An elegantly simple proposal, the Acute Unscheduled Care Model, attempts to put emergency physicians back in the driver's seat of care while illustrating value within the health care delivery system.
“I’m sorry we didn’t find the reason for your abdominal pain today, but your work-up in the ED did not reveal any acute life-threatening illness. I’m glad you feel better; please follow up with your primary care doctor or return for any worsening symptoms.”
Raise your hand if that sounds familiar. Go ahead - we’ll wait.
Now, what if we told you that only 17% of those patients are able to follow up with their PCP within 7 days, and it takes 30 days for 83% of patients to get into their PCP’s office? That doesn’t even include the nearly 20%, according to some government surveys, of Americans who don’t have a PCP to begin with. What do you do with that information? More important, who is responsible for the care of these patients after they leave the ED? Well, if the ACEP proposal to CMS is approved, it just might be you.
The proposal, titled Acute Unscheduled Care Model (AUCM): Enhancing Appropriate Admissions, is meant to allow emergency physicians to participate in Alternative Payment Models (APMs) by accepting financial risk directly attributable to their discharge disposition decisions. While that may sound unnerving, it may actually be a blessing in disguise. Current value-based (aka cost-saving) payment models attempt to remove the emergency physician from patient care by curbing visits to the ED that insurance providers (cough-cough) deem “unnecessary.” This is done via coordinated outpatient care, which sounds great, but the outpatient setting is cracking and patients are continuously falling through these cracks. Pair that with the hot topic of balanced billing, and it seems that lately emergency physicians are being scapegoated for the rising costs of health care in America. This is where the AUCM (or “awesome’”) proposal comes into play, attempting to place emergency physicians back in the driver’s seat and providing us with the chance to prove our value within the health care delivery system.
At its core, the proposal is elegantly simple. It focuses on rewarding emergency medicine providers while simultaneously decreasing cost of health care delivery in 3 ways.
- First, it aims to reduce hospital inpatient admissions and observation stays by providing a safer discharge option.
- Second, it empowers providers to coordinate, manage and avoid unnecessary post-discharge services on a case-by-case basis.
- Third, it attempts to avoid post-ED visit patient adverse events (repeat ED visits, inpatient events, observation stays and death) and their inherent costs.
By doing so, it increases the “value” of care provided by emergency physicians. Essentially, the AUCM proposal makes ED providers and their facility responsible (for lack of a better word) for a discharged patient 30 days from their initial encounter.
We know what you’re thinking…sounds good in theory, but HOW?
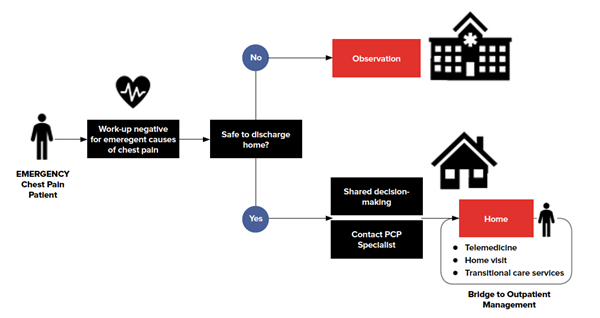
Keeping in mind that some details may change, the current proposal focuses on 4 chief complaints most ED physicians can approach in their sleep: chest pain, abdominal pain, syncope and altered mental status. Any patient checking into the ED with one of these 4 chief complaints will be eligible to enroll in the AUCM payment model up front. The final diagnosis in theory does not matter, although if your chest pain ends up being a STEMI, they would be pulled from AUCM. In fact, no patients admitted to inpatient or observation status would qualify under the current proposal. But the nearly 60% of chest pain patients discharged with a diagnosis of anxiety, costochondritis, GERD, or - our personal favorite - “non-cardiac chest pain”(thanks for being specific, doc), would fall into the model.
What does that actually mean?
Well, it means that instead of sending your patient out into the abyss, you would now have a tool set at your disposal to bubble wrap patients until they are back to their baseline. These tools, as proposed, include next-day telemedicine appointments, home visits by nurse practitioners/RNs, and other forms of transitional care, as well as care coordinators in the ED to help facilitate everything. This clearly comes with an initial financial investment. However, when that new cost is compared to the hospital’s current benchmarks for the same episodes of care, the upside is projected through the reduction of admission, readmission, and/or complication costs. The bottom line is if emergency physicians appropriately reduce unnecessary admissions, there will be a cost-savings, which by voluntarily participating in this awesome AUCM program, will be shared with ED providers.
Now, you may be reading this and saying, “But wait, I went into emergency medicine so I wouldn’t have to provide longitudinal care, and now you’re saying I may have to?” Recall that your purpose as a professional is to provide quality care. The proposed model does not, by any means, require you to establish lifelong relationships with your patients. Neither does it mandate that you adjust a patient’s insulin regimen 1 unit at a time until their HbA1c is just right (we got palpitations just writing that). What it does require, however, is for you to step up, be accountable, and ensure that patients do not fall through the cracks when they leave the walls of the department. The beautiful thing about emergency physicians is that we provide care to whoever, whenever, and wherever; not to whoever we prefer, whenever we see fit, and wherever it’s convenient. Traditionally, that care has been in the ED where we’ve served as a safety net for all, but now the safety net needs to expand beyond the ED. While that may seem like a tremendous burden, it actually provides our profession the opportunity to vastly increase our sphere of influence.
We pride ourselves on being go-getters, community leaders, problem-solvers, and innovators, and the AUCM proposal offers us a chance to once again prove our value. Sounds, well…awesome, doesn’t it?
Editor’s Note: This article, written by the 2019 recipients of EMRA’s EDPMA travel scholarship, is being simultaneously shared with the Emergency Department Practice Management Association.
The EDPMA is a trade association for emergency physician groups and their practice partners, such as billing and coding companies. EDPMA’s members deliver (or directly support) health care for about half of the 146 million patients that visit U.S. emergency departments each year. EDPMA advocates and educates on reimbursement that can sustain the delivery of high-quality, cost-effective care in the ED to an underserved patient population who often has nowhere else to turn. To learn more about the organization, visit their website at www.EDPMA.org.