Pregnancy comes with no shortage of potential complications. This 2018 Case-Con research summary offers insight into a severe postpartum condition to guard against.
Postpartum preeclampsia can result in severe long-term complications for a new mother. It is one of the most feared postpartum medical complications emergency physicians will encounter. Even more uncommon is the progression from seizures to intracranial hemorrhage. Early recognition of late onset eclampsia, defined as onset of seizures greater than 48 hours postpartum, is crucial in minimizing adverse outcomes. We present a case of a postpartum woman who developed late onset postpartum preeclampsia as well as subsequent intracerebral hemorrhage.
Case
A 24-year-old female, G1P1, 6 days postpartum presented to the emergency department with a chief complaint of headache for one day, unrelieved by over-the-counter acetaminophen. Initial blood pressure (BP) was 155/86 mm Hg. CT Head and CTA performed to rule out subarachnoid hemorrhage were normal. Patient was initially given Toradol IV, fluids, Compazine, and Sumatriptan with no improvement noted. On reassessment, BP was 206/97 mm Hg. Patient was started on Hydralazine IV, and labs were drawn which showed results consistent with preeclampsia. Obstetrics/ Gynecology (OB) was consulted to evaluate the patient, and treatment was continued with magnesium sulfate and additional IV hydralazine. Patient was admitted to (OB) service with a significant improvement in BP and headache relief. Patient was discharged home on oral Labetalol on hospital day 2 from the OB service.
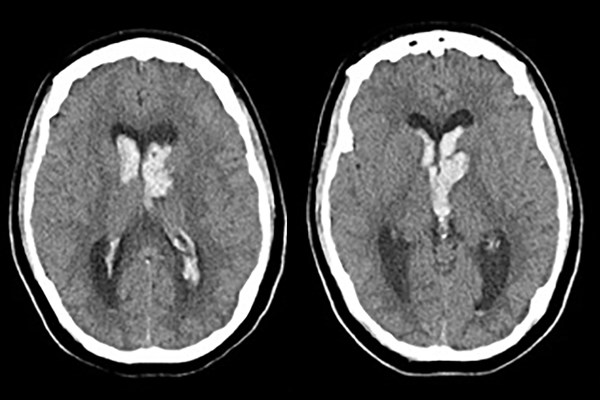
Less than 12 hours later, she was noted by her mother to be lethargic and with fixed eye deviation. She was taken to the same medical center and intubated on arrival for low GCS. Her BP prior to intubation was 187/89. CT head after intubation revealed left caudate intracerebral hemorrhage with intraventricular extension. The neurosurgery service immediately placed an external ventricular drain (EVD). Her BP was treated with a nicardipine infusion, and she was admitted to the neuroscience intensive care unit (NSICU) for management.
Blood pressure control was achieved. Her mental status progressively improved and she was extubated on hospital day 7 and the EVD removed on day 4. She was eventually discharged from the hospital with home OT/PT. Given her significant improvement, in-patient rehab was not recommended.
At her 2 month follow-up with neurosurgery, she had zero neurological deficits from her preceding intracerebral hemorrhage.
Discussion
Delayed postpartum eclampsia is uncommon, and can cause a diagnostic dilemma for emergency physicians. It is often overlooked as a differential diagnosis in postpartum women, especially those with an uncomplicated prepartum and antepartum course and no prior history of hypertension. Eclampsia can consist of many prodromal symptoms including headache, visual changes, right upper quadrant pain, and hypertension. Therefore, a differential diagnosis of postpartum eclampsia should always be considered in any postpartum woman who presents with these symptoms.1 Preeclampsia in the postpartum period is a serious diagnosis; if/when this diagnosis is made, aggressive treatment with antihypertensives and magnesium sulfate is indicated to minimize progression to eclampsia and possibly intracerebral hemorrhage.2 In this case, timely placement of external ventricular device (EVD) as well as aggressive management of the patient's hypertension ultimately resulted in a favorable outcome.
Conclusion
Postpartum preeclampsia is uncommon, and it can be easily overlooked as a diagnosis when a postpartum patient has no prior symptoms of preeclampsia.
At one time, it was thought that women could not develop eclampsia if they did not have preeclampsia during pregnancy; however, this has been found to be untrue. A review of the literature found postpartum eclampsia in a woman as far out as 8 weeks postpartum.3 We must be diligent when constructing a list of differentials for the postpartum patient. Any recently postpartum woman who presents with prodromal symptoms requires early detection and aggressive treatment of pre-eclampsia/eclampsia. This is critical in preventing adverse effects like intracranial hemorrhage.
References
1. Munjuluri N, Lipman M, Valentine A, Hardiman P, Maclean AB. Postpartum Eclampsia of Late Onset. BMJ. 2005;331(7524):1070–1071.
2. Townsend R, O’Brien P, Khalil A. Current Best Practice in the Management of Hypertensive Disorders in Pregnancy. Integr Blood Press Control. 2016;9:79-94.
3. Minnerup J, Kleffner I, Wersching H, Zimmermann J, Schabitz WR, Niederstadt T, Dziewas R. Late Onset Postpartum Eclampsia: It Is Really Never Too Late—A Case of Eclampsia 8 Weeks after Delivery. Stroke Res Treat. 2010;pii:798616.