Targeted temperature management has specific benefits for a variety of patients. But could therapeutic hypothermia be something to manage after a patient's death?
Case
You are called to the trauma room while on an overnight shift. A 52-year-old man became unresponsive during dinner. His family called 911. The paramedics arrive to your resuscitation room performing CPR on the patient. He is hooked up to a cardiac monitor and the rhythm shows asystole.
You begin resuscitation according to ACLS guidelines in an attempt to revive the patient. While he is being undressed, the nurse notes that the patient is wearing a necklace and bracelet engraved with the following:
IN CASE OF EMERGENCY CALL
800-XXX-XXXX. IN CASE OF DEATH PUSH 100,000U HEPARIN IV
DO CPR WHILE COOLING WITH
ICE TO 10 C KEEP PH 7.5
NO EMBALMING NO AUTOPSY
You have never seen this before. A social worker calls the number and it connects to an agent who informs you that the patient has an advanced directive, and he would like to preserved after death. He asks you to follow the aforementioned instructions while he dispatches a stand-by team to collect the patient and start their biostasis protocol.
On further inquiry, he informs you the patient is a member of a cryonics society. His goal is to be cryopreserved, in hopes that one day medical technology is advanced enough to revive him and bring him back from death. Your resuscitation attempts are unsuccessful, and the patient remains in asystole. What's your next step?
About Cryonics
Cryonics is the science of preserving human bodies with the hopes of one day being revived by advanced future medical technology. By being preserved in a state of suspended animation, patients who choose to undergo cryopreservation hope that the afflictions leading to their death can be managed successfully and they can resume their lives. Cryopreservation is achieved through a process of vitrification where high concentrations of chemicals called cryoprotectants, such as glycerol, replace the water in cells and tissue such that they can be cooled to temperatures below freezing. The process is similar to that used to preserve human embryos and sperm cells, but in this instance the entire body (or central nervous system) is preserved.
Once preservation is achieved by this process, patients are suspended in liquid nitrogen in long-term storage, where they will remain indefinitely until the day human medical knowledge will advance to a point where this process can be reversed. Cryonicists (as they call themselves) hope the medical technology of the future will be able to treat whatever medical problems the patients were afflicted with prior to their preservation, and lead to a more prolonged and fulfilling life.
Why Should We Care?
As much as this sounds like science fiction, there is a surprisingly significant number of people who have enrolled in such programs. As of September 2018, there exist about 2,704 individuals in the United States who are enrolled in programs offering cryopreservation.1,2
Additionally, 322 patients are currently cryo-preserved — and that number is expected to rise in the coming years. While there is much heated debate about this process in the scientific community, with most scientists labeling it pseudoscience and outside the realm of possibility, over the past decade many hospitals have been faced with the scenario in the case outlined above.3–7
Per published case reports, cryonics specialists often have to coordinate with hospital staff (mostly ICU or, in some cases, hospice) to set up equipment, initiate procedures, and transport the patient. It seems that hospital staff are usually aware that the patient has an advanced directive relating to this procedure, and often these patients have a DNR and a no-autopsy order. As patient enrollment rises, this scenario may become prevalent, and it is within the realm of possibility that emergency physicians will be faced with a situation completely foreign to them. As of yet, no cases have been reported in an emergency department.
Management in the ED or ICU
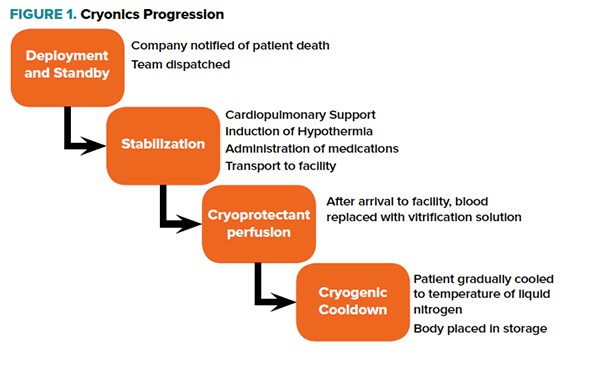
Going back to the case, the phone call the social worker placed would have alerted the staff at the cryonics facility. Depending on how imminent death is, a team is either placed on standby near the facility where the patient is admitted or directly dispatched to the site. In our case, the patient is being actively resuscitated with no appreciable rhythm, the team would have been dispatched directly (Figure 1).
