CASE
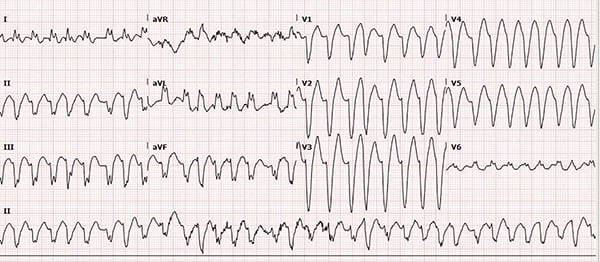
A 39-year-old female with no prior cardiac history presents with palpitations. What is your interpretation of the following ECG, and how would you treat this patient?
ANSWER
The ECG shows an irregular wide-complex tachycardia with a ventricular rate of ~192 bpm, left axis deviation, and a left bundle branch block pattern. The absence of P-waves or flutter waves narrows the differential (see Learning Points) to atrial fibrillation with aberrant conduction or polymorphic VT (PMVT). The LBBB pattern suggests a supraventricular origin and makes PMVT less likely. There is some subtle variability in the QRS morphologies with ventricular rates up to 300 bpm, which should raise suspicion for the presence of an accessory pathway (AP) and the possibility of AFib with WPW.
To help distinguish between AFib with a rate-related BBB and AFib with WPW, it is critical to review prior ECGs for conduction abnormalities (BBBs) and signs suggesting WPW (eg, delta wave). This is important because treatment with AV nodal blockers should be avoided in AFib with WPW.
When in doubt, the safest treatment options for hemodynamically stable patient with an irregular WCT are electrical cardioversion and procainamide.
Why to avoid AV nodal blocking agents in AFib with WPW?
To answer this, it necessary to understand the fundamentals of cardiac conduction. Anterograde conduction is toward the ventricle and retrograde is away from the ventricle. An AP can conduct in either direction. Orthodromic conduction describes anterograde conduction via the AV node and retrograde conduction via the AP. In the absence of a pre-existing conduction abnormality (eg, BBB), the QRS will be narrow.
Antidromic conduction describes anterograde conduction via the AP and retrograde conduction via the AV node. Anterograde conduction via the AP leads to abnormal ventricular depolarization and a wide QRS. The participation of the AP in a reentry tachycardia is what differentiates AVRT from AVNRT (in which anterograde and retrograde conduction both occur within or around the AV node).
The importance of conduction via an AP in AFib is because of its short refractory period relative to the AV node. The ventricular rate in AFib is usually limited by the refractory period of the AV node. Nodal blockers will slow conduction through the AV node but not the AP. Since the AP has a shorter refractory period, atrial impulses can conduct at a much faster rate. This can lead to ventricular fibrillation, either because the impulse arrives during the vulnerable phase of the ventricular cycle or because the rapid ventricular rate causes such a low cardiac output that there is myocardial ischemia. In AFib with aberrant conduction, rates >~220 bpm suggest anterograde conduction via an AP as this exceeds the refractory period for the AV node.
Case Resolution
The patient was treated with amiodarone and spontaneously converted to a normal sinus rhythm with no signs of ischemia or abnormal conduction, supporting the final diagnosis of AFib with a rate-related LBBB. Labs, including electrolytes and troponin, were normal. She was admitted to the Cardiology service and an echocardiogram showed an ejection fraction of 35% with no mural thrombus. Myocardial perfusion studies showed global hypokinesis with no sign of ischemia, consistent with a tachycardia-related cardiomyopathy. She was started on a beta blocker and novel anticoagulant, and discharged with cardiology follow-up.
LEARNING POINTS
Irregular Wide Complex Tachycardia
- Rate >100 bpm, QRS >120 ms, and variable RR interval
- DDx includes:
- Atrial fibrillation with aberrant conduction (BBB or WPW)
- Atrial flutter with variable block and aberrant conduction
- MAT with aberrant conduction
- Polymorphic ventricular tachycardia
- Ventricular fibrillation
Tachydysrhythmias in WPW
- Can be narrow (orthodromic conduction via AV node) or wide (antidromic conduction via accessory pathway)
- WPW with orthodromic AVRT:
- Rapid, regular narrow complex tachycardia
- Treat like AVNRT (PSVT)
- WPW with antidromic AVRT:
- Rapid, regular wide complex tachycardia
- Can look like monomorphic VT- treat like VT
- WPW with atrial fibrillation
- Very fast, irregularly irregular tachycardia (ventricular rate typically 180-300 bpm)
- Variable QRS morphologies in any single lead (ie, beat-to-beat variation in QRS morphology)
- Often misdiagnosed as atrial fibrillation with aberrancy from BBB
- AV nodal blockers should be avoided; can precipitate ventricular fibrillation and cardiovascular collapse
Procainamide and cardioversion/defibrillation are safe treatment options for any wide complex tachycardia in a patient with WPW.
For more, see p. 24-32 of the EMRA EKG Guide.



