Management of a pregnant trauma patient can be challenging, you must be aware of the anatomical and physiological changes of pregnancy in addition to the clinical implications these changes have in a trauma setting.
It is important to keep in mind that the mother’s wellness is a priority during resuscitation of pregnant trauma patients as fetal outcome is largely dependent on aggressive and early resuscitation of the mother. This concise review article highlights key concepts in the management of a pregnant trauma patient.
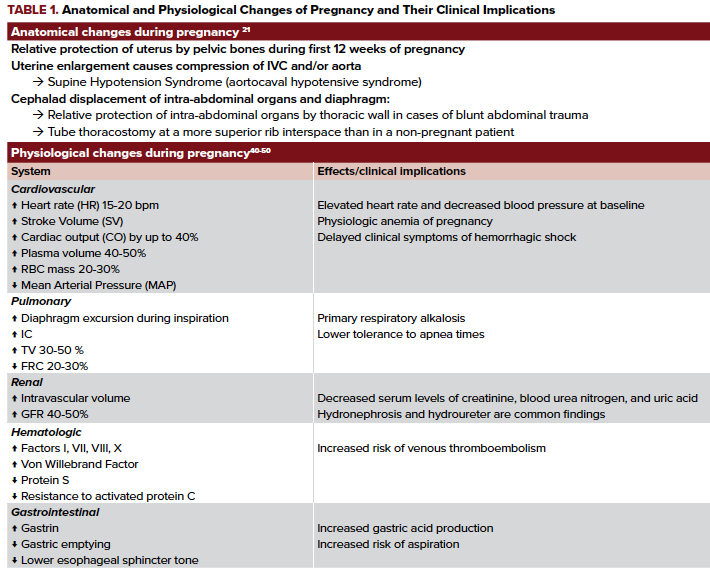
Table 1 provides an overview of the anatomic and physiologic changes of pregnancy.
Pre-hospital care
The pre-hospital care of pregnant trauma patients focuses on rapid assessment, adequate stabilization, and transport to the nearest appropriate medical facility. It is recommended to place pregnant women in the left lateral decubitus position in order to alleviate compression on the inferior vena cava (IVC) and improve hemodynamics.1 The 2015 American Heart Association guidelines on cardiac arrest in pregnancy recommend placing pregnant women in supine position with manual displacement of the uterus superiorly and laterally towards the left due to improved quality of chest compressions and ease of performing resuscitation procedures (eg, intubation). These same recommendations should be followed when possible when cardiac arrest is secondary to trauma. Additional resuscitative measures include obtaining intravenous (IV) access, leg elevation, and supplemental O2 administration.2
ED Assessment and Management
Primary Survey
The ED management of the pregnant trauma patient should ideally consist of a multidisciplinary approach. If possible, the trauma and obstetrical teams should be activated early. Additionally, the neonatal intensive care unit should be consulted as early as possible in preparation for a potential infant resuscitation.
- Airway
Pregnant patients have altered respiratory physiology resulting in a decreased functional reserve capacity (FRC), increased oxygen demand, and thus lower tolerance to prolonged apnea times. Therefore, a pregnant trauma patient should be preoxygenated adequately when the airway needs to be secured. Airway management is further complicated due to increased edema, hyperemia, and friability of the mucosa of the upper airway in pregnant women and may result in an increase in the Mallampati score.3 In the pregnant population, the rate of failed tracheal intubation is 0.4%, ten times higher than for the non-pregnant population (0.04%).4 The application of cricoid pressure has been recommended despite the lack of evidence supporting its benefit.5,6 Because of the decreased esophageal sphincter tone during pregnancy, there is an elevated risk of aspiration.7 To reduce this risk of aspiration, an orogastric tube placement should follow intubation.8
- Breathing
Evaluation of respirations in the pregnant patient mirrors what is done in the non-pregnant patient. As noted in Table 1, PaCO2 is reduced in pregnancy. A normal or elevated PaCO2 may represent pending respiratory failure. Due to the elevation of the diaphragm that occurs during pregnancy, management of a pneumothorax proceeds with placement of a tube thoracostomy 1 to 2 intercostal spaces superior to the usual 4th or 5th intercostal space anterior to the mid-axillary line.8
- Circulation
All trauma patients should have 2 large-bore IV cannulas placed to aid with volume resuscitation. Shock may be due to hemorrhage, direct cardiac injury, or obstructive mechanisms such as tamponade or tension pneumothorax. The uterus should be displaced manually or by placing the patient in left lateral decubitus position. When transfusion is necessary, the risk of alloimmunization in the Rh (-) mother is reduced by administering un-crossmatched type O, Rh (-) blood until type specific blood is available.9
- Disability
Disability assessment is a rapid neurologic assessment that includes a Glasgow Coma Scoring, pupillary examination, as well as an evaluation for lateralizing neurological deficits. - Exposure and environmental control
As in the general population, the patient should be fully exposed and thoroughly assessed. Hypothermia should be prevented in order to avoid the "trauma triad of death" - a vicious cycle involving hypothermia, coagulopathy, and acidosis.10
Secondary Survey
History
In addition to obtaining a thorough obstetrical history, providers can use the mnemonic AMPLE (allergies, medications, past illnesses/pregnancies, last meal, events/environment related to trauma) to aid in history taking.11
Fetal assessment
Ultrasound can be utilized to assess fetal heart rate, fetal movement, amniotic fluid quantity, position of the placenta, as well as fetal femur length for calculating gestational age. A femur length > 4 cm is suggestive of viability.12 A pregnant patient with a viable fetus (more than 22 to 24 weeks) should undergo continuous fetal cardiotocographic monitoring for a minimum of 4 hours. The presence of prolonged, painful, and/or regular contractions necessitates further monitoring or obstetric intervention.
