A 21-year-old female, G3P103, presented to the emergency department with a chief complaint of one month of right lower quadrant (RLQ) abdominal pain and one day of hematuria.
The pain was constant, described as a “ball of pressure,” with occasional sharp shooting pain provoked by position change. She had no relief with ibuprofen. She also reported associated nausea, headaches, and lightheadedness, but denied fever, chills, dysuria, vaginal bleeding, or vaginal discharge.
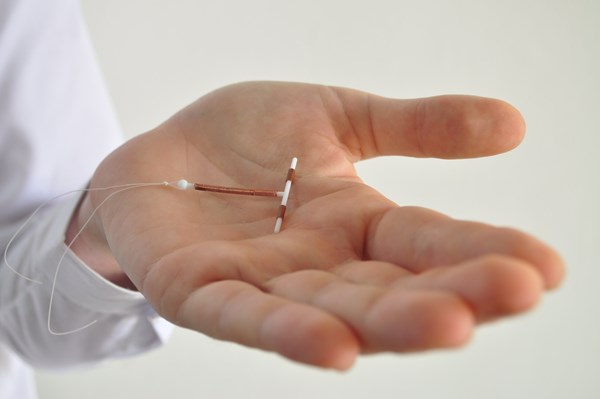
One month prior, she was seen in the ED for the same pain but had no hematuria. An ultrasound showed that her intrauterine device (IUD) was in the myometrium of her uterus, and a large left adnexal cystic structure from her left ovary had crossed into the right adnexa, measuring approximately 8.2 x 4.2cm. She was told to follow up with OB/GYN but could not schedule an appointment. A urinary tract infection (UTI) was also diagnosed during that visit. It was successfully resolved with cephalexin.
The patient's past medical history included a cesarean section eight months prior and two complicated preterm vaginal deliveries within the last three years. The IUD was placed two months after the C-section.
Initial vital signs in the ED included HR 78, BP 108/74, RR 18, temp 98.6°F, SpO2 100%, and BMI 43.62. Upon physical exam, the patient was in noticeable pain and had mild abdominal tenderness to deep palpation in the right lower quadrant (RLQ) without rebound, guarding, or CVA tenderness. On pelvic exam, an IUD string was seen in the cervix but no swelling, erythema, discharge, or lesion. The remainder of the physical exam was within normal limits. The urinalysis was normal. The pregnancy test was negative. A pelvic transabdominal and transvaginal ultrasound redemonstrated a malpositioned IUD extending into the myometrial wall and a large left adnexal cystic structure. OBGYN was consulted and attempted to remove the IUD in the ED, but was unsuccessful. Strings were visualized, grasped with ring forceps and gentle traction was applied but could not be removed. She was consequently admitted to have her IUD removed in the operating room (OR).
Discussion
Use of long-acting reversible contraceptive devices, such as IUDs, have increased dramatically in the past decade and therefore are seen more frequently in the ED. Serious complications are rare, but can include expulsion, pelvic inflammatory disease, contraception failure, ectopic pregnancy, and perforation.1
Uterine perforations are uncommon and occur in approximately 1 in every 1,000 insertions. Perforation rates are greater when insertion occurs less than eight weeks postpartum.2 It is possible that there is an association with perforations and scarred myometrium from cesarean deliveries and IUD placement while breastfeeding.3 A perforation can be complete or partial, fully entering the abdominal cavity or penetrating the uterine wall to varying degrees.4 Perforations can occur at the time of insertion or after the device has been successfully placed. Complete perforation will not protect against pregnancy and will frequently cause severe abdominal pain. The device is most commonly found in the Pouch of Douglas but can migrate in the abdominal cavity and attach to an organ, the bowel, the mesentery, and the omentum, resulting in further perforations and obstruction. Complete perforation, although unlikely, is very life threatening and must be addressed emergently.
Less severe and more frequently seen complications include malpositioned IUDs that are not perforating the myometrium, dysmenorrhea, amenorrhea, and normal pregnancy.5 Risk factors for malpositioning include obesity, prior uterine window or rupture, or copper IUD placement.6 Malpositioned IUDs are most frequently found in the lower uterus and can cause abnormal bleeding and pain,as well as increase the risk of pregnancy.7 Not all malpositioned IUDs require removal, but it is suggested due to possible lack of contraception.
A transvaginal ultrasound or, less commonly, a CT scan can accurately diagnose malpositioning. If the IUD has partially perforated the myometrium and the strings are visible, removal by pulling the strings should be performed. If it is not easily removed, then removal under anesthesia is generally indicated. This patient had several risk factors that could have influenced the perforation of her IUD, including placement within eight weeks of cesarean, breastfeeding during placement, and prior vaginal deliveries.


Case Conclusion
While in the hospital, the patient underwent a successful hysteroscopy and removal of the IUD. The IUD had partially perforated her myometrium but remained in the uterus. There were no further complications postoperatively, and the patient was subsequently lost to follow up. Although rare, complications with IUDs do occur and can require emergent diagnosis and management. ED physicians should consider IUD complications in patients who present to the ED with abdominal pain, and note that patients may not voluntarily report an IUD as part of their medical history unless specifically asked.
References
- Pocius KD, Bartz DA, Schreiber CA (Ed), Eckler A (Ed). Intrauterine contraception: Management of side effects and complications. UpToDate. 2021.
- Ramos-Rivera M, Averbach S, Selvaduray P, Gibson A, Ngo Ll (2021). Complications after interval postpartum intrauterine device insertion. American Journal of Obstetrics & Gynecology. 2021.
- Cheung ML, Rezai S, Jackman JM, et al. Retained Intrauterine Device (IUD): Triple Case Report and Review of the Literature. Case reports in obstetrics and gynecology. 2018; 9362962.
- Rowlands S, Oloto E, Horwell DH. Intrauterine devices and risk of uterine perforation: current perspectives. Open Access J Contracept. 2016;7:19–32.
- Berenson AB, Tan A, Hirth JM, Wilkinson GS. Complications and continuation of intrauterine device use among commercially insured teenagers. Obstetrics and gynecology. 2013;121(5):951–958.
- Connolly CT, Fox NS. Incidence and Risk Factors for a Malpositioned Intrauterine Device Detected on Three-Dimensional Ultrasound Within Eight Weeks of Placement. Journal of Ultrasound in Medicine. 2021.
- Wildemeersch D, Hasskamp T, Goldstuck N. Malposition and displacement of intrauterine devices–diagnosis, management and prevention. Clin Obstet Gynecol Reprod Med. 2016;2(3)183-188.