Malaria is a potentially life-threatening disease caused by the Plasmodium parasite. Symptoms usually present 1–4 weeks after infection but can present months to years later depending on the species. It's a diagnosis you don't want to miss.
Case
A 31-year-old female with a past medical history of polycystic ovarian syndrome and pre-diabetes presented to the ED for a positive malaria test taken by her PCP. The patient states she was in Ghana for 10 days last month to visit friends. She says she was offered malaria prophylaxis but declined. About 10 days after returning home she started developing symptoms of fever, night sweats, cough, nausea, and vomiting. She was seen at an urgent care facility and diagnosed with gastroenteritis. The patient says she did not get better and went to her family doctor, who tested her for malaria. She received a call the next day informing her that she tested positive for P. falciparum and was instructed to go to the ED immediately. Her degree of parasitemia was noted to be 7.5%, which is considered severe malaria.
On arrival to the ED the patient’s blood pressure was 85/72 mmHg and her heart rate was 146 bpm. Her initial lactate was > 5 mmol/L. Her repeat parasite density was 19%, which was an increase from 7.5% less than 24 hours prior. LFT’s were also significantly elevated with an AST > 1400 IU/L and a total bilirubin > 4 mg/dL. Her initial hemoglobin was 15 g/dL. Her platelets were noted to be only 14 k/mcL, which raised the concern for DIC, however, her fibrinogen was normal. She also had an acute kidney injury with a creatinine of 1.7 mg/dL. A chest x-ray did not show any pleural effusions, and she was not showing any signs of respiratory distress. The patient’s blood pressure improved with a 30 mL/kg bolus of Lactated Ringers. She was given a dose of doxycycline, and Infectious Disease was consulted immediately; they recommended a one-time dose of atovaquone/proguanil.
The CDC was notified within an hour of the patient arriving in the ED and flew in artesunate from Chicago. The door-to-IV-artesunate-treatment time was roughly 7 hours. She was admitted to the hospital for further management.
Malaria Background
Malaria is a disease caused by the protozoan parasite Plasmodium. According to the CDC, there are about 1700 cases of malaria per year in the U.S., 300 of which are considered severe. There are 5 known species of Plasmodium that can infect a human host. These species are P. falciparum, P. malariae, P. ovale and P. vivax. There is also P. knowlesi, which usually infects primates like the macaques but has been shown to infect humans as well. P. falciparum and P. vivax are the 2 most common species that cause malaria in humans.
The parasite spreads to humans through the bite of an infected female Anopheles mosquito. The Anopheles mosquito carries the infective form of the parasite known as sporozoites in its salivary glands. Once a human is bitten, these sporozoites travel to the liver, where they are taken up by hepatocytes. While in the hepatocytes they undergo replication and are released into circulation as merozoites, where they infect erythrocytes. How quickly the Plasmodium progresses through its life cycle depends on the species of Plasmodium. For example, P. ovale and P. vivax can lay dormant in hepatocytes for months and even years as hypnozoites. A typical incubation period is between 10 days to 4 weeks.
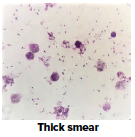
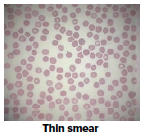
Initial symptoms include nausea, vomiting, headache, fevers, chills, diarrhea, and body aches. The gold standard for diagnosis of malaria is a peripheral blood smear.
Severe Malaria Criteria
Young children, immunocompromised patients, and pregnant women are at increased risk to develop severe malaria. Severe malaria is defined as any one of the following:
- Acid-base disturbances
- Acute renal failure
- Altered mental status
- Anemia <7
- Hyperparasitemia >5%
- Jaundice
- Pulmonary edema/ARDS
- Seizures
- Shock
Hypoglycemia and thrombocytopenia are also potential complications of malaria and should be monitored closely. Thrombocytopenia tends to be more common in P. falciparum compared to other species of Plasmodium. The degree of thrombocytopenia has not been shown to correlate with severity of infection in adults; however, a significantly low platelet count in children may be an indication of severe infection.
Treatment and Prevention of Malaria
The best treatment for malaria is prevention of malaria. This can be achieved with mosquito nets, insecticide, or anti-malarial drugs. Typical drugs used to prevent malaria are doxycycline, atovaquone/proguanil, chloroquine, mefloquine, primaquine, and tafenoquine. Which drug you use may depend on the region you are traveling to, and the susceptibilities of the drug in that given region. This patient received doxycycline, atovaquone/proguanil, and artesunate.
Artesunate is used as first-line treatment in cases of severe malaria and is thought to work by generating reactive oxygen species that damage malarial proteins. It is the only IV anti-malarial drug approved by the FDA in the U.S., and it is provided free of cost by the CDC. Pregnancy is not a contraindication for the use of artesunate in severe malaria.
Case Conclusion
While in the hospital our patient developed rhabdomyolysis and a severe kidney injury but did not require dialysis. Her parasite density was 0% after 3 doses of IV artesunate. Her LFTs and thrombocytopenia slowly resolved without any intervention. She did go on to develop a hemolytic anemia with a Hb of 7.9 g/dL on Day 4 but did not require a blood transfusion. Despite having multiorgan failure, high parasitemia, and signs of shock, the patient is expected to have a good outcome.
Take-Home Points
- Malaria is a potentially life-threatening disease caused by the Plasmodium Symptoms usually present 1–4 weeks after infection but can present months to years later depending on the species.
- Initial symptoms include nausea, vomiting, fevers, chills, and can mimic those associated with gastroenteritis or influenza, making it important to ask patients about recent travel history.
- Patients with severe malaria will have signs of end-organ damage, a high parasite density, and/or neurological findings. Once the diagnosis of severe malaria is made, the CDC will need to be notified as soon as possible in order to receive artesunate in a timely manner.
- Patients may be severely dehydrated, and aggressive hydration may be needed.
- Always encourage patients to use malaria prophylaxis and educate them on the signs and symptoms to watch out for if they travel abroad.
- Be especially cautious in pregnant patients and young children, as they are known to have increased mortality rates from malaria.
References
- CDC - Parasites - Malaria. Centers for Disease Control and Prevention. https://www.cdc.gov/parasites/malaria/index.html. Published December 11, 2019. Accessed January 25, 2020.
- CDC - Malaria - Diagnosis & Treatment (United States) - Treatment (U.S.) - Artesunate. Centers for Disease Control and Prevention. https://www.cdc.gov/malaria/diagnosis_treatment/artesunate.html. Published December 11, 2019. Accessed January 30, 2020.
- Ansari S, Khoharo HK, Abro A, Akhund IA, Qureshi F. THROMBOCYTOPENIA IN PLASMODIUM FALCIPARUM MALARIA. February 2009. http://ayubmed.edu.pk/JAMC/PAST/21-2/Ansari.pdf. Accessed January 29, 2020.
- Taylor T, Daily J, Baron E. Treatment of Severe Malaria . UpToDate. Accessed January 30, 2020.
- Anstey NM, Barber BE, William T. Non-falciparum malaria: Plasmodium knowlesi. UpToDate. Accessed January 30, 2020.



