The DAWN and DEFUSE trials have expanded the window for stroke intervention. How is that affecting prehospital care?
Clinical Scenario
A 70-year-old male with a history of HTN, HLD presents to the ED via EMS for weakness and aphasia. Family is able to tell you he was last normal before he went to sleep around 11 p.m. They say he woke up at 6 a.m. mumbling and unable to speak coherently. On physical exam, he has a right-sided facial droop, loss of right arm sensation and function, and a left-sided gaze preference. It is now 11 a.m. EMS reports they did not issue a stroke alert because of an unclear onset of symptoms. The patient’s CTA demonstrates a large left-sided middle cerebral artery (MCA) stroke.
Until recent trials, this patient would be unlikely to receive an EMS stroke alert or undergo acute stroke intervention. In the 2013 American Heart Association stroke guidelines, tPA was only recommended within 4.5 hours of stroke onset, and mechanical thrombectomy was only endorsed within the first 6 hours.1 These guidelines therefore excluded a large population of patients with strokes, including those with delayed presentation to the ED, and those who awaken with stroke symptoms—and thus have an unclear time of onset. A way to increase the window for effective intervention was clearly needed.
In 2018, the DAWN and DEFUSE trials expanded the window for stroke intervention. The DAWN trial was a multicenter, randomized open label trial that specifically examined patients known to be well 6-24 hours earlier with a mismatch between clinical deficit and infarct. Patients included in the trial were randomized to receive thrombectomy or standard medical therapy. Enrolled patients had evidence of occlusion at the intracranial internal carotid artery (ICA), first MCA segment, or both. The results of the trial showed better outcomes for disability and functional independence for thrombectomy patients compared with standard medical care. For every 2 thrombectomy patients, 1 additional patient had a better outcome.2
The DEFUSE trial also examined outcomes in patients receiving thrombectomy versus standard medical care 6-16 hours after last known normal. This trial included a broader population than the DAWN trial. Specifically, the DEFUSE trial included more patients with a larger ischemic core, as well as patients with a lower National Institutes of Health Stroke Score (NIHSS) and milder symptoms. The results of the trial similarly revealed better functional outcomes for patients receiving thrombectomy as compared to standard medical care.3
As a result of these trials, the 2018 AHA Stroke Guidelines broadened the window for stroke intervention to up to 24 hours in select patients.4 Now that the window has been expanded, the question becomes: How do EMS crews identify which patients qualify as a stroke alert, and how do we direct those patients to the most appropriate ED?
In the state of Florida, EMS medical directors in different practice settings addressed the new guidelines in 2 distinct ways.
Lake County has approximately 340,000 people, but has no comprehensive stroke centers. Desmond Fitzpatrick, MD, Medical Director of Lake County EMS, needed to carefully determine which patients with stroke symptoms would benefit from direction of transport to comprehensive stroke centers an hour away. In response, Lake County adopted a field stroke scale called LAMS (the Los Angeles Motor Score) to identify patients likely to have a large vessel occlusion stroke. Patients with an elevated score are then transported to an in-county hospital capable of a rapid CTA. When that imaging identifies a large vessel cutoff, the patient receives tPA and is immediately flown to the nearest comprehensive stroke center for endovascular care.
In comparison, Alachua County has approximately 260,000 people and features 2 comprehensive stroke centers, including the University of Florida. Jason Jones, MD, the Medical Director of Alachua County Fire Rescue (ACFR), considered adopting a stroke triage scale similar to LAMS. However, he notes that in a study by Turc et al., all of the triage scores produced false negative rates exceeding 25%, and thus fail to identify a large share of patients suffering from large vessel strokes.5
Dr. Jones feels the most critical question is: “When do acute stroke symptoms stop being a time-sensitive emergency?” He asked an assembly of vascular neurologists, neurosurgeons, and emergency physicians. The consensus was “when neurologists or neurosurgeons provide definitive intervention, or when neuroimaging reveals no such intervention is needed.” As a result, in this resource-rich setting, ACFR developed a policy to issue stroke alerts for all new focal deficits less than 24 hours old. Since the majority of interventions occur in the first 6-8 hours of symptoms, a 2-tier system is necessary to appropriately use hospital resources and reduce the burden on neurologists, he said.
At the University of Florida (Gainesville), stroke alerts are now sorted into level 1 and level 2 alerts based on the patient’s time last known normal (LKN).
