Patients with suspected ocular trauma are at risk of vision loss - and emergency physicians must recognize the danger.
This is one situation where an emergent ophthalmology consult is critical, as you work to measure and control intraocular pressure.
Case Presentation
A 67-year-old male with a past medical history of medication-controlled hypertension presented to the emergency department following a right eye injury sustained while working out. The patient was using an exercise band during a home workout when the band snapped, recoiled, and struck him in the right eye. He arrived with severe right eye pain and near-total visual impairment with shadow distinction. He otherwise denied photophobia, pain with extraocular movement, or headache. He never wore contacts or corrective lenses and had no prior ocular history. On physical examination, several minor superficial abrasions were noted on the right eyelid, and his right eye was erythematous. His right pupil was 5mm and non-reactive. His left eye was within normal limits, EOM intact and without pain. No proptosis was identified.
An exam under fluorescein stain identified several minor corneal abrasions with a negative Seidel sign. On tonometry, the right eye's intraocular pressure (IOP) was 56 mmHg, and the left eye's IOP was 10 mmHg. A diagnosis of traumatic glaucoma was made.
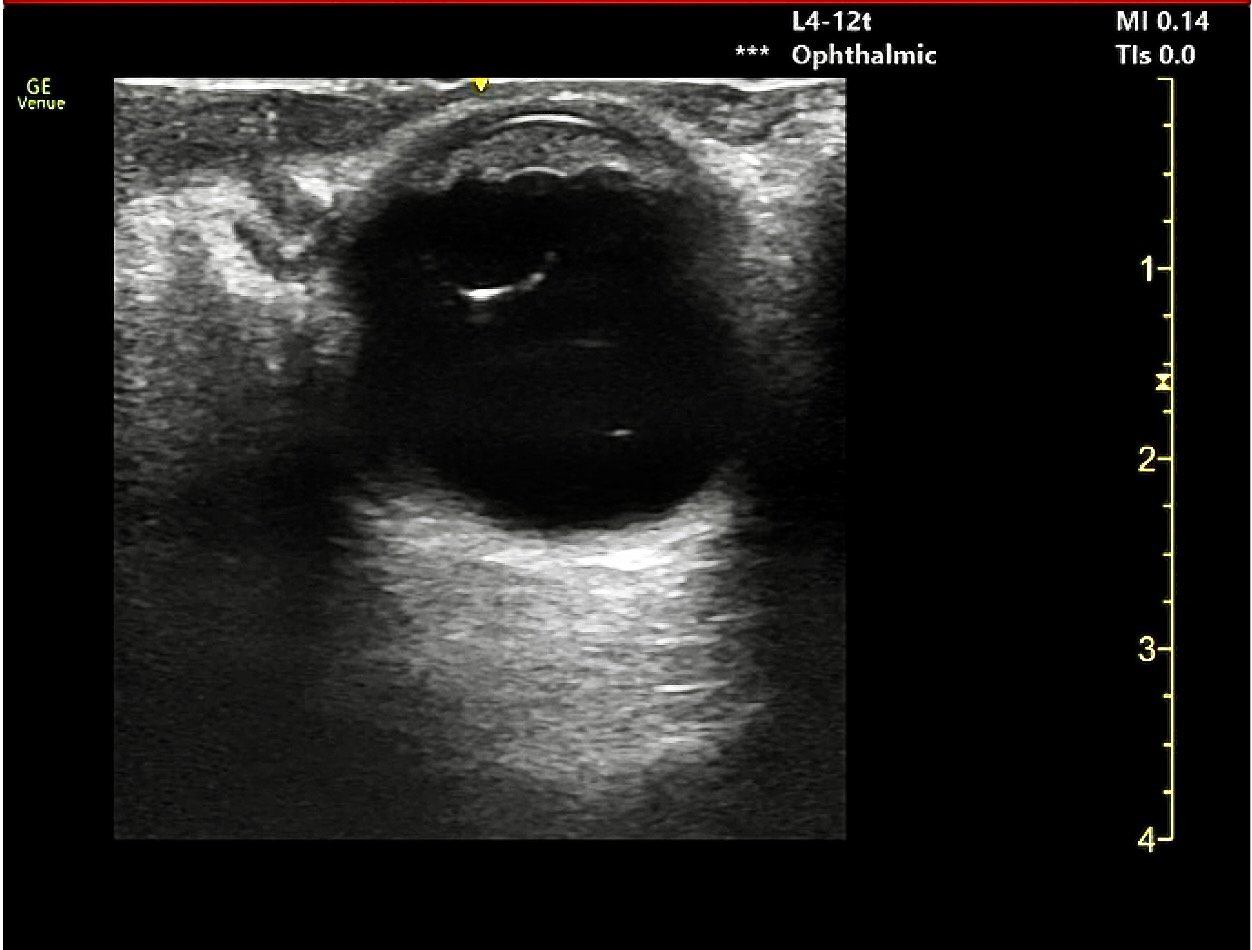

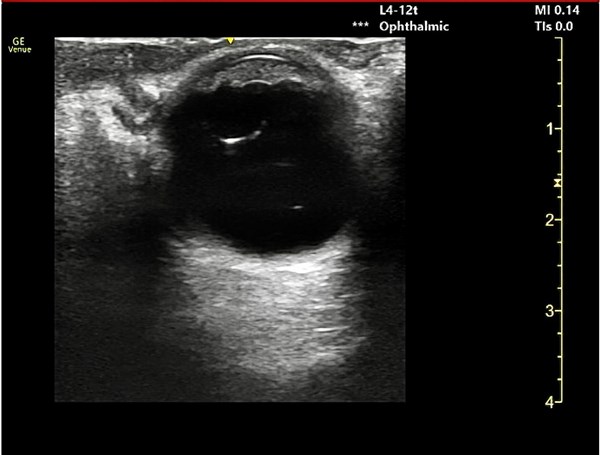
Images 1 and 2. Ultrasound images of the affected eye noting a posteriorly subluxed lens with mild vitreous hemorrhage
Case Discussion
Traumatic glaucoma is a form of secondary glaucoma that can develop following trauma to the eye and orbit. More common after blunt trauma, it can nevertheless occur following penetrating injury. Traumatic glaucoma may also develop after chemical, thermal, electrical, or radiation injuries.
