A 72-year-old male with past medical history of cirrhosis and emphysema presented to the ED for facial swelling.
Two days prior, the patient had a witnessed mechanical fall from standing without loss of consciousness or head injury. Patient endorsed worsening right arm swelling, followed by facial swelling, left arm swelling, and finally scrotal swelling. At triage, the patient's chief complaint was listed as “angioedema.” The patient’s wife provided a photo of the patient from 1 week prior that showed a thin male without facial or periorbital edema (Picture 1).

On presentation, his vital signs were BP 142/88, HR 143, RR 20, SpO2 93% on room air and temperature 36.9C. On physical examination, the patient had a midline epiglottis with no intraoral swelling, decreased air movement bilaterally, distant cardiac sounds, and diffuse, soft, nontender edema of the eyelids, face, neck, chest wall, abdomen, and scrotum. Crepitus was palpated over his shoulders, hands, and thighs.
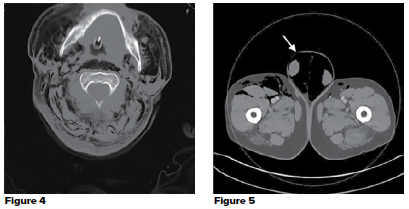
POCUS of the anterior chest wall was performed to evaluate for lung sliding. Normal chest wall landmarks were difficult to identify. Images were difficult to interpret due to the presence of multiple hyperechoic vertical lines with dirty shadowing reverberation artifact which obscured the anatomy (Picture 2). These findings were concerning for subcutaneous emphysema (SE). Similar POCUS findings were seen throughout the chest wall, abdomen, proximal extremities, and scrotum (Picture 3).
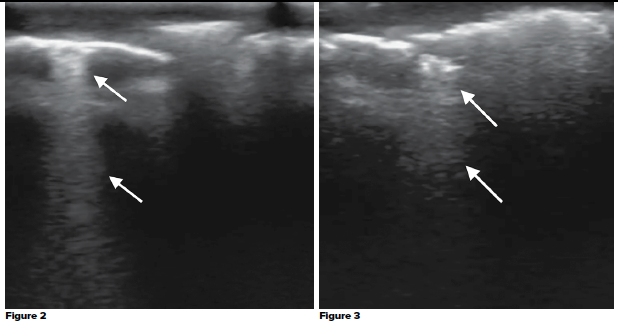
The patient began gurgling with respirations, prompting concern for airway compromise. A bedside fiberoptic nasal laryngoscopy demonstrated normal vocal cords without laryngeal swelling, but narrowed due to external compression. The patient was intubated for airway protection and transported to CT.
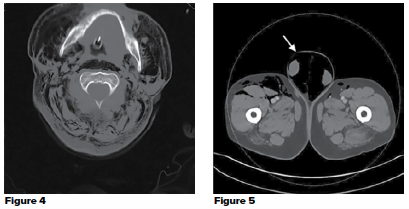
CT scan demonstrated extensive SE tracking from the chest wall up to the deep spaces of the face, right-sided pneumothorax with rib fractures, pneumomediastinum, pneumoperitoneum, and pneumoscrotum (Picture 4, 5).
Discussion
Subcutaneous emphysema is the presence of air within the subcutaneous layers of the skin caused by gas formation secondary to infection, or more commonly, air escaping from pleura, mediastinum, peritoneum, or gastrointestinal tract. Common causes include trauma, spontaneous pneumothorax, iatrogenicity, and barotrauma.2,3 In our case, the source was traumatic given the right-sided rib fracture. In the most severe form of SE (Grade V), there is involvement of the face, neck, torso, abdomen, and scrotum. While palpating for crepitus can help with the clinical diagnosis of SE, it often presents as generalized distention or bloating. In our case, the triage team labeled his symptoms as angioedema, which is similar to a previously published case report.1
SE can be seen on ultrasound as focal punctate hyperechoic regions with
dirty" posterior acoustic shadows and reverberation artifacts, called “E lines”. In POCUS evaluation, the movement of “E Lines” in SE can be mistaken for vertical B lines seen in sliding lungs.4 To avoid this mistake, it is critical to confirm that the vertical lines are originating from the pleural lines using rib shadows as reference, and to confirm the sliding motion correlates with breathing. In our case, there was no respiratory movement and no rib shadowing to indicate the level of the pleura.
SE itself is often benign, however, its discovery should be a red flag for significant injuries.3 In a prospective observation of 405 blunt traumatic patients, SE was only seen in 6% of cases, however, every case with SE also had a pneumothorax.5 SE can also cause severe airway compromise. A previous case report describes a case of a traumatic patient with SE and pneumothorax who initially presented with an intact airway. His airway acutely decompensated 7 hours after presentation and he was unable to be intubated due to visualized airway edema, ultimately requiring a surgical tracheostomy.6 Our prompt recognition of his SE and fiberoptic findings led to a change in management resulting in earlier intubation for airway protection.