Figure 1.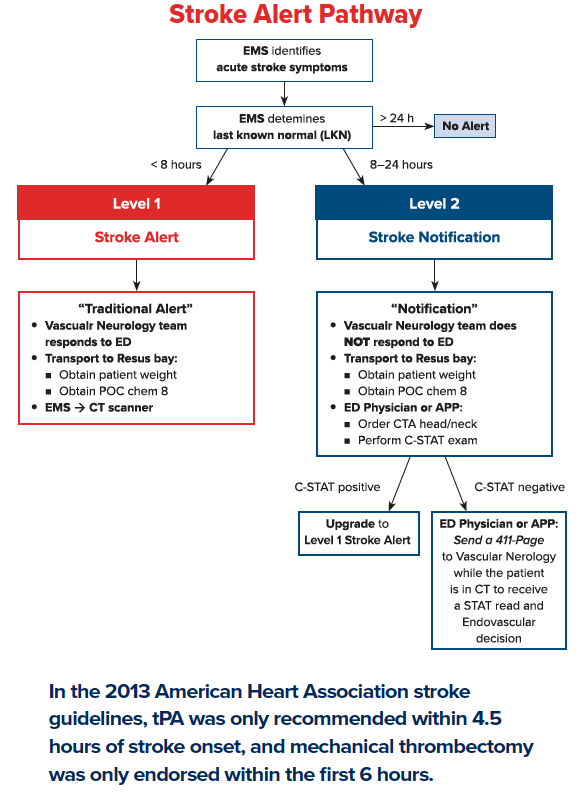
A Level 1 stroke alert is a patient with LKN 0-8 hours prior, and results in the Vascular Neurology team responding immediately to the emergency department. A Level 2 stroke alert is a patient LKN 8-24 hours prior. These patients proceed directly on the EMS stretcher and to CTA imaging, at which time the ED contacts Vascular Neurology to review the CTA remotely and determine if intervention is necessary.
An emergency physician can also upgrade the stroke alert to a level 1 if the CSTAT (Cincinnati Stroke Triage Assessment Tool) score is > 2.
Figure 2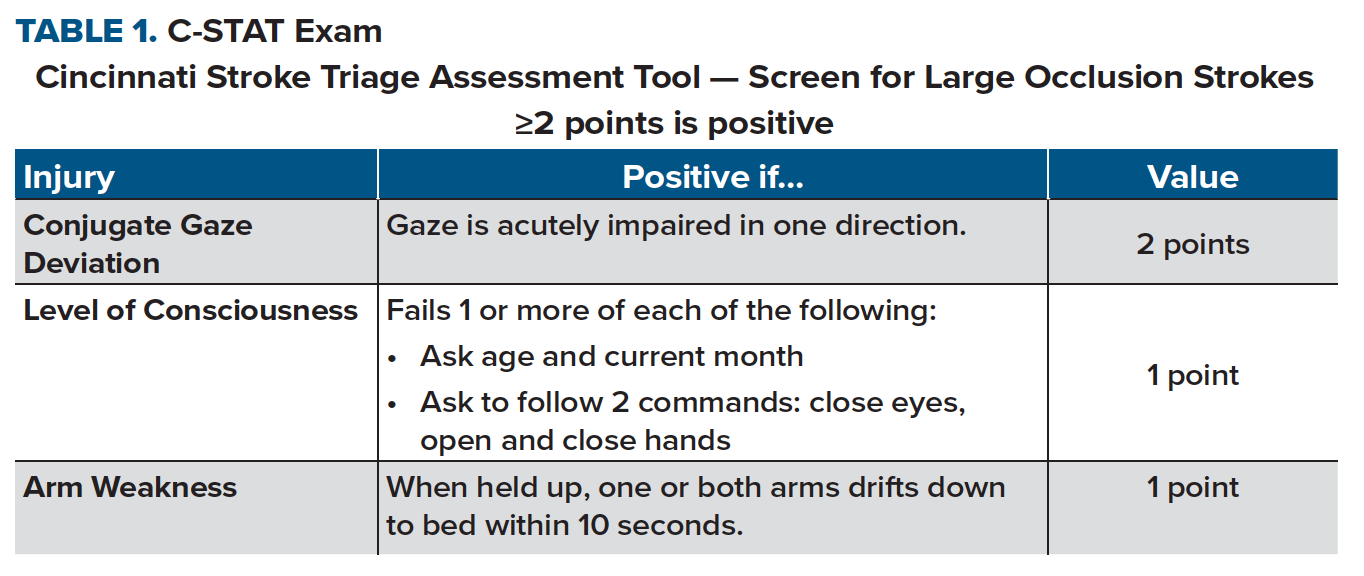
“While the 2-level system may increase the workload of our hospital stroke system, we greatly extend our ability to identify and reverse stroke deficits,” Dr. Jones said. “This process also allows EMS to distinguish patients requiring critical imaging and notify the ED before arrival. As the window widens, we have to adapt.”
The DAWN and DEFUSE trials have already changed the AHA stroke guidelines, but EMS agencies also need to adapt to the new stroke regulations. This article demonstrates 2 such adjustments: adding more detailed stroke scales and expediting transport protocols. Regardless of the method agencies choose to adopt, change must occur in order to provide the best possible patient care.
References
1. Jauch EC, Saver JL, Adams Jr HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
2. Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11-21.
3. Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718.
4. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e99.
5. Turc G, Maïer B, Naggara O, et al. Clinical Scales Do Not Reliably Identify Acute Ischemic Stroke Patients With Large-artery Occlusion. Stroke. 2016;47(6):1466-1472.
Interviewees
Jason Jones, MD, FACEP, Asst. Professor, University of Florida Health
Desmond Fitzpatrick, MD, FACEP, Asst. Professor, University of Florida Health



