Case
A 32-year-old female presents to the ED with 7 days of worsening abdominal pain. She appears in pain and refuses to lay on her back or walk. She lays on her left side. Her vitals on arrival pulse 97, BP 103/57. Her pain is 10/10, constant, and nothing makes it better. She cannot pinpoint one location where it hurts the most. She denies fevers or chills. Upon chart review you find she is a G7P2032 with past medical history of treated PID. Her urine pregnancy test is positive, she did not know she was pregnant. What is your next step?
Introduction
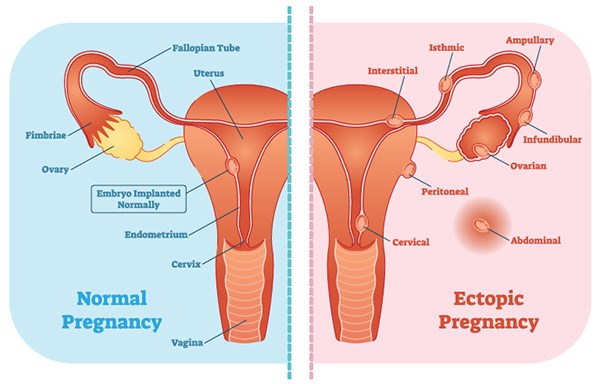
An ectopic pregnancy is simply an extrauterine pregnancy, accounting for 2% of all pregnancies.1 The vast majority (96%) occur in the fallopian tube, however other sites include the cervix, hysterotomy, ovary, or even abdomen. Very rarely, there can be both an intrauterine and ectopic pregnancy, which is coined a heterotopic pregnancy.2 Rates of ectopic pregnancies have been steadily increasing, however at least 40% of cases are initially misdiagnosed as a non-pregnancy condition or suspected intrauterine pregnancy (IUP).3 Failure to appropriately manage this common pathology leads to significant morbidity and mortality. In this article we will review the presentation, diagnosis, and approach to managing ectopic pregnancy.
Risk Factors
The biggest risk factor is previous ectopic pregnancy. Other major historical risk factors include uterine or tubal scarring from surgery (e.g. D&C, PID), increased maternal age, smoking, use of assisted reproductive techniques (ART) like in vitro fertilization.
Despite the popular misconception, IUD presence does not increase the overall risk of ectopic pregnancy, but a pregnancy with an IUD is more often an ectopic one.4
Presentation
Ectopic pregnancies can present in a variety of ways. Symptoms typically develop around 6-8 weeks after the last menstrual period. Women may misinterpret their vaginal bleeding as “normal menses”. Typical symptoms of pregnancy (breast tenderness, polyuria, nausea/vomiting) can also occur but with lesser frequency than IUPs, as the levels of human chorionic gonadotropin (hCG) are often lower.5,6
A retrospective cohort study in 2009 analyzed 2,026 females presenting to a US emergency department with a positive pregnancy test, vaginal bleeding, and/or abdominal pain. 18% (376 patients) had an ectopic pregnancy. Of those with ectopic pregnancy, vaginal bleeding was reported in 76%, and generalized abdominal pain in 66%.7 Importantly, there is no measured amount of bleeding that is associated more with ectopic pregnancy. Bleeding can range from scant to heavy. There is often non-focal tenderness on abdominal exam.
Even more fascinating, a population-based study in France looked at 849 tubal ectopic pregnancies and found the rate of tubal rupture to be 18% on presentation, so a high suspicion is warranted for potential decompensation.8
Multiple resources state that the diagnosis of ectopic pregnancy should be considered in any female with vaginal bleeding or abdominal pain- let’s expand on that. One must have a low threshold of thinking about ectopic pregnancy in any female of reproductive age. Given the high mortality and high rate of misdiagnosis, here’s some major complaints we always order a urine pregnancy test (UPT) for: syncope or near-syncopal symptoms, abdominal pain, chest pain, nausea/vomiting, dizziness, lightheadedness, or any GU complaint. This is by all means not a totally exhaustive list, but it does hit the highlights.
Important questions to ask a female with a +UPT include gravidity and parity, history of prior ectopic pregnancies, birth control status, usage of in vitro fertilization, prior history of STIs especially PID, and surgical history.
Pelvic exam has come under fire recently for suffering from relatively poor specificity and sensitivity, but it is still a necessary part of any GU workup. Your primary goal during the exam is to assess for the presence of bleeding, its quantity, and confirm that the uterus is the source of bleeding.
Diagnosis
Workup of ectopic pregnancy can quickly get algorithmic and tedious. Here is an overview to keep you grounded:

Relevant physiology
hCG is secreted into maternal circulation after implantation, about 6 days after ovulation. Normally, hCG should double ~48 hours during the first 30 days; decline is concerning for failed pregnancy. Traditionally, slower rise is concerning for ectopic pregnancy or early intrauterine demise, but hCG alone it is not confirmatory and there is no common predictable pattern of hCG in certain pathologies.9 In short, a single serum hCG level has very limited utility and it alone should not be used to make decisions (more on that below).10
Hemodynamically unstable
Here’s a shiny pearl: Females who are hemodynamically unstable with +UPT have an ectopic pregnancy until proven otherwise.