The other unique POCUS finding in our patient was pneumoscrotum. Pneumoscrotum can be primarily caused by gas producing infections like Fournier’s gangrene, or a secondary cause resulting in gas tracking from the mediastinum, peritoneum, retroperitoneum, or abdominal fascia. Pneumoscrotum is a very rare condition with only 59 cases in the literature since 2013. The majority were caused by abdominal endoscopy and laparotomic surgery, with only 5 cases of pneumoscrotum secondary to blunt chest trauma.7
Like SE, pneumoscrotum itself is often benign but associated with significant injuries. In the six reported cases of pneumoscrotum secondary to blunt trauma, every case was also found to have a pneumothorax and half of the cases had pneumomediastinum.8-13 One case report describes a pneumothorax that was correctly identified and treated during a traumatic arrest based on the clinical presence of pneumoscrotum.8 Pneumoscrotum can be difficult to diagnose clinically as it may present without crepitus and simply as scrotal edema, similar to our case. While most reports of pneumoscrotum were diagnosed by CT scan, evidence of pneumoscrotum can be seen on POCUS. Pneumoscrotum on POCUS is seen as linear hyperechoic reflections with significant retro-acoustic shadowing in the scrotal area.
SE can be a difficult and misleading clinical diagnosis, however, POCUS can rapidly confirm the presence of SE. While SE may obscure POCUS evaluation of the thorax and abdomen, the presence of SE should alert the provider to significant traumatic injuries and possible airway compromise. In addition, POCUS can diagnose pneumoscrotum, another marker of significant trauma.
Case Conclusion
The patient received a right-sided thoracostomy tube with improvement of his vital signs. He was admitted to the medical ICU and received a blow-hole incision for significant SE. He was extubated on hospital day (HD) 3, had the thoracostomy tube removed on HD 5, and discharged on HD 7.
REFERENCES
- Dhawan AK, Singal A, Bisherwal K, et al. Subcutaneous emphysema mimicking angioedema. Indian Dermatol Online J. 2016;7(1):55-56.
- Kukuruza K, Aboeed A. Subcutaneous Emphysema. [Updated 2020 Mar 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan.
- Aghajanzadeh M, Dehnadi A, Ebrahimi H, et al. Classification and Management of Subcutaneous Emphysema: a 10-Year Experience. Indian J Surg. 2015;77(Suppl 2):673-677.
- Dewitz A. Chapter 18. Musculoskeletal, Soft Tissue, and Miscellaneous Applications. In: Ma O, Mateer JR, Reardon RF, Joing SA. eds. Ma and Mateer's Emergency Ultrasound, 3e. McGraw- Hill.
- Ball CG, Ranson K, Dente CJ, et al. Clinical predictors of occult pneumothoraces in severely injured blunt polytrauma patients: A prospective observational study. Injury. 2009;40(1):44-47.
- Olmstead D, Gelfand G, Anderson I, et al. (2018). A Case Report of Acute Airway Compromise due to Subcutaneous Emphysema. Case Reports in Medicine. 2018. 1-5. 10.1155/2018/3103061.
- Cochetti G, Barillaro F, Cottini E, et al. Pneumoscrotum: report of two different cases and review of the literature. Ther Clin Risk Manag. 2015;11:581-587.
- Humayun A, Chai LF, Pontell ME, et al. Pneumoscrotum: Value as an early diagnostic sign of tension pneumothorax in blunt thoracic trauma. Int J Crit Illn Inj Sci. 2018;8(4):210-213.
- Patel R, Singh A, Devgarha S, et al. Pneumoscrotum as complication of blunt thoracic trauma: A case report. IOSR J Dent Med Sci. 2014;13:5–7.
- Lostoridis E, Gkagkalidis K, Varsamis N, et al. Pneumoscrotum as complication of blunt thoracic trauma: A case report. Case Rep Surg 2013. 2013:392869.
- Su JT, Hsia JY, Hu SY, et al. Pneumoscrotum after blunt chest trauma. Urology. 2011;77:75–6.
- Simaioforidis V, Kontos S, Fokitis I, et al. Subcutaneous emphysema of the scrotum (pneumoscrotum) due to traumatic pneumothorax: A case report. Cases J. 2008;1:293.
- Wakabayashi Y, Bush WH, Pneumoscrotum after blunt chest trauma. J Emerg Med. 1994;12:603–5.