Want to contribute to our POCUS FTW series? Find out how.
Want to contribute to our POCUS FTW series? Find out how.
Case
A 55-year-old male presents to a community free-standing ED for lightheadedness. While checking in, the patient has a syncopal episode and begins vomiting. The patient is rushed to the resuscitation bay. The patient is tachycardic to the 120s but normotensive, afebrile, and satting 95% on room air. He is pale and diaphoretic with clear lungs and no murmurs on auscultation. He has good pulses throughout and no lower extremity edema. EKG is obtained revealing sinus tachycardia. Point-of-care ultrasound (POCUS) is immediately performed.
Parasternal short axis view with flattening of the interventricular septum throughout cardiac cycle
Apical four chamber view showing increased RV:LV size ratio, as well as McConnell's sign. Depth should be increased and probe angle decreased in order to visualize atria for true four chamber view
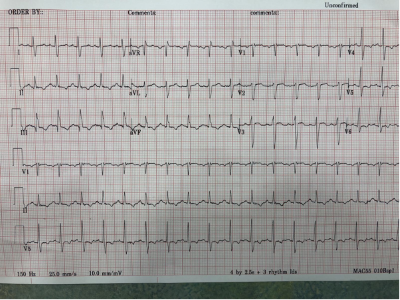
EKG demonstrating sinus tachycardia with S1Q3T3 pattern and right-axis deviation
Diagnosis: Pulmonary embolism (PE)
The above ultrasound clips demonstrate right heart strain. The parasternal short axis (PSSA) view shows a dilated right ventricle with flattening of the interventricular septum as it is pushed into the left ventricle, known as the “D-sign”. The apical four chamber (A4C) view further demonstrates “McConnnell’s sign” or right ventricular free wall hypokinesis with sparing of the apex. The dilated right ventricle relative to the left, or increased right ventricle to left ventricle (RV:LV) ratio, is also readily apparent on this view.
The finding of acute right heart strain in the absence of RV infarct or history of pulmonary hypertension, combined with the patient’s clinical picture, was concerning for pulmonary embolism. CT pulmonary angiography ultimately showed bilateral pulmonary emboli with a saddle component.
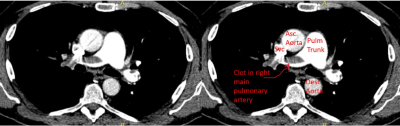
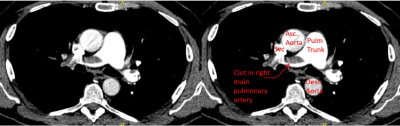
CT pulmonary angiography demonstrating filling defect consistent with pulmonary embolus
A note about S1Q3T3: while a “classic” pattern, the test characteristics for the pattern are not great with a sensitivity and specificity of only 54% and 62%, respectively.1 That said, the pattern does have some utility in prognostication with its presence predicting clinical deterioration and mortality.2
Ultrasound Review
Pulmonary embolism (PE) has an annual incidence ranging from 39-115 per 100,000 making it the third most common cardiovascular emergency behind myocardial infarction and stroke. With mortality rates of 3-15% and 25-50% for submassive and massive PEs, respectively, it is imperative to diagnose and treat rapidly.3
There are many patterns suggestive of right heart strain that are readily detectable with POCUS.4 In the absence of other causes of right heart strain such as right ventricular infarct or chronic pulmonary hypertension, these signs are very specific for PE. A 2017 systematic review and meta-analysis found that in patients being worked up for suspected PE, the “D-sign”, McConnell’s sign, and increased RV:LV ratio had sensitivities/specificities of 28% and 96%,19% and 98%, and 46% and 91%, respectively.5 A recent prospective observational trial found that sensitivity increased to 92% if there were any of these three signs and/or presence of tricuspid annular plane systolic excursion (TAPSE) <2.0 cm or any amount of tricuspid regurgitation in the setting of hemodynamic instability (heart rate >100, systolic blood pressure <90), although this increase in sensitivity did come at the expense of specificity which decreased to 64%.6
Check out this video for a walkthrough of the PE exam.
Back to the case
Right heart strain on point-of-care ultrasound together with the patient’s clinical picture were concerning for pulmonary embolism which was confirmed on CT angiogram shortly thereafter. Heparin drip was started within 30 minutes from patient hitting the door. Once stabilized, he was transferred to a tertiary care center where he underwent urgent mechanical thrombectomy and was discharged home after a short and otherwise unremarkable hospitalization.
To Probe or Not to Probe
POCUS is a quick, readily available tool that should be used to aid in the work up for PE, especially in the setting of hemodynamic instability. Evidence of acute right heart strain is highly specific for PE but importantly, the absence of these findings cannot rule out the diagnosis.
Take-home Points
- Pulmonary embolism is a life threat that must frequently be worked up in the ED.
- POCUS is a readily available tool to identify signs of right heart strain suggestive of PE.
- Rule out chronic causes of right heart strain by measuring the RV free wall (diameter >5 mm suggests chronic etiology).
- Other causes of right heart strain, such as RV infarction, must also be ruled out.
- Most POCUS signs associated with PE are very specific but lack great sensitivity.
References
- Ferrari E, Imbert A, Chevalier T, et al. The ECG in pulmonary embolism. Predictive value of negative T waves in precordial leads--80 case reports. Chest. 1997 Mar;111(3):537-43.
- Qaddoura A, Digby G, Kabali C, et al. The value of electrocardiography in prognosticating clinical deterioration and mortality in acute pulmonary embolism: A systematic review and meta-analysis. Clin Cardiol. 2017 Oct;40(10):814-824.
- Konstantinides S, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC), European Heart Journal, 2020;41(4): 543–603.
- Alerhand S, Sundaram T, Gottlieb M. What are the echocardiographic findings of acute right ventricular strain that suggest pulmonary embolism? Anaesth Crit Care Pain Med. 2021 Apr;40(2):100852.
- Fields J, Davis J, Girson L, et al. Transthoracic Echocardiography for Diagnosing Pulmonary Embolism: A Systematic Review and Meta-Analysis. J Am Soc Echocardiogr. 2017 Jul;30(7):714-723.e4.
- Daley J, Dwyer K, Grunwald Z, et al. Increased Sensitivity of Focused Cardiac Ultrasound for Pulmonary Embolism in Emergency Department Patients With Abnormal Vital Signs. Acad Emerg Med. 2019 Nov;26(11):1211-1220.