Periappendiceal abscesses are a rare complication of pediatric appendicitis.1
We present the case of an 11-year-old male who was evaluated in the pediatric emergency department for suprapubic pain, diarrhea, and fecal incontinence. Point-of-care ultrasound revealed a large lobular mass posterior and superior to the bladder, which was ultimately determined to be an abscess secondary to perforated appendicitis.
Case
An 11-year-old male presented to the pediatric emergency department (ED) for severe lower abdominal pain and diarrhea. Onset of pain was 2 months earlier and was initially intermittent, transitioning to persistent lower abdominal pain 2 weeks prior to presentation. The pain became severe after meals, and would sometimes wake him from sleep. 1 week prior to presentation he developed diarrhea, with several non-bloody liquid stools per day, which progressed to fecal incontinence. He reported that hunching over relieved the pain partially, and that he was urinating sitting down to avoid exacerbating the pain. Review of systems was positive for weight loss, as well as 2 days of subjective fevers and non-bloody, non-bilious emesis that resolved a week prior. There was no report of cough, congestion, odynophagia, polydipsia, polyuria, hematuria, urinary incontinence, weakness, numbness, or rash. There were no known sick contacts, and the patient was fully vaccinated. The patient had two negative COVID-19 tests in the past 3 weeks.
Vital signs at presentation to the ED demonstrated a temperature of 36.5°C, HR 90, RR 22, and BP 102/64. The patient was reclining on the bed. He had a thin habitus, and dry oral mucous membranes. Abdominal exam was significant for severe suprapubic tenderness with associated involuntary guarding, as well as moderate tenderness of the right and left lower quadrants. There was no costovertebral angle tenderness, hepatosplenomegaly, tenderness of the upper abdomen, inguinal lymphadenopathy, or signs of hernias or testicular torsion.
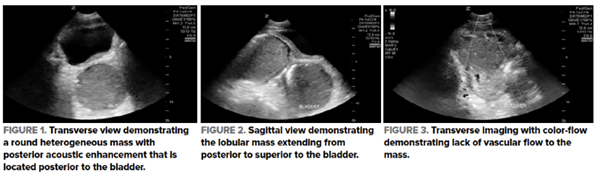
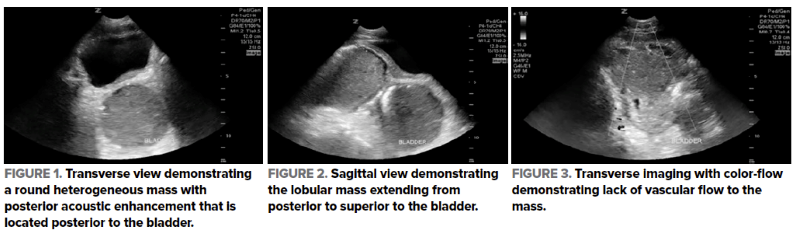
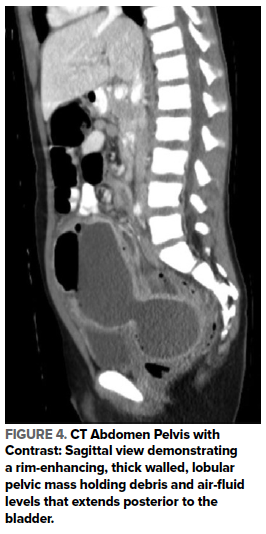
The differential diagnosis included urachal abscess, appendicitis, malignancy, and inflammatory bowel disease. POCUS performed by a third year pediatric emergency medicine fellow using a phased array transducer revealed a large, round, avascular mass posterior to the bladder that connected to a similar structure superior to the bladder. A large proportion of the mass was hypoechoic, with interspersed anechoic and hyperechoic elements (Figure 1, 2, 3). A radiology-performed abdominal ultrasound confirmed a well-circumscribed lobular mass that measured 12.3 x 5.0 x 7.0 cm, with heterogeneous echotexture and echogenic foci suggestive of air.
Serum testing was significant for an elevated white blood cell count 29.6 k/mm3 (range 4.1-10.1), 82% neutrophils, elevated immature granulocytes 2% (range 0-2), and an elevated C-reactive protein 95.4 mg/L (range <5). Urinalysis was significant for mild pyuria with 5-10 white blood cells/high power field (range <5) and elevated ketones.
