EMS arrived with a 38-year-old male who was found down by his roommate.
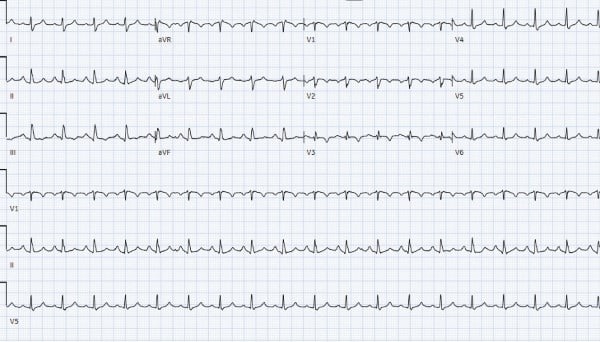
The patient was unresponsive with an irregular respiratory rate of 20. He was in a wide-complex tachycardia with a Glasgow Coma Score of 3. Narcan was given with no effect. The patient was intubated on scene with rocuronium and etomidate before ketamine was administered for sedation. There was a rhythm change en route to the hospital. EMS 12-lead showed a regular, wide-complex tachycardia with RsR’ ST-elevation in aVR and diffuse t wave changes. There was rightward axis deviation, and the QRS was widened to 138 milliseconds (ms).
EKG Findings: A Red Herring?
QRS prolongation and a terminal R’ should raise concern for tricyclic antidepressant (TCA) overdose, a diagnosis that often must be made on EKG alone due to a quick clinical progression and a high mortality rate. In cases of TCA overdose, a QRS greater than 100 ms is predictive of seizures, and as many as 50% of patients with a QRS over 160 ms will experience ventricular arrhythmias.1
TCAs exert their therapeutic effect by inhibiting the reuptake of norepinephrine and serotonin. At toxic doses TCAs also block sodium channels, impeding sodium entry into myocardial cells. Slower sodium entry delays membrane depolarization, therefore decelerating ventricular contraction and prolonging the QRS. The right–sided intraventricular conduction system is more susceptible to sodium channel blockade than the left bundle. The R’ seen in TCA overdose is most prominent in aVR because the right ventricle contracts more slowly than the left ventricle.1,2
In addition to arrhythmias caused by sodium channel blockade, TCA overdose causes hypotension through several other mechanisms. Anticholinergic effects from TCA muscarinic blockade cause tachycardia and decreased filling time. Alpha adrenergic receptors are blocked by TCAs in the periphery, causing vasodilation. Heart block (most notably right-sided conduction delays including bundle branch block) and bradycardia are late-stage manifestations, further exacerbating hypotension.3
Decompensation and Critical Interventions
Within 5 minutes of arrival, the patient lost pulses. CPR and standard resuscitation therapy were initiated. Bicarbonate, magnesium, and calcium administration were also prioritized, and return of spontaneous circulation (ROSC) was achieved after four rounds of compressions. Intermittent QRS prolongation responded well to boluses of bicarbonate throughout the next few hours.
First-line treatment of TCA overdose consists of bicarbonate and hyperventilation, both of which alkalize the blood. TCAs are weakly basic, and their ionized effective state is most stable in acidic environments. At a higher pH, TCAs become protein bound, thereby decreasing their chemical activity. In overdose, alkalization therefore minimizes TCA toxicity. Monitoring with serial EKGs is necessary as QRS prolongation can recur up to 72 hours after an initially adequate response to treatment.4
The EKG findings of TCA toxicity should prompt the clinician to also consider other etiologies. Right bundle branch block, T wave inversions in V2–V3, and ST elevation in aVR are all associated with increased risk of circulatory shock and death in cases of pulmonary embolism (PE).5
Unexpected Causes Found
Prior to ICU transfer, the patient was sent for CT pulmonary angiography, which showed bilateral pulmonary emboli involving the right distal main pulmonary artery. Reflux of contrast into the IVC raised concern for right heart strain. Serial serum TCA testing was negative. Urine toxicology resulted positive for cocaine and benzodiazepines.
