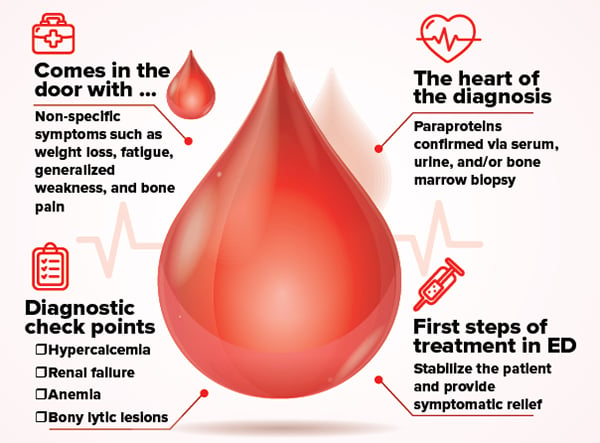
ED management of multiple myeloma should focus on medical stabilization and symptomatic relief. However, there are potential complications that require special consideration.
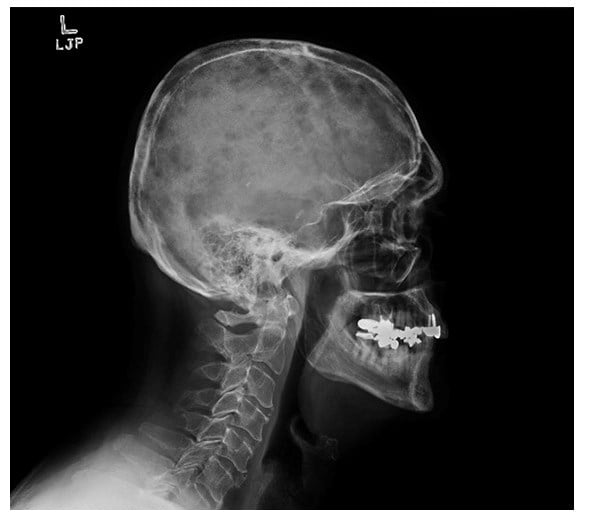
A 65-year-old male with a past medical history of peptic ulcer disease presents to the emergency department with 2 months of generalized weakness, constipation, and weight loss. Initial vitals include temperature 98.7 degrees Fahrenheit, heart rate 111, blood pressure 191/88, and oxygen saturation 98% on room air. On physical exam, he appears cachectic and ill-appearing. He has evidence of conjunctival pallor. His abdominal exam is positive for distention. He also has bony tenderness over the lumbar spine. Digital rectal exam reveals guaiac negative brown stool and normal rectal tone. Laboratory studies are significant for creatinine 15.9 mg/dL, calcium 13.4 mg/dL, hemoglobin 4.7 g/dL, and total serum protein 10.3 g/dL (normal range 6 – 8.3 g/dL). A skeletal survey performed in the ED demonstrates scattered lytic lesions and an L1 compression fracture. The patient receives resuscitation with intravenous fluids, analgesics, and 2 units of packed red blood cells. Nephrology and hematology are consulted and the patient is admitted with a presumed diagnosis of multiple myeloma.
Discussion
Multiple myeloma (MM) is a cancer of plasma cells that results in the production of abnormal antibodies (ie, paraproteins), which accumulate in the bone marrow and other vital organs. MM accounts for 1-2% of all cancers and results in approximately 106,000 deaths per year worldwide.1 It is known as a cancer of the elderly, with a median diagnosis age of 66 years. The precise etiology is unknown, but an increased incidence has been linked with environmental exposures including agricultural pesticides, sheet metal, and wood dust.2
Patients will often present with non-specific symptoms such as weight loss, fatigue, generalized weakness, and bone pain.3 A definitive diagnosis is rarely made in the ED but there are certain features of the disease that should raise your level of suspicion. The classic tetrad of hypercalcemia, renal failure, anemia, and bony lytic lesions are important components of the diagnostic criteria. Total serum protein is a nonspecific marker but an elevated level may suggest MM in the appropriate setting. In order to make a formal diagnosis, the presence of paraproteins must be confirmed via serum, urine, and/or bone marrow biopsy. This is often not an appropriate or feasible test to perform in the ED, so it is usually performed by the admitting medical team.
