The most common cause of torsades de pointes is acquired prolongation in the QT interval because of medication. Treating it may require pharmacologic pacing or, in some circumstances, mechanical pacing.
Case Report
A 59-year-old female presents to the ED complaining of dizziness and unsteady gait that started a day ago. She was found lethargic and confused by her family. Further information was unavailable because of the patient's altered mental status. Past medical history includes diabetes and hypertension; medications are insulin, amlodipine, and gabapentin. Vital signs are HR 48 bpm, blood pressure 224/100 mmHg, respiratory rate 18, temperature 36.8 C, and oxygen saturation 98% on room air.
On physical examination, patient is lethargic and disoriented. There is loss of nasolabial fold on the right side with decreased motor strength 4/5 in the right upper and lower extremity. Patient also has slurred speech.
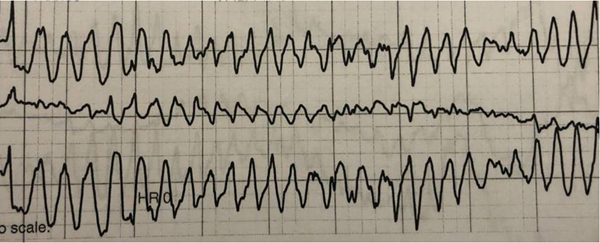
Initial EKG showed sinus bradycardia with heart rate 48 bpm, Qtc 498 ms, no acute STE, STD, TWI noted. (Figure 1).
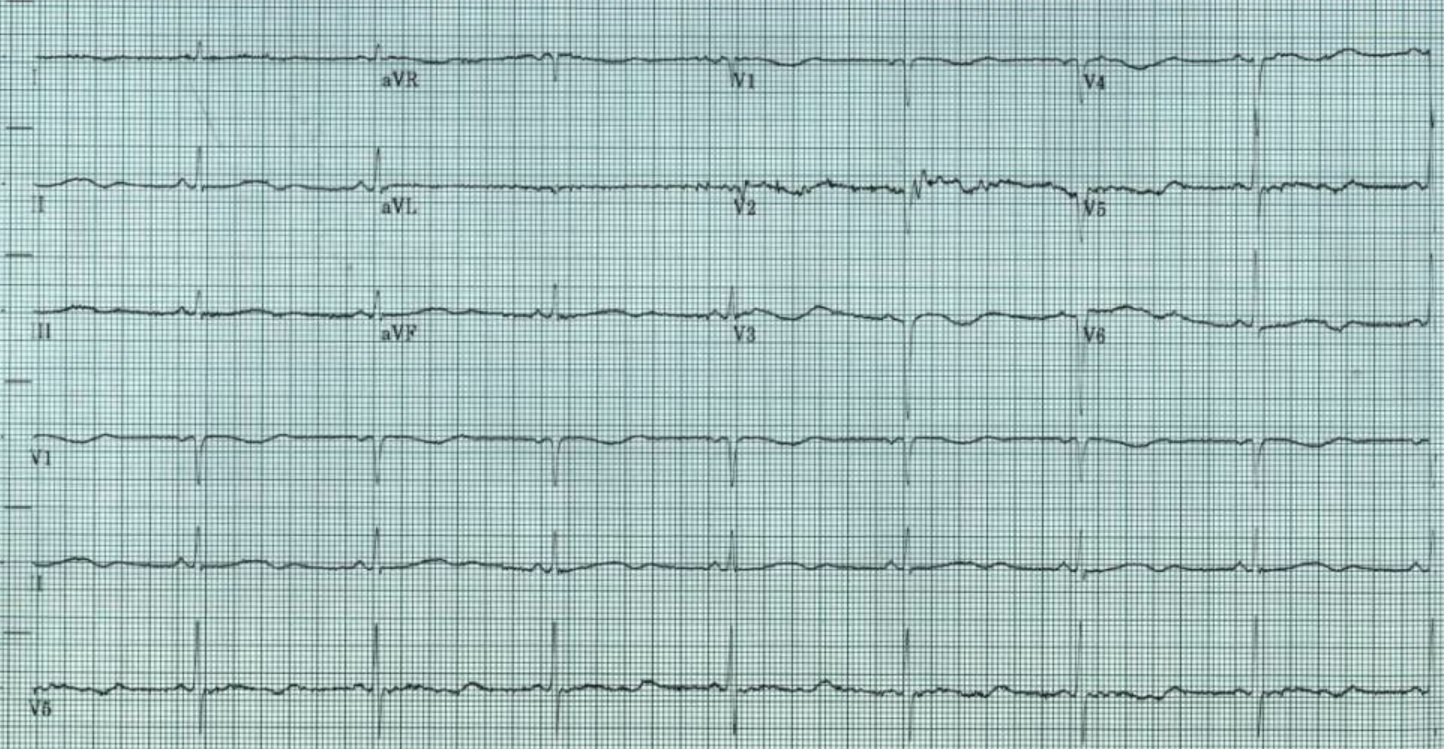
Figure 1. Initial EKG
One dose of 20 mg of labetalol via IV was given, for suspected hypertensive crisis with intracranial pathology (ischemic vs. hemorrhagic stroke). Workup included CBC, CMP, EKG, chest XR, CT and CTA head and neck, coagulation panel, ammonia, thyroid profile, urine drug screen, urinalysis, and alcohol level. While in the ED, patient experienced an episode of torsades de pointes, with loss of consciousness, that lasted for 20-30 seconds (Figure 2).
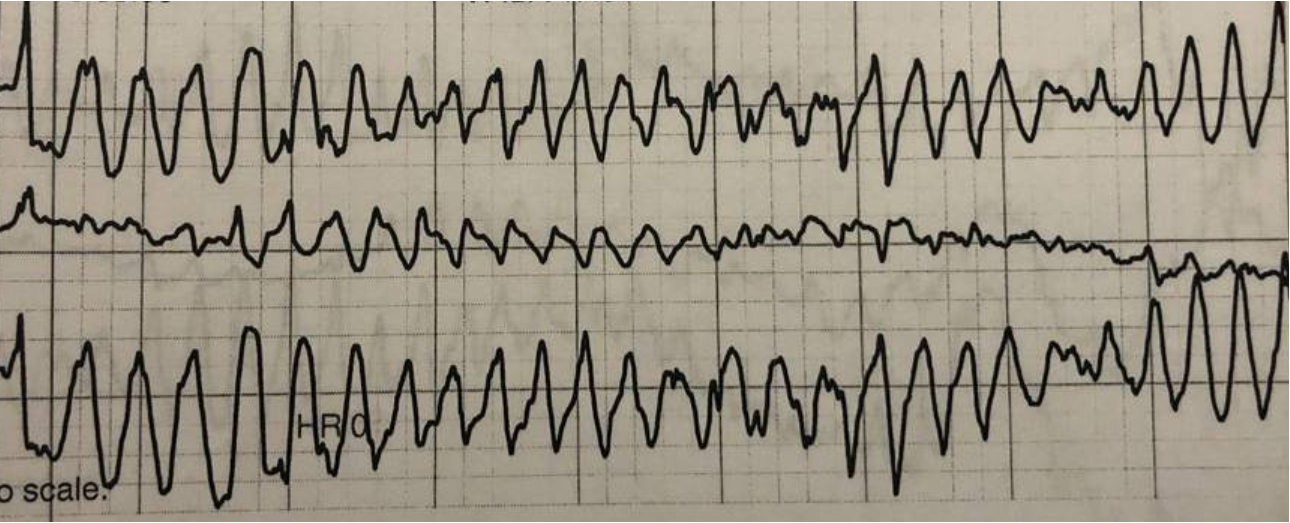
Figure 2. Torsades de pointes
Repeat EKG showed heart rate 65 bpm, with prolonged QTC of 628 ms with ventricular bigeminy (Figure 3).