Apart from PE and TCA overdose, additional hypotheses for the case’s EKG findings are reviewed below.
Cocaine toxicity can cause sodium channel blockade, an ‘S’ wave in leads I and aVL, and an ‘R’ wave in lead aVR. It can be accompanied by an incomplete RBBB pattern in the precordial leads.6 Trazodone, which the patient was prescribed, is also known to cause wide-complex tachycardia and heart block in the setting of overdose.7 Lastly, hyperkalemia should be considered in any case involving prolonged QRS or unexplained EKG findings.8
Repeat potassium on arrival to the MICU (around 4 hours after ROSC) showed an increase to >7. An EKG was taken around this time, prior to treatment. Serial EKGs showed no changes corresponding with this subsequently elevated potassium. (Figures 1 and 2)
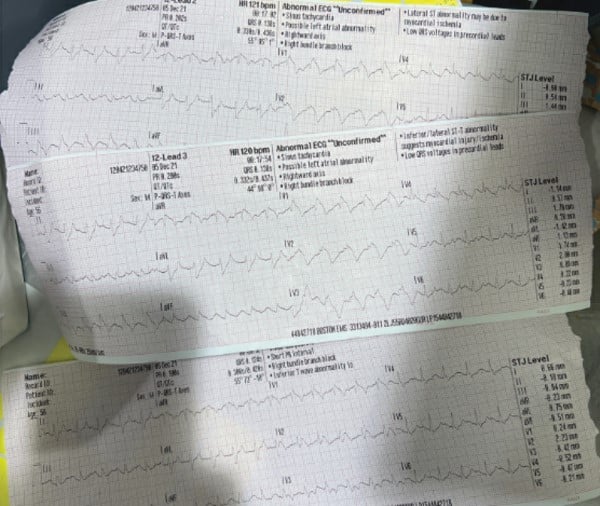
Figure 1 (above) and Figure 2 (below)
Take-Home Points
• At toxic doses, TCAs cause blockade of sodium channels, muscarinic receptors, and alpha-adrenergic receptors. Slowed ventricular contraction, tachycardia, and vasodilation cause hypotension in these cases.
• QRS prolongation and a terminal R’ should raise concern for TCA overdose, but may be found in other acute pathologies as well. Consider empiric administration of bicarbonate based on EKG alone.
• Both TCA overdose and PE specifically strain the right ventricle. ST elevation in aVR, often seen in PE, can mimic the classic R’ seen in aVR during TCA overdose.
References
- Boehnert MT, Lovejoy FH. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985;313(8):474-9.
- Yates C, Manini AF. Utility of the electrocardiogram in drug overdose and poisoning: theoretical considerations and clinical implications. Curr Cardiol Rev. 2012;8(2):137-51.
- Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emergency Medicine Journal. 2001;18(4):236-241.
- Brown TC, Barker GA, Dunlop ME, Loughnan PM. The use of sodium bicarbonate in the treatment of tricyclic antidepressant-induced arrhythmias. Anaesthesia and Intensive Care. 1973;1(3):203-210.
- Shopp JD, Stewart LK, Emmett TW, Kline JA. Findings From 12-lead Electrocardiography That Predict Circulatory Shock From Pulmonary Embolism: Systematic Review and Meta-analysis. Acad Emerg Med. 2015;22(10):1127-37.
- Hoffman RS. Treatment of patients with cocaine-induced arrhythmias: bringing the bench to the bedside. Br J Clin Pharmacol. 2010;69(5):448-57.
- Soe KK, Lee MY. Arrhythmias in Severe Trazodone Overdose. Am J Case Rep. 2019;20:1949-55.
- Dittrich KL, Walls RM. Hyperkalemia: ECG manifestations and clinical considerations. J Emerg Med. 1986;4(6):449-455.



