As the U.S. struggles to flatten the ever-rising curve of COVID-19, the virus has revealed a new weakness in the health care system.
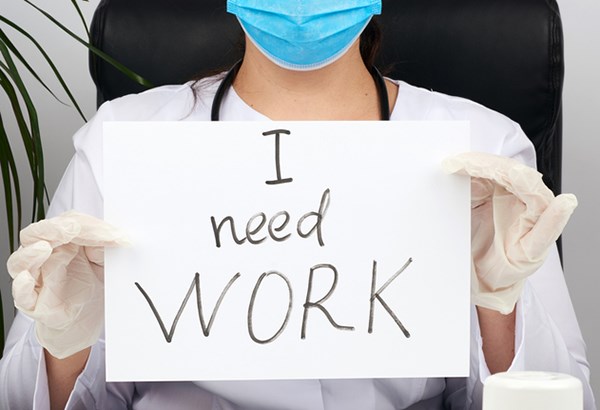
More and more patients are falling ill, and despite the fact that emergency medicine residents put their health at risk to treat them, the unimaginable is happening: Residents are becoming unemployed.
In a shocking twist, it turns out that COVID-19's latest casualty is us.
The prospect of unemployment after residency graduation is a new one, and the pandemic is directly responsible. Though workforce trends have been shifting for years, EM has kept up. Non-physician providers vied for unsupervised patient care, and EMRA leads the fight to protect your education. Residency slots increased, but graduates found jobs.
Just last year, jobs were plentiful. The class of 2020 found themselves awash with recruiters offering up to six-figure signing bonuses. Many grads signed contracts in the fall of 2019. Largely able to pick their practice setting and location, they could focus on their education and patient care without worrying about what might come next.
That started to change in the spring of 2020. COVID-19 hit. Residents started getting sick, hospitals became overwhelmed, and economic forces beyond their control started closing in. Residents across the country, once secure in their future, started to worry. Their new employers started making changes to contracts. Some cut hours. Some cut pay. And tragically, some even terminated contracts. As the class of 2021 started looking for jobs, they hit a wall. This year, they barely get interviews.
How did this happen?
In just one year, how did we go from a market that supports graduating residents to one that leaves us facing unemployment?
The problem lies at the core of our specialty. EM is the only specialty required to treat every patient who comes through the doors, day or night, regardless of their ability to pay. Our specialty embraces this social justice mission, and it is a prime reason many–including me–chose EM in the first place. But the government never provided a sustainable funding mechanism to support the EMTALA mandate. EM compensation is based on services provided, not on our 24/7 availability to manage literally any patient presentation possible.
This reimbursement model caught up with us in 2020. In the first full month of the pandemic in the U.S., EDs across the country suffered a massive drop in volume. Patient volume plunged by 40% and plateaued at a 25% drop throughout the summer. Most EDs have not recovered their volume, and their bottom lines suffered. According to an ACEP survey, 20% had layoffs, a third had furloughs, and more than half cut hours or wages.1
These changes disproportionately affect residents. Despite making as little as $15 per hour as residents, the debt is crushing. Half owe more than $200,000 in student loans. I am part of the quarter of residents who owe more than $300,000;2 that is more than the average cost of buying a home in the U.S.
Changing Course
As expected, some senior residents are trying to find alternatives to typical employment, rather than attempting to wade into the job market. More are choosing fellowships. Some are turning to urgent care.
Others are considering rural EM. EMRA is a leader in supporting rural EM training and service,3 and it is no surprise that members are looking for jobs in geographic areas that they might not have previously considered. But even those rural areas do not guarantee employment. In rural Ohio, one group has staffed their ED with 100% board certified/board eligible EM physicians for the first time ever.
With even rural groups filling up, residents struggle to get interviews anywhere. Residents are calling employers and simply being told they are not hiring this year, or that they will re-evaluate hiring decisions in the spring. This puts them in a holding pattern, casting a wider and wider net, hoping to catch a lead somewhere.
The larger political and market forces weighing down our industry should not prohibit our highly trained graduating residents from gainful employment. ACEP led a fierce fight against Medicare cuts,4 a success that helps us all. EMRA is doing our part to support our residents and protect our patients. When employers rescinded contracts, we banded together to support contract protections for graduating residents.5 EMRA also supports physician-led patient care and training, and we lead the effort to ensure resident education and training will not be compromised or diluted by non-physician providers.6
Now more than ever, the EM community, at every phase of training and career, must stand united, instead of standing by. We know we provide the very best emergency care for our patients, but we need a place to do that. We need employers to hire us. Volumes are starting to increase, and hiring new grads supports our EM community.
Give us the chance to shine.
References
- Rosenberg MS. Letter from ACEP to The Honorable Joseph R. Biden Jr. Nov. 24, 2020.
- Martin KL. Medscape Residents Salary & Debt Report 2020. Medscape. Aug. 7, 2020.
- Koski-Vacirca R, VanderVinne N, Burmeister B. Physician Shortage and Physician Workforce Challenge. In: Schlicher N, Haddock A, eds. Emergency Medicine Advocacy Handbook. 5th Dallas, TX: Emergency Medicine Residents' Association; 2019:103-110.
- American College of Emergency Physicians. Advocating Against 2021 Medicare Cuts: Update. Accessed Jan. 10, 2021.
- Emergency Medicine Residents' Association. Support of Honoring Graduating Emergency Medicine Resident Employment Contracts. April 27, 2020. Accessed Jan. 9, 2021.
- AAEM, AAEM/RSA, ACOEP, RSO, ACEP, CORD, EMRA, SAEM, SAEM-RAMS. Post-Graduate Training of Nurse Practitioners and Physician Assistants. Sept. 3, 2020. Accessed Jan. 9, 2021.