Physical exam
Uterine tenderness, vaginal bleeding, and pooling of fluid in the vagina are indicators of possible complications with the uterus. Bimanual exam should be avoided when rupture of membranes is suspected. If the gestational age is > 23 weeks, speculum exam should be deferred until placenta previa is ruled out. While examining the vagina, the physician should also assess for the presence of lacerations or bony fragments.
Imaging Studies
Focused assessment with sonography for trauma (FAST) is less accurate in pregnant patients, although serial FAST exams may improve the accuracy.13 Due to low sensitivity, ultrasound should not be used to rule out retroperitoneal hemorrhage or placental abruption. Addition of lung windows to the FAST exam is known as the extended FAST (eFAST) exam. Lung ultrasound is more sensitive and has similar specificity as supine anteroposterior chest radiographs.14
Laboratory Testing
Lab testing largely follows what would be done in most patients with traumatic injuries. The Rh status should be determined as Rh (-) patients are at risk of alloimmunization. Fibrinogen levels are often elevated in pregnancy15,16 and low fibrinogen levels are associated with severe hemorrhage or the development of disseminated intravascular coagulation (DIC). The Kleihauer-Betke (KB) test is used to detect the approximate the volume of fetal-maternal hemorrhage (FMH) but its lower limit of sensitivity does not allow this test to rule out the presence of FMH. The formula used is:
% of fetal cells determined by KB test/100 x 5,000 ml = volume of FMH (in mls).17
Flow cytometry is a superior alternative test for estimating the volume of FMH but it is rarely available in most hospitals.18,19 Evaluation for prelabor rupture of membranes (PROM) is done by testing vaginal fluid for the presence of ferning, higher pH (vaginal pH is 5 vs amniotic fluid pH is 7), or for the presence of specific amniotic proteins such as IGFBP-1 and AFP.20
Medications
- Rho(D) immune globulin (anti-D IgG, Rhogam)
It is recommended that anti-D IgG is administered within 72 hours to all Rh (-) pregnant trauma patients at risk of FMH.21 The standard dose of 300 mcg administered intramuscularly is effective at preventing alloimmunization to 30 mL of fetal blood. The need for additional doses of anti-D IgG is determined by the results of KB testing or less frequently flow cytometry.22 - Corticosteroids
For imminent delivery of a viable fetus between 24- and 34-weeks gestational age, corticosteroids (e.g. betamethasone or dexamethasone) given over a period of 24 hours before birth or even in single doses has been shown to reduce overall neonatal morbidity and mortality.23 - Tocolytics
The role of tocolytics in pregnant trauma patients is widely controversial. Their use might be valuable when delaying delivery is vital for administering important medications such as magnesium sulfate or corticosteroids.24 Tocolytics that have beta adrenergic activity (e.g. terbutaline) should be avoided in the trauma setting as they may cause tachycardia and/or hypotension. 25 - Tranexamic Acid
In the setting of pregnancy, tranexamic acid (TXA) has been used to prevent complications from postpartum hemorrhage. Results of the World Maternal Antifibrinolytic (WOMAN) trial demonstrated that the use of TXA in postpartum hemorrhage resulted in lower reported outcomes of death (TXA 1.5% vs Placebo 1.9%), with most benefit seen in patients who received TXA between 1 and 3 hours of delivery.26 Multiple studies have studied the utility of TXA in the trauma setting; however, none have looked specifically at the use of TXA in pregnant trauma patients. The CRASH-2 trial showed that TXA administration significantly decreased all-cause mortality due to trauma by 1.5% (14.5% in TXA group vs 16.0% in placebo group).27,28 Similarly, results from the retrospective MATTERS study showed that TXA administration in a trauma setting was associated with reduction in unadjusted mortality (TXA 17.4% vs No TXA 23.9%).29 The dose of TXA frequently used is 1 g infused over 10 minutes, followed by an infusion of 1 g over eight hours.