Management
ED management should focus on medical stabilization and symptomatic relief. However, there are potential complications that require special consideration.
Spinal Cord Compression
Although a rare occurrence, bony infiltration of the spinal column can result in vertebral fractures, spinal cord compression, and rapid progression to paralysis. Patients with a known or presumed diagnosis of MM who complain of back pain should undergo a thorough evaluation to assess for neurological deficits. If cauda equina is being considered, assessment of rectal tone, lower extremity reflexes, and sensory deficits of the perianal area should be documented. In patients with bladder dysfunction, a bladder ultrasound can be performed to assess for post void residual (PVR). PVR >50 mL (may be up to 100 mL in age > 65 years) is considered abnormal. MRI of the spine is the diagnostic modality of choice and prompt neurosurgical consultation is required in patients with suspected epidural involvement.4
Renal Failure
Acute kidney failure is a common complication and poor prognostic indicator in patients with MM. Renal dysfunction is caused by precipitation of paraproteins within the distal tubules as well as direct toxic effects to the proximal tubules and glomeruli. Adequate fluid hydration, correction of electrolyte derangements, and early consultation with nephrology are paramount. Some patients may arrive to the ED in extremis and will require dialysis on initial presentation.3
Hypercalcemia
Hypercalcemia is primarily caused by local osteolysis triggered by malignant plasma cells. Patients will present with symptoms of hypercalcemia: abdominal cramps, nausea, vomiting, constipation, and fatigue. Associated nephrocalcinosis (calcium deposition in kidneys) and dehydration further aggravates the overall decline in renal function. Characteristic EKG findings include QT shortening, AV blocks, QRS widening, and occasionally Osborn waves. Prior to initiating treatment, ionized calcium levels should be obtained as non-ionizing calcium can bind to paraproteins, resulting in a falsely elevated number. Intravenous fluid hydration, adequate analgesia, and cardiac stabilization should be the priority in the ED. Diuretics can be considered but only in patients with clear evidence of volume overload. In severe cases, bisphosphonates and calcitonin can be administered with guidance from nephrology.3
Hematologic Complications
Bone marrow infiltration can result in a wide array of hematologic abnormalities. Leukopenia and antibody dysfunction can increase the risk of life-threatening infections. Chemotherapeutic intervention further exacerbates immunosuppression leading to sepsis. Patients should be treated accordingly with fluid hydration and broad-spectrum antibiotics. Thrombocytopenia and anemia are also common, and patients may require appropriate transfusions to maintain hemodynamic stability. Finally, hyperviscosity syndrome can also occur secondary to aggregation of paraproteins within blood vessels. Patients can present with neurological symptoms ranging from a headache to a stroke. The paraproteins can also lead to coagulation pathway disruption which can result in spontaneous bleeding from mucous membranes. Treatments of choice include plasmapheresis and chemotherapy.3
Case Conclusion
During the patient’s hospital course, additional diagnostic testing was performed, which revealed a predominance of IgA in the serum and a bone marrow aspirate with 97% clonal plasma cells, confirming the diagnosis of multiple myeloma. He received intravenous bisphosphonates for hypercalcemia and an additional two units of packed red blood cells for persistent anemia. He was started on chemotherapeutic medications that consisted of cyclophosphamide, dexamethasone, and subcutaneous bortezomib. He remains hemodialysis-dependent.
C.R.A.B. Symptoms
● Calcium Elevation
● Renal Insufficiency
● Anemia
● Bone Lytic Lesions
References
1. Rajkumar SV. Multiple myeloma: Clinical features, laboratory manifestations, and diagnosis. UpToDate. https://www.uptodate.com/contents/multiple-myeloma-clinical-features-laboratory-manifestations-and-diagnosis.
2. Memorial Sloan Kettering Cancer Center. Multiple Myeloma Risk Factors. https://www.mskcc.org/cancer-care/types/multiple-myeloma/multiple-myeloma-risk-factors.
3. Xiao J, Todd BR. Multiple Myeloma Emergencies. emDocs. http://www.emdocs.net/multiple-myeloma-emergencies/.
4. Swaminathan A. Cauda Equina Syndrome. REBEL EM blog. https://rebelem.com/cauda-equina-syndrome/.