Distal radius fractures are one of the more common fractures taken care of in the ED.
These occur in a wide variety of patients and often require manipulation or reduction in the ED prior to splinting. This reduction is one of the more painful procedures performed in the ED and, as such, has been associated with evolving analgesic procedures to assist in its successful performance. These procedures range from hematoma blocks to Bier blocks to procedural sedation. Reduction of distal radius fractures in the ED can be complicated if the patient has comorbid medical conditions such as polytrauma, hypotension, or traumatic brain injuries which can further complicate or limit the safety of procedural sedation.1 Recently, the utility of performing regional nerve blocks under ultrasound (US) guidance has gained popularity as it has the potential to combine adequate pain control with ease and efficiency in an ED setting.
While not widely studied, US guided Supracondylar Nerve blocks have been shown to be easily performed by an US trained physician in an ED setting with success rates as high as 95%.2 When compared to hematoma blocks, US guided supracondylar nerve blocks have been shown to significantly decrease pain scores pre-reduction, during reduction, and post-reduction.3 Although their utility in decreasing overall ED LOS has not been studied, it can be inferred from many related studies that utilizing regional anesthesia over procedural sedation may lead to significant decreases in ED LOS and improvement in patient satisfaction.4
Cadaver studies have shown that the majority of the distal radius is innervated by the posterior interosseous nerve, a branch of the radial nerve. Therefore, the supracondylar nerve block can theoretically provide adequate pain control for distal radius fractures. If adequate anesthesia is not achieved, adding a median nerve block can address any nerves (anterior interosseous nerve and median nerve) not anesthetized by the supracondylar nerve block.2,5
Ultrasound guided supracondylar blocks provide a motor and sensory blockade of the radial distal forearm. This anesthetic affect has been described as early as 15 minutes post-procedure with successful reductions taking place anywhere from 15-30 minutes post-procedure.6 No serious or long term complications have been described to date. These procedures can be performed by a single EP and do not require additional staff, monitoring, or resources associated with procedural sedation.
The Procedure
Materials Needed:
- US with linear probe
- 5-10 mL (milliliters) Anesthetic (Lidocaine, Bupivacane, or 1:1 mixture)
- 27 G Needle
- 20 or 22 G needle
- Sterile Gloves
- Sterile US probe cover
- Chlorhexidine or povidone Iodine
These should be performed under sterile technique with the use of povidone iodine or chlorhexidine, sterile gloves, and a sterile US probe cover.
Supracondylar Nerve Block
Step One: Positioning
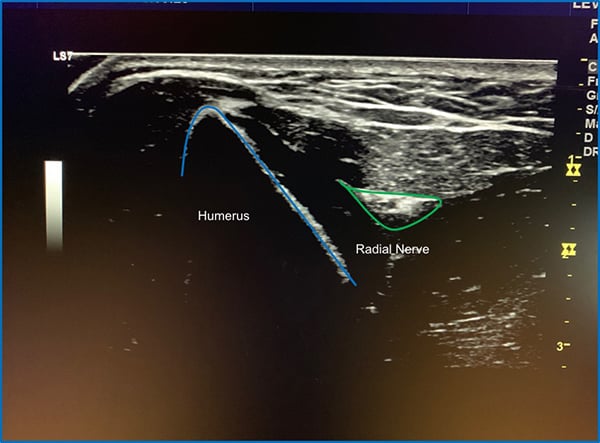
Patients should be placed in a supine position to help prevent any complications associated with anesthetic introduction such as vasovagal syncope. The forearm should be flexed at 90 degrees at the elbow with the wrist held in pronation. The linear US probe can then be applied about 2-4 cm superior to the lateral epicondyle of the elbow to facilitate appropriate identification of the radial nerve, surrounding vasculature/musculature and bony landmarks (Figure 1).

Step Two: Landmark Identification:
This positioning allows for rapid identification of the radial nerve which can be visualized as a hyperechoic triangular structure lying between the hypoechoic structures of the brachioradialis and brachial muscles, and adjacent to the humerus (Figure 2).
