Chances are you have seen a story in the media about a medical helicopter crash, often with fatalities to the crew and patient. But helicopter EMS (HEMS) is less dangerous than often portrayed, and safety is continuously being improved at all levels from the individual, aeromedical agencies, and national regulatory bodies.
The first use of HEMS dates back to World War II for aeromedical evacuation in Burma. HEMS use became routine during the Korean War and is credited with drastically reducing combat-related mortality.1 These findings prompted the adoption of HEMS into the civilian world, and its use has since evolved to hold an important role in both scene response and interfacility transport, with an estimated 400,000 medical patients flown each year in the United States.2
Even with the frequent use of HEMS, there is still no universal standard practice regarding their utilization. Providers often request HEMS out of the assumption that it will decrease out-of-hospital time and lead to better outcomes. Some of this misconception may come from the historical 60-minute threshold known as the “golden hour,” which was previously accepted in EMS and EM practice but has since faded as a standard of care. Some literature indicates that aeromedical transport improves morbidity and mortality in critically ill medical and trauma patients; however, conflicting studies show equivalent or poorer outcomes when compared to ground-based EMS (GEMS).3-7
When requesting HEMS, transport time should always be considered. A major benefit of HEMS is decreased travel time, since helicopters can fly a direct path and exceed the speed of GEMS. However, some aspects of HEMS take more time, which increases the total prehospital interval.6 Requesting a helicopter requires several steps, including a weather evaluation, flight planning, the crew being alerted, a pre.flight check, lift off, flight to the scene, landing, shutting down the aircraft, handoff, take off, return flight, landing, unloading, and possibly ground transport from the helipad to receiving facility. In many situations, GEMS units are more readily available and can complete the transport in a shorter period of time. Some of these delays can be mitigated by preplanning landing zones and flight paths, or avoided by standby activations for prolonged extrications or austere environment rescues. In these instances, HEMS response may be beneficial as time delays incurred by air transport occur before the patient is ready for transport. Critical patients can also be brought to the local ED for initial resuscitation with HEMS being dispatched to that ED to transfer to a tertiary center after the patient has been stabilized. This limits scene landings, which are higher risk than landing at an established hospital landing pad. HEMS often provides a higher level of care, especially in rural areas that may have only basic life support GEMS or rely on volunteers with variable levels of training.
HEMS typically operates as a nurse/paramedic team, may carry blood products, and have a scope of practice beyond GEMS advanced life support. This may include surgical airways, chest tubes, a wider range of medication, and the ability to care for patients requiring balloon pumps or ECMO.8-10 This expanded scope of practice may provide benefit for critically ill patients requiring interfacility transport; however, these same benefits may be obtained with lower risk using ground-based critical care transport teams.
Launching a helicopter involves a complex evaluation of risk and benefit. HEMS is both expensive, with each air medical transport costing between $12,000 and $24,000, and dangerous for patients and providers.11 It is impossible to remove all hazards from HEMS, but significant progress has been made over the past 5 years. The Federal Aviation Administration reported that HEMS accidents have been steadily decreasing since 2013, with 106 accidents and seventeen fatalities in 2016.12 This reduction is attributed to improved safety procedures, technological advances, and increased regulations. After increasing rates of aeromedical crashes in 2008 and 2009 with a total of 125 deaths in 20 years, the FAA revised its policies, releasing Final Rule 2010-0982 in February 2014. It mandates HEMS agencies to adopt enhanced procedures for flying in difficult weather, at night, and in remote terrain and required minimum standards for equipment including radio altimeters and terrain avoidance warning systems. The Final Rule increased training requirements for both pilots and crew members.13
Many HEMS agencies have individual policies in place to improve the safety of their crews and patients. A procedure used by many is “blinding,” where calls are dispatched to the crew without the nature of the call being given. This eliminates emotion as a motivator to accept a mission in conditions the crew would otherwise deem unsafe. When these details are relayed, many agencies continue to keep the pilot “blinded” in order to maintain objective operation of the aircraft. “All-or-none” policies, in which every member of the flight crew must individually agree to fly before the aircraft takes off, are also popular.14 This allows for the entire crew to evaluate the risk without fear of peer pressure or repercussion. Other policies attempt to combat “helicopter shopping,” where providers may contact a competing HEMS agency if declined by the in first agency due to weather or safety concerns.15 This is especially a concern among for-profit HEMS agencies, which have an additional pressure to increase helicopter utilization.16,17
Advances in technology are being incorporated to improve HEMS safety. Many HEMS agencies are now capable, meaning that the pilots are certified to operate the aircraft in low visibility situations with just the use of GPS and other instruments for navigation.16 Night Vision Imaging System, which consists of night vision goggles and lighting systems, improves the safety in operations, both in limited lighting and nighttime take-offs and landings.18 Wire Strike Protection Systems, known as “wire cutters,” have been implemented into civilian HEMS because 16% of fatal helicopter collisions involve a striking a telephone or power line, primarily during the descent to a non-established landing zone. Wire cutters, the specialized razor blades attached to the top and bottom of the aircraft, sever any wires the aircraft may contact. Studies by the U.S. Army have shown that this simple and inexpensive solution decreases crashes and mortality.19
Policy changes and technological improvement have decreased the risk of helicopter crashes – yet the risk can never be eliminated. Crew members wear a helmet and 5-point harness and sit in energy absorbing seats. Unfortunately, even with advancements in safety equipment, helicopter crashes still carry a high rate of mortality, especially for patients, who are more exposed.