An abdominopelvic computed tomography (CT) with contrast was obtained, confirming a lower abdominal and pelvic lobular, thick walled, rim-enhancing, complex fluid collection that was most consistent with an abscess. The mass held air-fluid levels and layered debris, and measured 14.2 x 5.2 x 8.4 cm. The structure was in contact with multiple loops of bowel, and was most likely secondary to a perforated appendicitis (Figure 4).
The patient was started on intravenous metronidazole and ceftriaxone, and he underwent CT fluoroscopic-guided drainage catheter placement with Interventional Radiology (IR). He was transitioned to oral Augmentin 2 days later to complete 2 weeks of antibiotics, was discharged on post-procedure day 3, and the drain was removed after 2 weeks.
Ultrasound Findings
Point-of-care ultrasound demonstrated a large, lobular mass in the lower abdomen. In the transverse view, this mass was visible posterior to the bladder (Figure 1). In the sagittal view, the mass visibly extended from posterior to superior to the bladder, and appeared structurally separate from the bladder (Figure 2). The structure was heterogeneous, with hyperechoic and anechoic foci, and demonstrated posterior enhancement (Figure 1, Figure 2). Using color Doppler, vascular flow was visible to the surrounding tissue and there was absent vascular flow to the mass (Figure 3).
Ultrasound Technique
POCUS for the evaluation of the pediatric abdomen is performed using the low frequency transducers to evaluate deep structures. Both the curvilinear and phased array transducers can be utilized in the pediatric abdominal ultrasound examination, and these transducers commonly include the frequencies 2-5 MHz and 1-5 MHz respectively.2,3 The curvilinear transducer gives the advantage of a larger footprint and optimal penetration, and is preferred in patients of larger body habitus for both superficial and deeper structures.2–4 The higher frequency linear transducer is favored for evaluating superficial structures; at greater depths it has reduced resolution.3,4 Water-based gel should be applied to the target area and the minimum pressure needed for visualization should then be applied to the transducer, to maximize patient comfort.3–5
Graded compression is performed to systematically evaluate the lower abdomen for appendicitis.5–7 In visualizing an abnormality in the abdominal or pelvic area on ultrasound, it is important to rotate the transducer 90° in order to evaluate two perpendicular planes.2,5,7
Abscesses are typically anechoic or hypoechoic in appearance, however the echotexture can also be heterogeneous. Abscesses can display septations, internal echoes, and posterior acoustic enhancement.3,4 Periappendiceal abscesses can additionally display hyperechoic foci due to air.7 The diagnosis of abscess is further supported by a swirl sign, which is a finding characterized by swirling purulent material with compression. Abscesses often display hyperemic tissues surrounding the cavity, with absent vascular flow to the cavity itself. It is important to evaluate the abscess using color Doppler as it aids in distinguishing it from a vascular or tissue malformation.3,4
Discussion
Abdominal pain is a common presenting complaint to the pediatric emergency department with an extensive differential diagnosis.8 Targeted imaging in conjunction with clinical exam findings can be used to rapidly narrow the potential etiologies and determine the optimal intervention.8,9 Ultrasound is recommended as the first line imaging for nontraumatic pediatric abdominal pain as part of stepwise clinical protocols designed to minimize radiation.10
While appendicitis is a relatively common pathology in the pediatric population, periappendiceal abscesses are rare.1 The incidence of appendicitis in the United States is approximately 1 per 1000, and 15-50% of pediatric appendicitis cases are perforated.11 However, the incidence of presentations of appendicitis complicated by periappendiceal abscess reached just 4.3% in one retrospective study.1 These abscesses may be constituted by single or multiple fluid collections, and sizes are cited as ranging as broadly as 3 to 1047.2 cm3 in children.1
Appendicitis is classically described as presenting with periumbilical pain that then localizes to the right lower quadrant, however patients may present with diffuse abdominal tenderness if there is appendiceal perforation.5,11 Examination findings may also demonstrate peritoneal signs such as guarding and rebound tenderness, and symptoms can include fever, anorexia, nausea, vomiting, and diarrhea.5,11
In our case, point-of-care ultrasound facilitated the diagnosis of a large abdominopelvic abscess secondary to appendiceal perforation for a patient with an atypical presentation. Point-of-care ultrasound identified our abnormal ultrasound findings 2 hours before the radiology-performed ultrasound occurred. Timely diagnosis of appendicitis is a known advantage of point-of-care ultrasound utilization, occurring an average of 2.5 hours earlier than radiology sonography in one prospective study.12 Additionally, when evaluating for appendicitis, point-of-care ultrasound performed by pediatric emergency physicians with focused ultrasound training has a sensitivity and specificity reaching 85 and 93 percent respectively.12
When ultrasound is non-diagnostic in the evaluation of abdominal pain for appendicitis, there should be consideration for abdominal CT or abdominal magnetic resonance imaging (MRI). CT has the benefits of reduced dependence on operator experience, as well as an elevated sensitivity and specificity of 90 to 97 percent and 91 to 99 percent respectively.8,13 MRI should also receive strong consideration given its lack of associated radiation, as well as its elevated sensitivity and specificity of 100 and 96 percent respectively.8,11,13
Treatment of appendicitis complicated by large abscess formation requires immediate empiric broad spectrum intravenous antibiotic coverage followed by IR percutaneous drainage. Elective appendectomy is performed several weeks after the acute episode to address the risk of recurrent appendiceal inflammation.1,11 In contrast, if the abscesses are small or are constituted by multiple discrete fluid collections that would necessitate multiple drainage sites, the first line of management is intravenous antibiotics, with interval imaging to evaluate for improvement.1
Conclusion
Periappendiceal abscesses are a rare complication of appendicitis that can be detected early with targeted point-of-care ultrasound. The use of point-of-care ultrasound in our patient’s case enabled prompt detection, diagnosis, and intervention for a large abdominopelvic abscess secondary to perforated appendicitis.