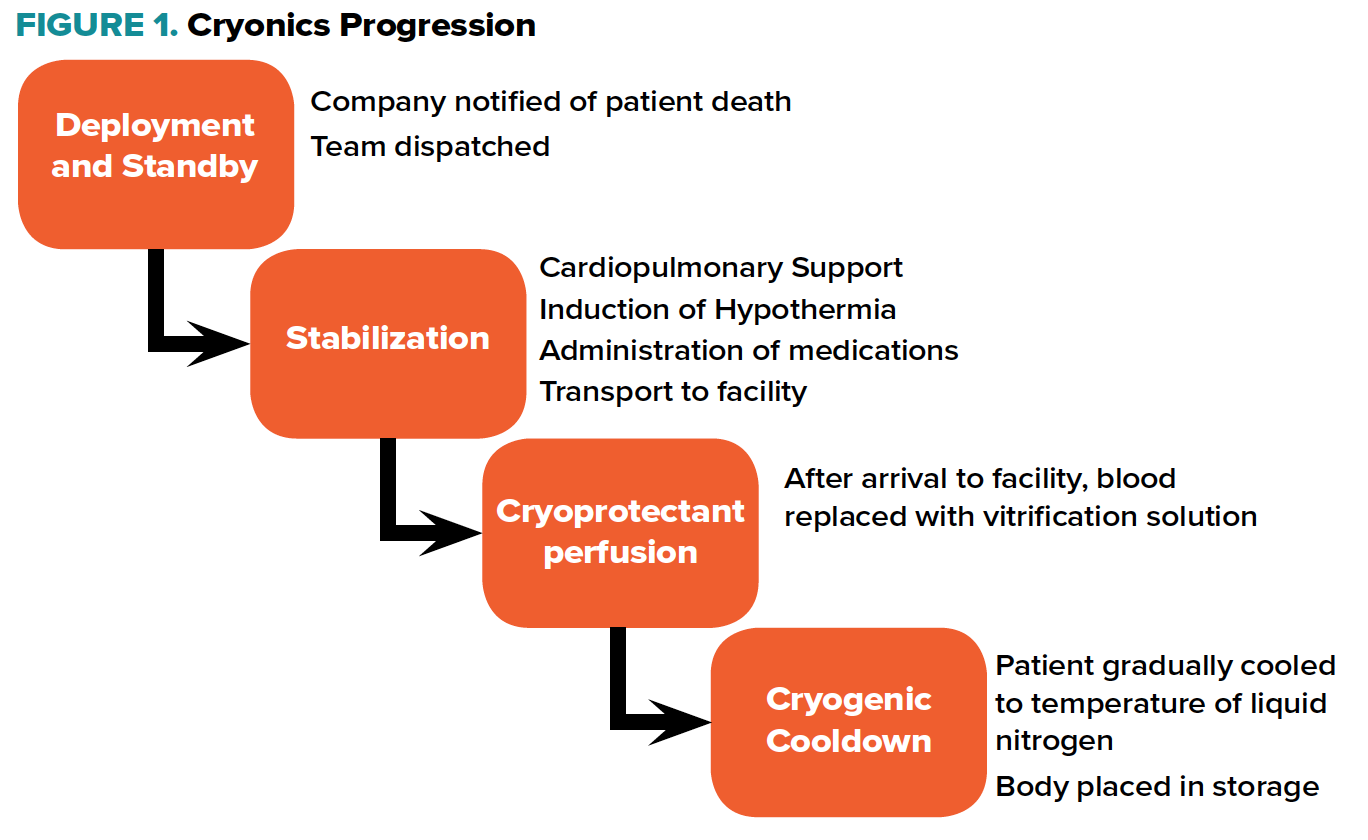
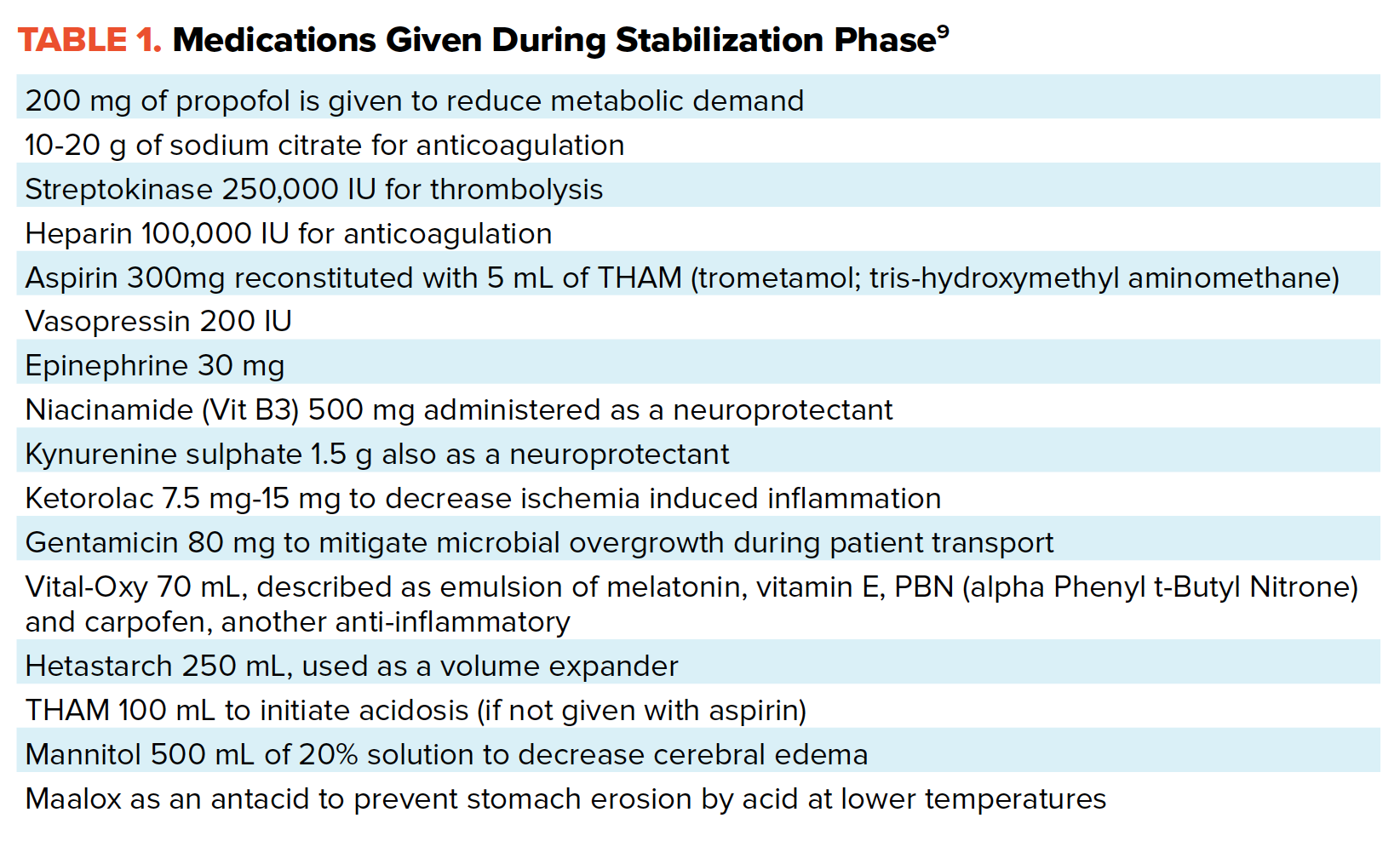
In the emergency department, after pronouncement of death, cardiopulmonary support would continue, preferably with a mechanical device. Cardiopulmonary support would start with mechanical devices such as a Lucas.8 At the same time, active external cooling would begin, at first with ice-packs and then placing the patient in a portable ice bath when it is ready. A whole automated regimen of medications is then administered to the patient, primarily to slow down the effects of ischemia, as well as anticoagulants and thrombolytics to prevent clot formation (see index for list of medications).