The most critical step is to perform a bedside basic gynecologic ultrasound (uterus, ovaries, cul de sac) with a FAST exam to look for free fluid, ovarian pathology, or intrauterine pregnancy (Figures 1 & 2).

Figure 1: TAUS Transverse view of the uterus and R ovary. Note the free fluid present surrounding the R ovary in the left aspect of the image, as well as the pseudogestational sac in the uterus on the right.

Figure 2: TVUS Sagittal view of the uterus demonstrating free fluid in the cul de sac.
All the while, you should follow aggressive resuscitation algorithms (2 large bore IVs, blood products), and promptly alert Ob/Gyn.
Hemodynamically stable
In those hemodynamically stable, there needs to be a complete, formal ultrasound. Transvaginal (TVUS) is the best test to effectively exclude an ectopic pregnancy.
There are 3 possible conclusions that can be drawn from the TVUS11:
Option 1: Gestational sac with a yolk sac or embryo in the uterus = IUP
Option 2: Gestational sac with or without yolk sac outside the uterus or echogenic extraovarian mass = ectopic pregnancy
Option 3: No pregnancy is identified = nondiagnostic
In confirmed ectopic cases, the most common finding is an extraovarian adnexal mass, at 89% of the time.
It is critical to recognize that the presence of an intrauterine gestational sac alone does not confirm an IUP! In fact, the presence of an intrauterine “sac-like” structure could actually be a pseudogestational sac, which is a collection of blood and hypoechoic fluid in the uterus that can be seen in ectopic pregnancy (Figure 1).12
A small amount of clear fluid in the pelvis is physiologic, but echogenic free fluid in a woman with +UPT is virtually diagnostic of ectopic pregnancy. In a prospective study, finding echogenic fluid has a sensitivity of 56% and specificity of 96% for predicting ectopic pregnancy.13
From the TVUS, if Option 1 occurs, ectopic pregnancy is effectively ruled out as the risk of heterotopic pregnancy is negligible in females not using assisted reproductive techniques. If Option 2, proceed with medical or surgical management of ectopic pregnancy by contacting Ob/Gyn.
Option 3 requires further workup. If no pregnancy is identified (either IUP or ectopic), it is likely because gestation is too early to be visualized on ultrasound. Transabdominal US (TAUS) can pick up an IUP at about 7-8 weeks; TVUS around 5 weeks. These patients will need close Ob/Gyn follow up with repeat hCG measurements and likely a repeat TVUS.14
What about the magical “discriminatory zone”?
The discriminatory zone is traditionally defined as the hCG level above which one should see an IUP via US. On average, this is about 2000 mIU/mL for TVUS (about 6000 for TAUS). Traditional teaching was that if a patient’s serum hCG was below the cut-off value and the US showed no IUP, there was a “decreased risk” for EP. This has been found to simply not be accurate and there are even some studies to suggest the opposite (i.e. increased risk for ectopic pregnancy).15 Therefore, we recommend not using the discriminatory zone alone to rule out ectopic pregnancy. There is no standard hCG level ectopic pregnancies are expected to present at. Remember, a single serum hCG level has very limited utility.
For patients with an elevated hCG, but a nondiagnostic US, this is a pregnancy of unknown location, and a wide range (8-40%) turn out to be ectopic. Call Ob/Gyn and arrange for follow up. The patient will need repeat hCG measurement in about 48 hours along with potentially repeating the TVUS (Figure 3). Serial hCGs that do not rise by about 66% in 48 hours is coined an abnormal pregnancy (ectopic or nonviable IUP). Besides stressing close Ob/Gyn follow up with the patient, strict return precautions should be given.

What about heterotopic pregnancies?
By definition this is a simultaneous IUP and ectopic pregnancy. This is a feared pathology that very rarely occurs. In fact, it is estimated to occur in 1 in 30,000 pregnancies.16 Therefore, in a female that has a confirmed IUP with no assisted reproductive techniques being used (ART), no further workup for heterotopic pregnancy need occur.
The risk of heterotopic pregnancy in those using ART is 1.5 per 1000 pregnancies.17 We predict this number to increase in the future as more and more patients are utilizing ART. Expect similar symptoms of ectopic pregnancy. In these patients, aside from an IUP, evidence of heterotopic pregnancy typically includes complex adnexal mass or fluid. They are often falsely labeled as a corpus luteum cyst.18 Ob/Gyn should be consulted early on to assist with this complicated pathology.
Treatment overview
If an ectopic pregnancy is confirmed, treatment discussion should obviously involve Ob/Gyn. All patients that are hemodynamically unstable, have significant free fluid on US, or have symptoms of rupture go to emergency surgery. That’s easy enough. In stable patients, methotrexate therapy has been found to be quite beneficial at reducing surgical exposure and its associated complications. There are strict indications and contraindications that must be reviewed, and OB/Gyn will obviously drive this discussion.