Step Three: Needle Advancement and Anesthetic Administration
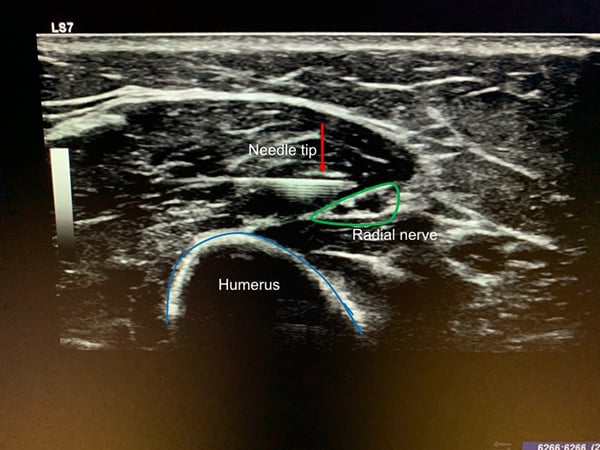
The skin is prepped in a sterile fashion with chlorhexidine or betadine. A sterile US probe cover should be applied and sterile US gel should be used to help limit the risk of introducing infection. With the radial nerve kept in view under ultrasound guidance, an in-plane approach should be used to visualize the needle thought its entire course as it approaches the nerve. After anesthetizing the tract using lidocaine and a 27 gauge needle, a larger gauge needle (20-22G) is used for the procedure as it tends to be visualized better under ultrasound. The anesthetic is introduced in a circumferential pattern around the nerve; this is done by injecting above and below the nerve, which will dissect it from the surrounding tissue and allow anesthetic to surround the nerve. A total of 5-7 mL of anesthetic is infiltrated. Initially 1-2 mL of anesthetic can be introduced to ensure appropriate positioning with the remaining amount administered upon verification (Figure 3).
Median Nerve Block
Step One: Positioning
The patient is placed in a position where the supinated forearm can be accessed by the provider. This can be in a sitting position or a supine position. The provider should create a clear line of sight from the patient’s forearm to the ultrasound screen (Figure 4).

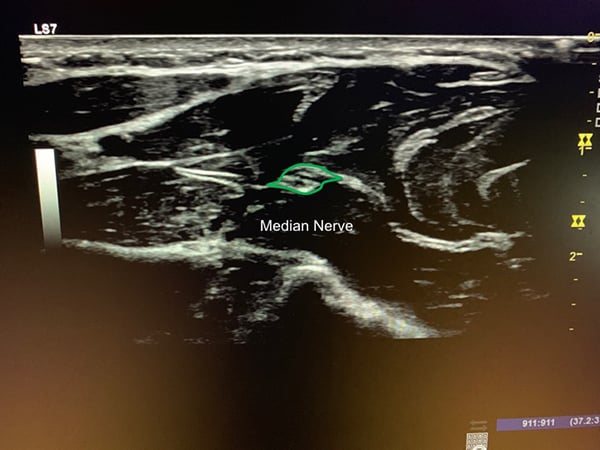
Step Two: Landmark Identification
The median nerve traverses the mid-volar forearm. The ultrasound probe is placed so that a cross-sectional view of the forearm is obtained from the volar surface. The provider should locate the nerve around the mid forearm (if you look closer to the wrist the nerve is hard to differentiate from the surrounding wrist flexor tendons). The nerve appears as a cluster of hypoechoic structures that are wrapped by hyperechoic tissue: this has been described as a cluster of grapes, or a honeycomb. You should also identify the ulnar and radial arteries on the periphery of the screen as these will need to be avoided during the procedure (Figure 5).