Once stabilized, the patient is transferred to the company's facility, where blood substitution with a cryoprotectant solution is performed. The major arteries and veins are cannulated, and blood washout occurs. The patient is then prepared for cryogenic cooldown. The temperature is dropped rapidly to -110C then slowly to -196C to prevent some of the effects of rapid cooling such as fracturing of brain tissue.
Once cryogenic cooldown is completed, the patient is placed inside a vacuum-insulated, liquid nitrogen filled Dewar (think large steel cylinder). The patient will remain in that Dewar until such a time when medical technology has advanced enough to allow for resuscitation and revival.9 There are obvious concerns about the process detailed above. Skeptics abound, and criticisms range from the very real scientific and logistical challenges, to more abstract ethical and even spiritual concerns.10,11,12
Previous experiences with cryonics have shown very real problems, and the process itself still needs an extreme amount of polishing.3–7,13,14 There exist, however, a significant number of people in the United States who have signed up to undergo this procedure. In a somewhat similar vein to how organ donation was practically unheard of some decades ago, it stands to reason that at some point an emergency physician somewhere in the United States will wander into unfamiliar territory when confronted with an unconscious patient who has signed up to be a cryonicist. In that situation, a strong argument can be made for respecting patients' autonomy, analogous to patients refusing autopsy for religious reasons, or refusing blood transfusion or porcine products.
The trickiness of the situation lies in advocating for the patient in the face of auxiliary staff, hospital administration and risk management. The emergent nature of cardiac arrest and in-hospital resuscitation brings forth the added challenge of immediacy and time constraints. Would there be enough time to negotiate with the hospital on behalf of the patient to allow a cryonics team onsite? In prior examples referenced, the patients were at hospice or long term care facilities, and arrangement were able to be made beforehand. However, preparation is made much more difficult if a cryonicist would succumb to acute life-threatening ailment at an unexpected time and locale. Could organ donation protocols be applied to these patients, in the sense that they could be treated as a whole body donor? These are very real questions that may become more pressing in the future as cryonics becomes more ubiquitous (if it ever does), but for now, we limit ourselves to engaging in the mental exercise, and wonder which one of us will win the lottery and be faced with this dicey situation.
References
1. Alcor. Alcor: Membership Statistics.
2. Cryonics Institute. Member Statistics | Cryonics Institute.
3. Standby CB, Leader T, and Standby MS. Alcor A-1088 Case Report. 2013.
4. Standby CB and Leader T. Alcor A-1349 Case Report. 2014.
5. ADrake. Alcor A-2605 Case Report. 2013.
6. Hixon H and Johanson S. Alcor A-2813 Case Report.
7. Gaspar C and Carvalho T. Alcor A-1497 Case Report. 2016.
8. Product specifications - LUCAS - Chest Compression System.
9. Alcor Life Extension Foundation Human Cryopreservation Protocol. 2016.
10. Hendricks M. The False Science of Cryonics - MIT Technology Review. MIT Technology Review.
11. Gorski D. Cold reality versus the wishful thinking of cryonics – Science-Based Medicine. Science Based Medicine.
12. Tarantola A. Why Freezing Yourself Is a Terrible Way to Achieve Immortality.
13. Standby CB, Leader T, and Standby MS. Alcor A-1088 Case Report. 2013.
14. Zahed R, Mousavi Jazayeri MH, Naderi A, et al. Topical Tranexamic Acid Compared With Anterior Nasal Packing for Treatment of Epistaxis in Patients Taking Antiplatelet Drugs: Randomized Controlled Trial. Acad Emerg Med. 2018.