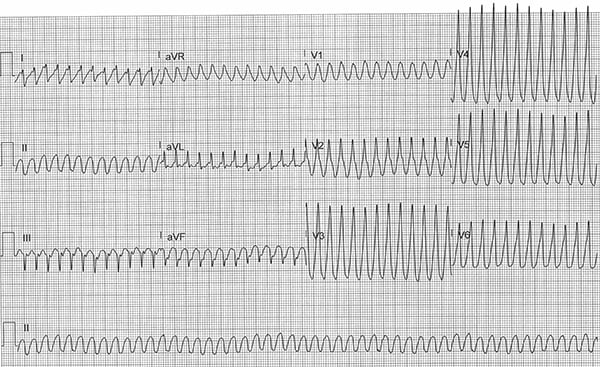
A 48-year-old male with a past medical history of asthma and recent positive COVID-19 test presents to the ED with acute onset of palpitations and chest pressure followed by a brief syncopal episode. What is your interpretation of his EKG?
Answer
This ECG shows a regular wide complex tachycardia with ventricular rate of 297 bpm, no discernible P-waves, northwest/extreme axis deviation (ie, between -90° and 180°), prolonged QRS complex duration of 157 msec, and positive QRS complex concordance in leads V1-V6 (ie, all of the QRS complexes are positively oriented).
The differential diagnosis for a regular wide complex tachycardia includes:
- Monomorphic ventricular tachycardia
- Antidromic AVRT
- Any regular SVT (sinus tach, AVNRT, atrial flutter, etc.) with aberrant conduction
- Causes of aberrant conduction include fixed or rate-related BBB, metabolic abnormalities, sodium channel blocker toxicity, ventricular paced rhythm, and ventricular pre-excitation (eg, WPW)
The EKG features that increase the likelihood of VT in a regular wide complex tachycardia include:
- QRS complex duration > 200 msec is almost always VT, hyperkalemia, or sodium channel blocker toxicity
- AV dissociation (ventricular rate > atrial rate)
- Positive or negative QRS complex concordance in leads V1-V6 (entirely or predominantly positive or negative QRS complexes from leads V1 to V6)
- Extreme axis deviation (also called "northwest axis")
- The absence of a typical RBBB or LBBB pattern suggests VT (ie, normal RBBB or LBBB pattern makes SVT with aberrant conduction more likely)
- Fusion beats: hybrid QRS complex formed by both supraventricular and ventricular focus
- Capture beats: sinus QRS formed by transient normal conduction amid AV dissociation
- Brugada's sign: time from the onset of the QRS complex to the nadir of the S-wave is > 100 msec
- Josephson's sign: notching on the downslope of the S-wave near its nadir
The findings in this EKG that suggest monomorphic VT include positive QRS complex concordance in leads V1-V6, northwest/extreme axis deviation, and the absence of a typical RBBB or LBBB pattern.
Case Conclusion
This patient's initial evaluation was notable for thready, but palpable, pulses with a systolic blood pressure of 90 mmHg. Given these findings in the setting of active chest pressure, the patient was treated with synchronized cardioversion. This was successful in converting the patient back to normal sinus rhythm, but only transiently, and he went back into monomorphic VT. He was cardioverted 2 more times, both only transiently successful, and also was treated with IV amiodarone (150 mg bolus followed by a drip) and 4 g IV magnesium sulfate.
Cardiology was consulted and started the patient on a continuous infusion of lidocaine for VT storm.
VT storm, also called VT/VF storm, electrical storm, or arrhythmic storm, refers to a state of cardiac electrical instability that is generally defined as ≥3 episodes of sustained VT, VF, or appropriate shocks from an ICD within 24 hrs.1 The patient eventually was stabilized on a continuous esmolol infusion, and a subsequent cardiac catheterization showed no significant coronary artery disease. He was admitted to the Cardiac ICU, and during his hospitalization had a cardiac MRI that showed delayed myocardial hyperenhancement consistent with myocarditis, likely caused by COVID-19.
Monomorphic VT Learning Points
- ≥ 3 consecutive, regular, wide complex beats with rate > 120-130 bpm
- Non-sustained: < 30 sec duration with no hemodynamic instability
- Sustained: ≥ 30 sec duration OR causes hemodynamic instability
- Rates < 120-130 bpm can be seen in patients on chronic antidysrhythmic medications (eg, amiodarone, flecainide, sotalol) or with severe cardiomyopathies
- For regular WCT with rates < 120 bpm, consider mimics:
- Hyperkalemia
- Sodium channel blocker toxicity
- Accelerated idioventricular rhythm (AIVR)
References
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2018;138(13):e272–e391.



