The ED diagnosis of blunt cardiac injury is difficult, as trauma patients often have various concomitant injuries that may serve as distractors.
Case
A 25-year-old man with no past medical history presented to the emergency department (ED) after a motor vehicle collision, following a 10-minute extrication period. He had obvious injuries to the scalp, face, right hand, and right lower leg. Initial vitals were heart rate of 68 bpm, blood pressure of 113/54 mmHg and respiratory rate of 19 breaths/minute with 100% SpO2. The primary survey did not warrant emergent intervention and the patient’s GCS (Glasgow coma scale) was 15. Focused Assessment with Sonography in Trauma (FAST) was normal, and the secondary survey demonstrated facial trauma, an obvious right lower leg deformity, chest wall tenderness, and multiple lacerations to the extremities.
Diagnosis
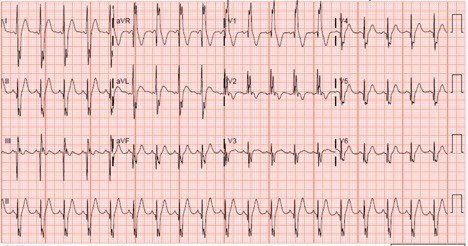
His initial 12-lead electrocardiogram (ECG) demonstrated sinus tachycardia with a right bundle branch block pattern, without historical comparison available (Figure 1). The ECG morphology raised concern for blunt cardiac injury (BCI) and cardiac enzymes were ordered. The initial troponin I and CKMB levels were 24.27 ng/mL (ref. <0,04 ng/mL) and 9.0 ng/mL (ref. </= 2.5 ng/mL), respectively.
An hour after presentation, the patient demonstrated tachycardia, and a repeat FAST demonstrated free fluid in the RUQ and LUQ. Computed tomography of the chest, abdomen and pelvis revealed liver and splenic lacerations and contusions. A plain radiograph revealed a comminuted right femoral shaft fracture.
The patient received emergent transfusion of packed red blood cells and was admitted to the trauma intensive care unit (ICU) for management and for monitoring of blunt cardiac injury with serial electrocardiograms and cardiac enzymes given the high risk for cardiovascular complications.
DISCUSSION
Echocardiography performed on admission revealed normal systolic function without ventricular wall abnormalities. However, previous studies have shown troponin elevations to be associated with increased mortality in blunt cardiac injury, whereas echocardiography has been less consistently correlated with cardiac complications.1,2 In this case, serial ECGs normalized over the course of admission, as the patient received blood transfusion and maintenance intravenous fluid in the ICU. The initial troponin I level was the peak value for admission and trended down with supportive care.
Blunt cardiac injury (BCI) is the result of a direct blow to the precordium or a sustained force to the chest wall causing compression of the heart between the spine and sternum, most commonly seen in the setting of motor vehicle collision or major thoracic injury.3,4 The ED diagnosis of BCI is difficult, as trauma patients often have various concomitant injuries that may serve as distractors. A lack of evident external thoracic injury or mild symptoms do not exclude the presence of BCI.3 The presenting symptoms in patients with BCI fall across a spectrum ranging from mild symptoms such as precordial pain and palpitations to hemodynamic instability and heart failure (tachycardia, hypotension, hypoxia).3,4
An elevated troponin level is an important diagnostic and prognostic marker for BCI.1 However, obtaining an ECG is important in the initial evaluation, with one series demonstrating that 88% of patients with BCI demonstrating abnormal EKG, defined as bundle branch block, T wave changes or ST segment changes.1 Cardiac injury to the left ventricle manifests as diffuse ST changes or pathological Q waves in contrast to the right ventricle which may manifest as right ventricular strain signs (such as right bundle branch block, as seen in this patient).3 The right ventricle is more commonly injured due to its anterior position in the thorax; injury to its smaller mass may create subtle ECG abnormalities which are easy to overlook.3,4
Take-Home Points
- Possible complications of BCI include ventricular dysrhythmias (usually within the first 24-48 hours), cardiac structural injury, or failure and cardiovascular collapse.2,4 One case series reported a mortality rate as high as 44% in those diagnosed with BCI.1
- A normal ECG alone is not sensitive enough to rule out BCI.2 However, emergency providers should understand the significance of abnormal ECG findings, some of which might otherwise be deemed insignificant, should prompt consideration of BCI in the appropriate clinical context.1,3 It is important to screen all patients who present to the ED with concerning mechanism or symptoms for BCI with an initial troponin level and an ECG; there is evidence that a normal ECG and cardiac troponin I have a 100% negative predictive value for BCI, though rarely a delayed rise in troponin may occur as late as at 8 hours.4,5
- Recognition of high risk electrocardiographic or clinical features should prompt further diagnostics or monitoring. This may include serial cardiac enzyme testing, echocardiogram or telemetry monitoring in order to identify and potentially intervene upon those with myocardial injury who are at risk for life-threatening complications.
REFERENCES
- Joseph B, Jokar TO, Khalil M, et al. Identifying the broken heart: predictors of mortality and morbidity in suspected blunt cardiac injury. The American Journal of Surgery. 2016;211(6):982-988. doi:10.1016/j.amjsurg.2015.10.027
- Kaye P. Myocardial contusion: emergency investigation and diagnosis. Emergency Medicine Journal. 2002;19(1):8-10. doi:10.1136/emj.19.1.8
- Sybrandy KC. Diagnosing cardiac contusion: old wisdom and new insights. Heart. 2003;89(5):485-489. doi:10.1136/heart.89.5.485
- Marcolini EG, Keegan J. Blunt Cardiac Injury. Emergency Medicine Clinics of North America. 2015;33(3):519-527. doi:10.1016/j.emc.2015.04.003
- Huis In ‘T Veld, MA, Craft CA, Hood RE. Blunt Cardiac Trauma Review. Cardiology Clinics. 2018;36(1):183-191. doi:10.1016/j.ccl.2017.08.010