Step Three: Needle Advancement and Anesthetic Administration
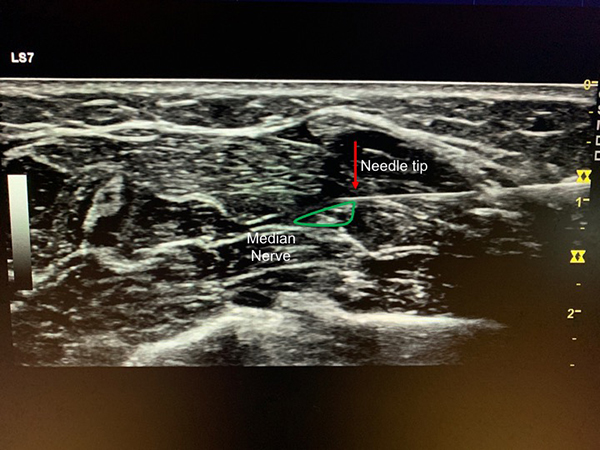
Again, the skin is prepped in a sterile fashion, a sterile US probe cover is applied, and sterile US gel is used. With the ultrasound probe in cross-section and the median nerve centered in the screen, note the depth of nerve from the skin surface. Then at either the radial or ulnar side of the forearm insert the needle into the skin directly below the edge of the US probe at a depth that matches the nerve depth. This will also be an in-plane approach with a goal to visualize the needle thought its entire course and the needle will run parallel to the US probe.
As above, the tract is anesthetized using lidocaine and a 27 gauge needle and if better visualization of the needle is required a larger gauge needle (20-22G) is used for the procedure. The anesthetic is introduced in a circumferential pattern around the nerve; this is done by injecting above and below the nerve, which will dissect it from the surrounding tissue and allow anesthetic to surround the nerve. A total of 5-7 mL of anesthetic is infiltrated. Initially 1-2 mL of anesthetic can be introduced to ensure appropriate positioning with the remaining amount administered upon verification (Figure 6).
The anesthetic of choice is provider dependent, but generally ranges from a short acting agent such as lidocaine, to a medium-acting agent such as bupivacaine or ropivicaine, to a mix of the two. Studies looking specifically at nerve blocks (orthopedic and anesthesia literature) show that lidocaine has a significantly faster onset of action compared to that of bupivacaine or ropivicaine, but a shorter duration of action7,8; while studies looking at skin anesthesia (plastic surgery and emergency medicine literature) point toward equivalence between the action of the agents, with onset of both within 30 seconds and effects lasting over 6 hours.9,10 Mixing the two has been shown to combine the benefits of the individual anesthetics. The literature supports success with multiple different medication choices.11 It is important to consider time to reduction, need for repeat neurovascular exams, and pain control upon discharge in these patients; anesthetic choice is based on balancing these considerations.
Complications
Given the limited adoption of US guided supracondylar nerve blocks, the associated risks or their rates of occurrence have not been widely studied, although they are important to consider prior to shifts in practice. In theory, these risks would be similar to other regional nerve blocks including neurovascular damage, bleeding, and infection. The use of US guidance and sterile technique can limit these risks, however more studies would be needed to show safety in practice.
It is important to realize that the supracondylar nerve block is a motor and sensory block. This will limit the ability to perform a neurovascular exam after the reduction. Because of this, the use of a short acting anesthetic (lidocaine) may be beneficial to facilitate the early recognition of any complications.
It is also important to consider anesthetic choice and the potential of rebound pain upon patient discharge which may lead to repeat visits or poor pain control upon discharge. There is limited evidence on rates of rebound pain in patients treated with regional anesthesia in an operative setting, but it is theorized that up to 40% of patients may experience this effect.12 It is reasonable to assume that this would translate to the ED setting. This is an important consideration, especially when providing return precautions and discharge pain control.
Anesthesia during splinting may also lead to tighter splint placement and limit diagnosis of compartment syndrome, however, the safety of forearm splint placement under IVRA has been shown in previous studies.13
Emergency Medicine is an ever-evolving field and it is important that we evolve with it. The addition of US guided procedures has increased the safety and efficacy of many different procedures from vascular access to arthrocentesis and should be considered in the utility of regional anesthesia. While more data is needed, there is promising evidence to suggest that distal radius fractures can be manipulated and splinted in a pain-free setting with fewer associated complications, shorter ED LOS, and with improved patient satisfaction with the use of ultrasound guided supracondylar radial nerve blocks.