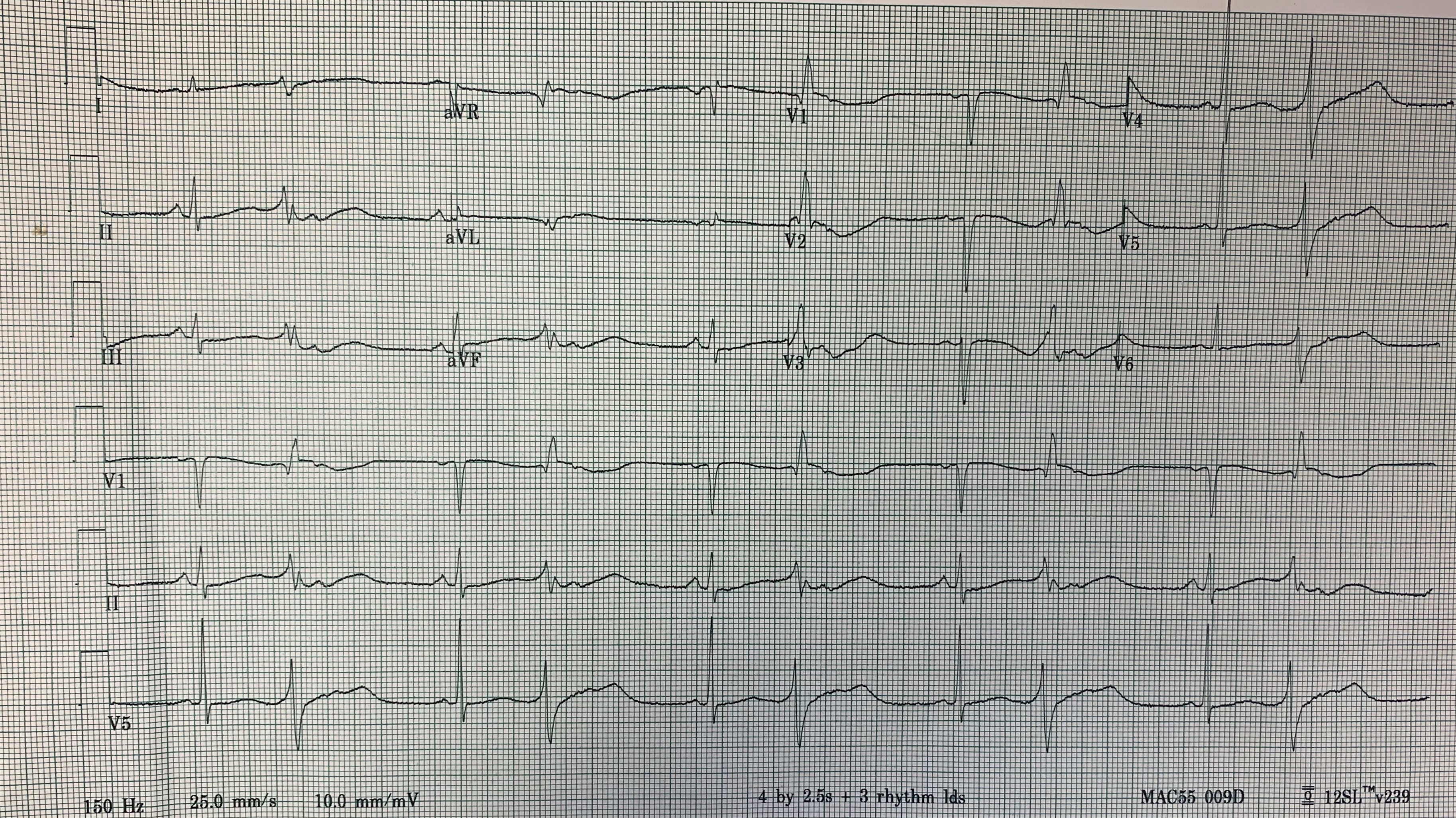
Figure 3. Repeat EKG
Metabolic panel revealed electrolyte abnormalities: hypokalemia with a potassium of 2.6 mmol/L, hypomagnesemia with magnesium of 1.4 mg/dL, and hyperglycemia with glucose of 486 mg/dL. Urine drug screen was positive for methadone, and urinalysis was positive for leukocyte esterase with white blood cells > 50/hpf.