Case Conclusion
You perform a pelvic exam which is negative for bleeding or discharge. You perform a bedside TAUS to look for IUP and discover free fluid in Morrison’s pouch as well as a pseudogestational sac. As Ob/Gyn is urgently called, her repeat BP drops to 95/73 systolic and emergency blood products are hung. You place a 2nd large bore IV via US-guidance. Ob/Gyn urgently takes the patient to the OR where a ruptured ectopic pregnancy of the left ovary is found with a small hematoma. She recovers well and was discharged without incident.
Take-Home Points
-
Have a low threshold for ordering a urine pregnancy test, even if the chief complaint isn’t “GU related.”
-
A single serum hCG level has very limited utility and it alone should not be used to make decisions.
-
Females who are hemodynamically unstable with +UPT have an ectopic pregnancy until proven otherwise.
-
The most critical step in an unstable female with +UPT is to perform a bedside basic gynecologic ultrasound (uterus, ovaries) with a FAST exam.
-
If the TVUS is nondiagnostic in a stable patient, it is likely because gestation is too early to be visualized on ultrasound. Transabdominal US can pick up an IUP at about 7-8 weeks; TVUS around 5 weeks. These patients will need close Ob/Gyn follow up with repeat hCG measurements and likely a repeat TVUS.
-
There is no standard hCG level ectopic pregnancies are expected to present at. Do not let the “discriminatory zone” guide management. Remember, a single serum hCG level has very limited utility.
-
Assisted reproductive technologies raises the risk of heterotopic pregnancies.
References
- Seeber BE, Barnhart KT. Suspected ectopic pregnancy. Obstet Gynecol. 2006;107(2 Pt 1):399-413.
- Bouyer J, Coste J, Fernandez H, Pouly JL, Job-Spira N. Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod. 2002;17(12):3224-3230.
- Barnhart KT, Katz I, Hummel A, Gracia CR. Presumed diagnosis of ectopic pregnancy. Obstet Gynecol. 2002;100(3):505-510.
- Xiong X, Buekens P, Wollast E. IUD use and the risk of ectopic pregnancy: a meta-analysis of case-control studies. Contraception. 1995;52(1):23-34.
- Zou S, Li X, Feng Y, et al. Comparison of the diagnostic values of circulating steroid hormones, VEGF-A, PIGF, and ADAM12 in women with ectopic pregnancy. J Transl Med. 2013;11:44.
- Feng C, Chen ZY, Zhang J, et al. Clinical utility of serum reproductive hormones for the early diagnosis of ectopic pregnancy in the first trimester. J Obstet Gynaecol Res. 2013;39(2):528-535.
- Casanova BC, Sammel MD, Chittams J, et al. Prediction of outcome in women with symptomatic first-trimester pregnancy: focus on intrauterine rather than ectopic gestation. J Womens Health (Larchmt). 2009;18(2):195-200.
- Job-Spira N, Fernandez H, Bouyer J, et al. Ruptured tubal ectopic pregnancy: risk factors and reproductive outcome: results of a population-based study in France. Am J Obstet Gynecol. 1999; 180(4):938-944.
- Daya S. Human chorionic gonadotropin increase in normal early pregnancy. Am J Obstet Gynecol. 1987;156(2):286-290.
- Cole LA. Individual deviations in human chorionic gonadotropin concentrations during pregnancy. Am J Obstet Gynecol. 2011;204(4):349.e1-e7.
- Stein JC, Wang R, Adler N, et al. Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann Emerg Med.2010;56(6): 674-683.
- Atri M, Leduc C, Gillett P, et al. Role of endovaginal sonography in the diagnosis and management of ectopic pregnancy. Radiographics. 1996;16(4):755-774.
- Chen PC, Sickler GK, Dubinsky TJ, et al. Sonographic detection of echogenic fluid and correlation with culdocentesis in the evaluation of ectopic pregnancy. AJR Am J Roentgenol. 1998;170(5):1299-1302.
- Doubilet PM, Benson CB, Bourne T, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369(15):1443-1451.
- Condous G, Kirk E, Lu C, et al. Diagnostic accuracy of varying discriminatory zones for the prediction of ectopic pregnancy in women with a pregnancy of unknown location. Ultrasound Obstet Gynecol. 2005;26(7):770-775.
- Reece EA, Petrie RH, Sirmans MF, et al. Combined intrauterine and extrauterine gestations: a review. Am J Obstet Gynecol. 1983;146(3):323-330.
- Tal J, Haddad S, Gordon N, Timor-Tritsch I. Heterotopic pregnancy after ovulation induction and assisted reproductive technologies: a literature review from 1971 to 1993. Fertil Steril. 1996;66(1):1-12.
- Cheng PJ, Chueh HY, Qiu JT. Heterotopic pregnancy in a natural conception cycle presenting as hematometra. Obstet Gynecol. 2004;104(5 Pt 2):1195-1198.