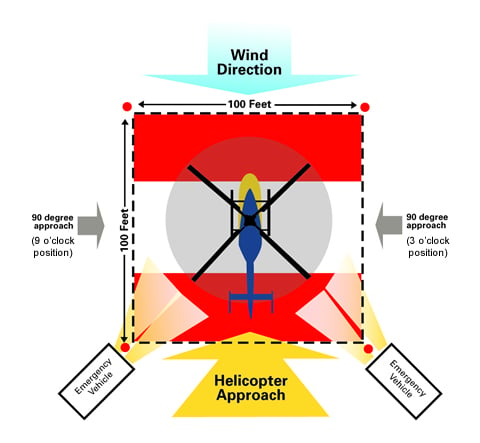
Providers can help improve HEMS safety. Ensuring a safe landing zone (LZ) is paramount to an efficient and safe transfer of care. (See Figure)
Most helicopters require a 100x100 ft flat area to land, with special attention to overhanging trees or electrical lines. Clear the area of any debris that may become airborne with the wind forces created during the landing. If the area is overly dry, it can be quickly wet down by fire services. In a fire or hazardous materials incident, the LZ should be upwind to prevent possible exposure. Ground crews should remain in contact with helicopter during approach and landing.
HEMS will never be risk-free, but great strides have been made to improve HEMS safety. Each day, more than 1,000 HEMS missions are flown, usually without incident. With continued advances, further research, and evidence-based guidelines for utilization, aeromedical transport will continue to improve medical care and transport.
References
1. Helicopter EMS: Part 1: A Brief History. EMS World. 13 Oct. 2010, www.emsworld.com/article/10319182/helicopter-ems-part-1-brief-history.
2. Fact Sheet and FAQs. AAMS. aams.org/member-services/fact-sheet-faqs/.
3. Abernathy M, et al. Reduce Inappropriate Helicopter Utilization in EMS. JEMS. 28 Feb. 2010.
4. Brown JB, Gestring ML. Does Helicopter Transport Impact Outcome Following Trauma? Trauma. 2013;15(4):279-288.
5. Galvagno SM, et al. Association Between Helicopter vs Ground Emergency Medical Services and Survival for Adults With Major Trauma. JAMA. 2012;307(15):1602-1610.
6. Pham H, Puckett Y, Dissanaike S. Faster on-Scene Times Associated with Decreased Mortality in Helicopter Emergency Medical Services (HEMS) Transported Trauma Patients. Trauma Surg Acute Care Open. 2017;2(1).
7. Sewalt CA, et al. Letter to the Editor Regarding the Article: “Identifying Pre-Hospital Factors Associated with Outcome for Major Trauma Patients in a Regional Trauma Network: an Exploratory Study.” Scand J Trauma Resusc Emerg Med. 2017;25(1):113.
8. Darocha T, Kosinski S, Podsiadlo P, Jarosz A, Drwila R. EMS, HEMS, ECMO Center, ICU Team: Are You Ready for Hypothermic Patients? JACC: Heart Fail. 2016;4(10):829-830.
9. Guide for Interfacility Transport. Ems.gov, National Highway Safety Administration. 2006. www.ems.gov/pdf/advancing-ems-systems/Provider-Resources/Interfacility_Transfers.pdf.
10. Duke Life Flight. lifeflight.duhs.duke.edu/.
11. Consumer Alert: Understanding Air Ambulance Insurance. National Association of Insurance Commissioners.
12. U.S. Helicopter Accidents Decrease. FAA. 2017.
13. Press Release – FAA Issues Final Rule to Improve Helicopter Safety. FAA. 19 Sept. 2014.14. Hudson J. Trauma Junkie: Memoirs of an Emergency Flight Nurse. Firefly Books, 2010.
15. EMS Helicopter Shopping: Dead Wrong. EMS | Flight Safety Network. 2017.
16. Brynick M. Soaring Through the Clouds, Weather, or Not. Air Care.
17. Hawryluk M. Rapid Growth in Air Ambulance Industry Raises Safety Concerns. The Bulletin. 2014.
18. Pope S. Rethinking the Safety of Medical Helicopters. Flying Magazine.
19. 7 Technologies That Can Reduce Helicopter Accidents. EMS World. 2014.