Patient was given 40 mq potassium and 2 g magnesium bolus IV. She had another short episode of Tdp with loss of consciousness. Another 4 g of magnesium was given.
Isoproterenol was unavailable, so transcutaneous overdrive pacing was attempted. Mechanical and electrical capture was obtained with heart rate 110 bpm at 80 mA. CTA head and neck showed complete occlusion of the left middle cerebral artery at the M1 branch with an Acute to subacute infarct in the left frontal, caudate, and basal ganglia (Figure 4).
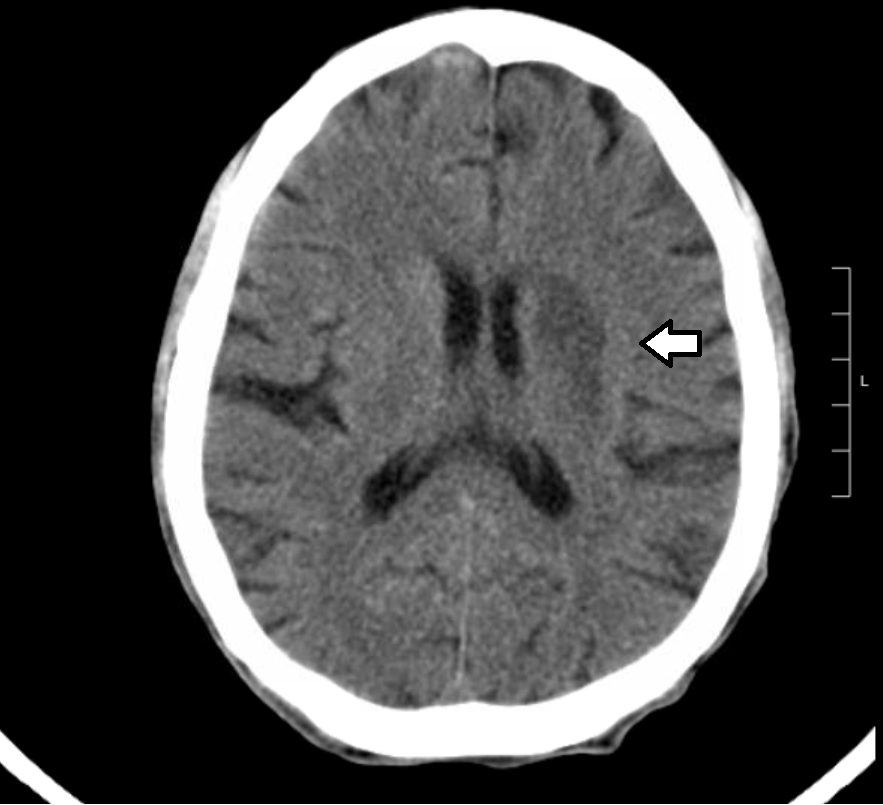
Figure 4. Imaging of the head and neck
Findings were consistent with MCA distribution infarct. The patient was transferred to a tertiary hospital for further treatment and admission to cardiac intensive unit.
Discussion
Torsades de pointes is a type of polymorphic ventricular tachyarrhythmia in which the QRS complexes appear to twist around the isoelectric line. It is universally associated with congenital or acquired long QTc syndrome (LQTS).1 Congenital LQTS has been found to be associated with 1 of 6 identified mutations in genes coding for cardiac ion channels (LQT 1–6).2
The most common cause of torsades de pointes is acquired prolongation in the QT interval because of medication. Acquired QT prolongation has been the single most common cause of withdrawal or restriction of drugs' use after they have been marketed in the past decade.3
Multiple risk factors are implicated in prolonged QT interval progressing to torsades de pointes:4-7
- Hypokalemia
- Female sex
- Hypomagnesemia
- Digitalis therapy
The prolongation of the QT interval to longer than 500 ms during drug therapy should prompt a critical re-evaluation of that therapy and consideration of therapeutic alternatives. Many drugs are known to cause QTc prolongation, including chlorpromazine, metoclopramide, atypical antipsychotics, thioridazine, TCAs, macrolide antibiotics, methadone, lithium, and antiarrhythmic drugs (class IA, IC, and III).
