunt, E. M., & Di Bisceglie, A. M. (2001). A 35-Year-Old Woman with Progesterone Implant Contraception and Multiple Liver Masses. Seminars in Liver Disease, 21(03), 453–460. https://doi.org/10.1055/s-2001-17559
- Nexplanon [Package insert]. N.V. Organon, Oss, The Netherlands, a subsidiary of Merck & Co., Inc.; 2020