Often, traumatic glaucoma develops immediately following trauma to the eye, although on occasion, it may present days to weeks following the initial injury. The disease progresses when increased aqueous humor collection within the eye leads to increased IOP and damage to the optic nerve. Increased IOP may develop after ocular trauma through several mechanisms: disruption of the trabecular meshwork after globe trauma, bleeding into the anterior chamber (hyphema), or traumatic, inflammatory changes to the iris leading to compromise of the blood-aqueous barrier.
A complicating factor in this case was the apparent posterior lens subluxation noted on ultrasound (Figure 1). Posterior displacement of the lens can lead to rupturing of the zonular fibers which hold the lens in place. Subluxation typically occurs when 25% or more of the zonules are torn. Full lens dislocation (ectopia lentis) may occur with complete disruption of the zonules. It is thought that the posteriorly dislocated lens may have promoted intermittent angle closure or that the vitreous prolapse (vitreous leak into the anterior chamber and pupil) may have disrupted the trabecular meshwork, disrupting clearance of aqueous humor. Subluxed or dislocated lenses may also cause local trauma and irritation to the nearby iris, leading to the release of pigments into the vitreous, which may also work to disrupt proper aqueous absorption.
Once the diagnosis was made, treatment was promptly initiated (see below), and ophthalmology was consulted.
Vision-Saving Treatment in the ED
In the emergency setting, treatment of traumatic glaucoma must focus on reducing IOP while establishing a plan for definitive care. Medical treatment aims to accomplish this by increasing aqueous humor outflow and reducing aqueous humor production. The patient was administered IV acetazolamide to reduce aqueous humor production. Dorzolamide/Timolol (combined topical carbonic anhydrase inhibitor and beta-blocker) and Brimonidine 0.15% (alpha agonist) eye drops were administered every fifteen minutes, along with serial tonometry measurements. Despite these measures, the IOP remained elevated in the affected eye, and this same regimen was continued for another hour. It is postulated that the IOP remained elevated despite medical therapy because the posteriorly dislocated lens may have been intermittently and transiently obstructing the resorption of aqueous humor.
Following the second hour of medical therapy, intraocular pressures improved but remained elevated at 30-40 mmHg. At this time, a decision was made to transfer the patient to a center with additional ophthalmological capabilities for further management. While awaiting transfer, the patient was provided additional medical therapies, including prednisolone and Cyclopentolate eye drops, and was administered a one-time dose of IV mannitol over 45 minutes with a continued goal of normalizing intraocular pressure at the recommendation of our ophthalmology consultants.
On outside hospital arrival, right intraocular pressure was measured at 21 mmHg. He was observed for several hours with serial pressure checks and ultimately discharged home with a plan for IOP re-check in 24 hours and non-emergent outpatient surgical management.
He was instructed to continue prednisone, brimonidine, acetazolamide, and dorzolamide/timolol, to sleep with head of bed elevated, and to avoid NSAIDs and any straining or heavy lifting.
Take-Home Points
- Measuring intraocular pressure in patients with suspected ocular trauma is essential. However, it is critical to exclude globe rupture first, as measuring intraocular pressure in this case can be harmful. Elevated intraocular pressure (usually greater than 30mmHg although diagnosis can be made with >21 mmHg), along with eye pain and a minimally reactive pupil, is concerning for acute traumatic glaucoma.
- This is one situation where an emergent ophthalmology consult is critical. The goal for ED physicians is to reduce IOP until ophthalmology decides on a definitive care plan. Early and effective therapy is crucial in optimizing ocular nerve perfusion and limiting potential permanent vision loss. Medical intervention aims to increase aqueous humor outflow while reducing production.
- Ocular ultrasound is a valuable tool in identifying additional contributory pathologies such as lens subluxation/dislocation or detachment, vitreous hemorrhage or detachment, or retinal detachment.
References
- Emanuel ME, Parrish RK II, Gedde SJ. Evidence-based management of primary angle closure glaucoma. Curr Opin Ophthalmol. 2014;25(2):89–92.
- Khouri A, Murchison A, Justin G, Woreta F, Owaidhah O. Traumatic glaucoma. EyeWiki. Accessed April 30, 2024.
- Ng JK, Lau O. Traumatic Glaucoma. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
- Weizer J. Angle-Closure Glaucoma. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on April 30 2024.)