Magnesium sulphate suppresses torsades de pointes by decreasing the influx of calcium ions, which in turn results in decreased amplitude of early afterdepolarizations.8 The initial dose is 2 g (20 mL of 10% solution), given IV over 1-2 minutes. This can be repeated up to a total of 6 g, with 5-15 minutes between doses. Following a bolus of 2-4 g of magnesium, very little magnesium is absorbed into cardiac tissue. Most is excreted in the urine, and unless the patient has severe renal failure, magnesium levels will drop back to baseline over next several hours.9 Hence, it's preferred to follow the bolus with a magnesium infusion at a rate of 1-2 g/hr.
In some circumstances, pharmacologic pacing (using isoproterenol) or transvenous pacing may be necessary to suppress arrhythmias by increasing the baseline heart rate to 100-150 bpm.10-11 Temporary transcutaneous pacing has also been successfully used to convert torsades de pointes.12 IV lidocaine, a Class IB antiarrhythmic that shortens QT interval, can also be used. An acute episode prolonged enough to cause hemodynamic compromise is treated with unsynchronized cardioversion, beginning with 100 joules.
As in our case, it is important to remember that isoproterenol may not always be available, and mechanical pacing may be necessary. Targeting higher magnesium serum levels with magnesium infusion and IV lidocaine can be life-saving.
References
1. Viskin S. Long QT syndromes and torsades de pointes. The Lancet. 1999;354(9190):1625-1633.
2. El-Sherif N, Turitto G, Boutjdir M. Congenital Long QT syndrome and torsades de pointes. Ann Noninvasive Electrocardiol. 2017;22(6):e12481.
3. Roden DM. Drug-Induced Prolongation of the QT Interval. Wood AJJ, ed. N Engl J Med. 2004;350(10):1013-1022. doi:10.1056/NEJMra032426.
4. Makkar RR, Fromm BS, Steinman RT, Meissner MD, Lehmann MH. Female Gender as a Risk Factor for Torsades de Pointes Associated With Cardiovascular Drugs. JAMA. 1993;270(21):2590-2597.
5. Torp-Pedersen C, Møller M, Bloch-Thomsen PE, et al. Dofetilide in Patients with Congestive Heart Failure and Left Ventricular Dysfunction. N Engl J Med. 2008;341(12):857-865.
6. Houltz B, Darpo B, Edvardsonn N, et al. Electrocardiographic and Clinical Predictors of Torsades de Pointes Induced by Almokalant Infusion in Patients with Chronic Atrial Fibrillation or Flutter: A Prospective Study. Pacing Clin Electrophysiol. 1998;21(5):1044-1057.
7. Yang T, Roden DM. Extracellular Potassium Modulation of Drug Block of IKr. Circulation. 1996;93(3):407-411.
8. Tzivoni D, Banai S, Schuger C, et al. Treatment of torsades de pointes with magnesium sulfate. Circulation. 1988;77(2):392-397.
9. Biesenbach P, Mårtensson J, Lucchetta L, et al. Pharmacokinetics of Magnesium Bolus Therapy in Cardiothoracic Surgery. J Cardiothoracic Vasc Anesthesia. 2018;32(3):1289-1294.
10. El-Sherif N, Turitto G, Boutjdir M. Acquired long QT syndrome and torsades de pointes. Pacing Clin Electrophysiol. 2018;41(4):414-421.
11. Roden DM. A practical approach to torsades de pointes. Clin Cardiol. 1997;20(3):285-290.
12. Charlton NP, Lawrence DT, Brady WJ, Kirk MA, Holstege CP. Termination of drug-induced torsadess de pointes with overdrive pacing. Am J Emerg Med. 2010;28(1):95-102.