References
- Smits GJ, Kuypers MI, Mignot LA, et al. Procedural sedation in the emergency department by Dutch emergency physicians: a prospective multicentre observational study of 1711 adults. Emerg Med J. 2017;34(4):237-242.
- Ünlüer EE, Karagöz A, Ünlüer S, et al. Ultrasound-guided supracondylar radial nerve block for Colles Fractures in the ED. Am J Emerg Med. 2016;34(8):1718–1720.
- Aydin AA, Bilge S, Kaya M, Aydin G, Cinar O. Novel technique in ED: supracondylar ultrasound-guided nerve block for reduction of distal radius fractures. Am J Emerg Med. 2016;34(5):912-913.
- Blaivas M, Adhikari S, Lander L. A Prospective Comparison of Procedural Sedation and Ultrasound-guided Interscalene Nerve Block for Shoulder Reduction in the Emergency Department. Acad Emerg Med. 2011;18(9), 922–927.
- Van de Pol GJ, Koudstaal MJ, Schuurman AH, Bleys RLAW. Innervation of the Wrist Joint and Surgical Perspectives of Denervation. J Hand Surg. 2006;31(1):28-34.
- Frenkel O, Herring AA, Fischer J, Carnell J, Nagdev A. Supracondylar Radial Nerve Block for Treatment of Distal Radius Fractures in the Emergency Department. J Emerg Med. 2011;41(4):386-388.
- Cuvillon P, Nouvellon E, Ripart J, et al. A comparison of the pharmacodynamics and pharmacokinetics of bupivacaine, ropivacaine (with epinephrine) and their equal volume mixtures with lidocaine used for femoral and sciatic nerve blocks: a double-blind randomized study. Anesth Analg. 2009;108(2):641-649.
- Vinycomb TI, Sahhar LJ. Comparison of local anesthetics for digital nerve blocks: a systematic review. J Hand Surg Am. 2014;39(4):744-751.e5.
- Collins JB, Song J, Mahabir RC. Onset and duration of intradermal mixtures of bupivacaine and lidocaine with epinephrine. Can J Plast Surg. 2013;21(1):51-53.
- Alhelail M, Alsalamah M, Al-Mulhim M, Al-Hamid S. Comparison of bupivacaine and lidocaine with epinephrine for digital nerve blocks. Emerg Med J. 2009 May;26(5):347-350.
- Martin R, Dumais R, Cinq-Mars S, Tétrault JP. [Axillary plexus block by simultaneous blockade of several nerves. II. Evaluation of lidocaine-bupivacaine combination]. Ann Fr Anesth Reanim. 1993;12(3):233-236.
- Lavand’homme, P. Rebound pain after regional anesthesia in the ambulatory patient. Curr Opin Anaesthesiol. 2018;31(6):679-684.
- Aarons CE, Fernandez MD, Willsey M, et al. Bier Block Regional Anesthesia and Casting for Forearm Fractures. J Ped Orthop, 2014;34(1):45-49.
Other resources:
- Bear DM, Friel NA, Lupo CL, Pitetti R, Ward WT. Hematoma Block Versus Sedation for the Reduction of Distal Radius Fractures in Children. J Hand Surg Am. 2015;40(1):57-61.
- Godwin SA, Burton JH, Gerardo CJ, et al. Clinical Policy: Procedural Sedation and Analgesia in the Emergency Department. Ann Emerg Med. 2014;63(2):247-258.e18.
- Kendall JM, Allen P, Younge P, Meek SM, McCabe SE. Haematoma block or Bier’s block for Colles’ fracture reduction in the accident and emergency department—which is best? J Accid Emerg Med. 1997;14(6):352–356.
- Stone MB, Wang R, Price DD. Ultrasound-guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med. 2008;26(6):706-710.


