Emergency contraception is a key intervention when treating sexual assault survivors. Two options are currently underutilized in the ED: ulipristal acetate and copper intrauterine device.
Case
A 17-year-old woman presents to the ED after being sexually assaulted while at a party approximately 36 hours prior. She believes she was drugged and does not recall most details of the incident. She is tearful, but otherwise uninjured. The patient is not currently using any form of contraception. In the ED the patient consents to a forensic examination. She is also provided with STI screening, empiric antibiotic prophylaxis, Hepatitis B booster vaccine, and counseling regarding the risk of HIV exposure. She also confirmed prior completion of the HPV vaccination series.1 She is concerned about pregnancy and wishes to discuss her options for emergency contraception. What would you tell her?
Introduction
The timely provision of emergency contraception (EC) for sexual assault survivors is a critical intervention for preventing unwanted pregnancy.2 While providing EC is the standard of care if there is any concern for pregnancy, counseling regarding the most effective methods as well as provision of those methods is highly variable among emergency physicians.3,4 A recent study of patients treated in pediatric EDs around the country found that 6% to 89% of patients were receiving STI and pregnancy testing and 0% to 57% were receiving all recommended prophylaxis, including EC.4 Another small survey from 2016 found that very few emergency physicians regularly offer the newly available and highly effective EC options to women.3 Specifically, this article highlights the 2 most effective methods of EC currently underutilized in the ED: Ulipristal Acetate and the Copper Intrauterine Device (Cu-IUD).
Types of Emergency Contraception
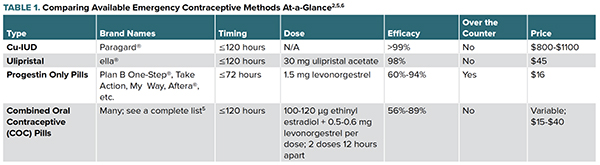
Four major types of EC are currently recommended by the American College of Obstetrics and Gynecology.2 Method choice may be based on institution-dependent practices, time since intercourse, method efficacy, availability over the counter or the woman’s individual long-term contraceptive and reproductive goals (Table 1).
A Note on Efficacy
No method of EC is perfect, and studies regarding the efficacy of each method are highly variable. In general, efficacy of all EC methods decreases as time since intercourse increases. All oral regimens have reduced efficacy in overweight and obese women; body mass index (BMI) has no effect on efficacy of the Cu-IUD.2,5
Nuts and Bolts
Cu-IUD
The Cu-IUD is currently being used off-label as EC. Insertion must be done by a trained provider. All OB/GYNs and an increasing number of primary care providers receive training in IUD insertion.7 The Cu-IUD is the most effective form of EC and will reliably prevent pregnancy for up to 10 years after initiation. Unlike other methods, its efficacy as EC is not lower in patients with high BMI.2 While insertion in the ED as EC is currently uncommon, emergency physicians may consider a consult to OB/GYN for patients who prefer this method.
Ulipristal Acetate
Ulipristal Acetate is the newest form of oral EC. Given its simplicity, efficacy and side effect profile, emergency physicians should strongly consider recommending this method before offering other oral regimens to patients.
Progesterone Only Pills
Progestin only pills are the over-the-counter option for EC, most commonly referred to as “Plan B.” They are available at Walgreens, CVS, Amazon, and any other major drugstore, and can be purchased by any individual. These pills are typically taken in a single dose.
Combined Oral Contraception Pills
Also called the Yuzpe regimen, this off-label method consists of taking a high dose of certain combined oral contraceptive pills that contain both Estradiol and Levonorgestrel. Depending on particular formulation, this method involves ingesting 4-6 pills (100-120 ug Ethinyl Estradiol and 0.5-0.6 mg Levonorgestrel) per dose. Two doses should be taken 12 hours apart. This is widely considered the least effective method of EC.
Adverse Effects
Cu-IUD insertion is typically accompanied by cramping; uterine perforation is a rare but serious complication (1/1000). Common long-term adverse effects include dysmenorrhea and heavy menstrual bleeding.2
Nausea, headache and irregular bleeding are common with all forms of oral EC. Nausea is most common with Combined Oral Contraceptive regimens. Less commonly women will experience dizziness, fatigue, breast tenderness and abdominal pain.2
Take-Home Points
- Emergency physicians are responsible for caring for women after some of the most traumatic experiences of their lives. Provision of EC is an essential component of post-sexual assault care, but highly effective methods are currently underutilized in the ED setting.3
- Ulipristal Acetate and the Copper IUD should be considered first line options for pregnancy prevention.
- Knowledge regarding all available options will allow emergency physicians to better counsel and care for their patients.
References
- 2015 Sexually Transmitted Diseases Treatment Guidelines: Sexual Assault and Abuse and STDs: Center for Disease Control and Prevention; 2015 [Available from: https://www.cdc.gov/std/tg2015/sexual-assault.htm.
- Practice Bulletin No. 152: Emergency Contraception. Obstet Gynecol. 2015 Sep;126(3):e1-11.
- Probst MA, Lin MP, Lawrence LG, Robey-Gavin E, Pendery LS, Strayer RJ. Survey of emergency physicians regarding emergency contraception. Am J Emerg Med. 2016 Jun;34(6):1176-8.
- Schilling S, Samuels-Kalow M, Gerber JS, Scribano PV, French B, Wood JN. Testing and Treatment After Adolescent Sexual Assault in Pediatric Emergency Departments. Pediatrics. 2015 Dec;136(6):e1495-503.
- Answers to Frequently Asked Questions About: Types of Emergency Contraception: Princeton University Office of Population Research; [updated February 22, 2019. Available from: https://ec.princeton.edu/questions/dose.html#dose.
- GoodRx [Available from: https://www.goodrx.com/.
- Chelvakumar M, Jabbarpour Y, Coffman M, Jetty A, Glazer Shaw J. Long-acting Reversible Contraception (LARC) Provision by Family Physicians: Low But on the Rise. J Am Board Fam Med. 2019 Jan-Feb;32(1):10-12.