Learning Points
- Appendicitis is classically described as presenting with periumbilical abdominal pain that migrates to the right lower quadrant, however patients may present with diffuse abdominal tenderness in cases of appendiceal perforation.
- Ultrasound is the first line imaging modality for nontraumatic paediatric abdominal pain, and point-of-care ultrasound can facilitate early diagnosis and escalation of patient care for appendicitis and its complications.
- Appendicitis complicated by large periappendiceal abscess is treated with broad spectrum intravenous antibiotics, percutaneous drainage, and interval appendectomy after recovery.
References
- Zhang Y, Stringel G, Bezahler I, Maddineni S. Nonoperative management of periappendiceal abscess in children: A comparison of antibiotics alone versus antibiotics plus percutaneous drainage. J Pediatr Surg. 2020;55(3):414-417. doi:10.1016/j.jpedsurg.2019.09.005
- Dawson M, Mallin M. Introduction to Bedside Ultrasound: Volume 1. Emergency Ultrasound Solutions; 2013.
- Ma OJ, Mateer JR, Reardon RF, Byars D V., Knapp BJ, Laudenbach AP. Ma and Mateer’s Emergency Ultrasound. 4th ed. McGraw-Hill; 2020.
- Mallin M, Dawson M. Introduction to Bedside Ultrasound: Volume 2. Emergency Ultrasound Solutions; 2013.
- Katz Lavine E, Saul T, Frasure SE, Lewiss RE. Point-of-Care Ultrasound in a Patient With Perforated Appendicitis. Pediatr Emerg Care. 2014;30(9):665-667. doi:10.1097/PEC.0000000000000219
- Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986;158(2):355-360. doi:10.1148/radiology.158.2.2934762
- Gongidi P, Bellah RD. Ultrasound of the pediatric appendix. Pediatr Radiol. 2017;47(9):1091-1100. doi:10.1007/s00247-017-3928-4
- Smith J, Fox SM. Pediatric Abdominal Pain: An Emergency Medicine Perspective. Emerg Med Clin North Am. 2016;34(2):341-361. doi:10.1016/j.emc.2015.12.010
- Nicole M, Desjardins MP, Gravel J. Bedside Sonography Performed by Emergency Physicians to Detect Appendicitis in Children. Acad Emerg Med. 2018;25(9):1035-1041. doi:10.1111/acem.13445
- Niles LM, Goyal MK, Badolato GM, Chamberlain JM, Cohen JS. US Emergency Department Trends in Imaging for Pediatric Nontraumatic Abdominal Pain. Pediatrics. 2017;140(4):1-6. doi:10.1542/peds.2017-0615
- Rentea RM, St Peter SD, Snyder CL. Pediatric appendicitis: state of the art review. Pediatr Surg Int. 2017;33(3):269-283. doi:10.1007/s00383-016-3990-2
- Sivitz AB, Cohen SG, Tejani C. Evaluation of acute appendicitis by pediatric emergency physician sonography. Ann Emerg Med. 2014;64(4):358-364.e4. doi:10.1016/j.annemergmed.2014.03.028
- Quigley AJ, Stafrace S. Ultrasound assessment of acute appendicitis in paediatric patients: Methodology and pictorial overview of findings seen. Insights Imaging. 2013;4(6):741-751. doi:10.1007/s13244-013-0275-3