Complications Specific to Trauma in Pregnancy
Placental abruption is the second highest cause of perinatal mortality from trauma.6 The diagnosis is often made clinically with cardiotocographic fetal monitoring.30,31 Because 40% of abruption hemorrhages are retroperitoneal, computed tomography (CT) imaging is more sensitive for diagnosis than ultrasonography.32 Uterine rupture is another dangerous complication of trauma, with a fetal mortality rate of almost 100%.25 If present, examination may reveal an irregularly shaped uterus, palpable fetal parts, or abdominal tenderness. Prompt laparotomy with fetal delivery and either hysterectomy or uterine repair is the treatment of choice. Amniotic fluid embolism (AFE) presents with sudden hypoxemia and cardiovascular collapse and can progress to DIC and multi-organ failure. The mechanism of AFE is hypothesized to be amniotic fluid entering the maternal circulation and leading to either vascular obstruction or anaphylaxis. Treatment is supportive with resuscitation and potential delivery of the fetus.33 The risk of preterm labor, preterm premature rupture of membranes (PPROM), or PROM is significantly higher after traumatic injury and may not present immediately after the injury.34
Perimortem Cesarean Section
Perimortem cesarean delivery is considered a life-saving procedure for both the mother and the fetus as it alleviates the compression of the IVC by the uterus and thus improves maternal hemodynamics and fetal perfusion. Ideally, but rarely in practice, the procedure should commence within 4 minutes of the arrest with delivery of the fetus one minute later.35,36 There are reports in the literature showing fetal survival even if delivered 30 minutes after arrest.37 Procedural success can be optimized by contacting an obstetrician and a neonatologist, as well as ensuring that an incubator, pediatric crash cart, and surgical tools are available.38
The first step in the procedure is to perform a vertical incision through the skin of the abdominal wall, starting from the pubic symphysis and extending to the xiphoid process. The subcutaneous tissue is bluntly dissected to expose the peritoneum, which is then cut. The uterus should be delivered anteriorly in order to improve visualization. Generally, the uterine incision should be performed on the inferior aspect of the uterus owing to the usual superior location of the placenta. However, if the location of the placenta is already known, then the incision should be performed opposite to that location. If the placenta is located anteriorly, then it should be cut through in order prevent delay in delivery. After delivering the fetus, the cord is clamped and cut immediately, and the fetus is transferred to an assistant for resuscitation. The placenta should be delivered manually, followed by packing of the uterus. If there is return of spontaneous circulation, uterine massage and oxytocin administration may be necessary to prevent atony. Oxytocin should be infused slowly in order to prevent hypotension.39
Conclusion
Management of traumatic injuries in pregnant patients requires careful evaluation with an understanding of the alterations in anatomy and physiology that occur during pregnancy. Standard evaluation of pregnant patients proceeds in the usual fashion as for non-pregnant patient with primary attention to the A-B-Cs of trauma care. Interpretation of vital signs and lab tests may be different for the pregnant patient. To optimize the potential for good outcomes for the mother and the fetus, resuscitation of the mother takes priority.
References
- Humphries A, Mirjalili SA, Tarr GP, Thompson JMD, Stone P. Hemodynamic changes in women with symptoms of supine hypotensive syndrome. Acta Obstet Gynecol Scand. 2019.
- Jeejeebhoy FM, Zelop CM, Lipman S, et al. Cardiac Arrest in Pregnancy: A Scientific Statement From the American Heart Association. Circulation. 2015;132(18):1747-1773.
- Basaranoglu G, Columb M, Lyons G. Failure to predict difficult tracheal intubation for emergency caesarean section. Eur J Anaesthesiol. 2010;27(11):947-949.
- Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42(5):487-490.
- El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg. 2010;110(5):1318-1325.
- Mushambi MC, Kinsella SM, Popat M, et al. Obstetric Anaesthetists' Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia. 2015;70(11):1286-1306.
- Robinson M DA. Aspiration under anaesthesia: risk assessment and decision-making. Continuing Education in Anaesthesia, Critical Care & Pain. 2014;14(4):171-175.
- Jain V, Chari R, Maslovitz S, et al. Guidelines for the Management of a Pregnant Trauma Patient. J Obstet Gynaecol Can. 2015;37(6):553-574.
- Committee on Practice B-O. Practice Bulletin No. 181: Prevention of Rh D Alloimmunization. Obstet Gynecol. 2017;130(2):e57-e70.
- Holcomb JB, Jenkins D, Rhee P, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62(2):307-310.
- MacArthur B, Foley M, Gray K, Sisley A. Trauma in Pregnancy: A Comprehensive Approach to the Mother and Fetus. Am J Obstet Gynecol. 2019;220(5):465-468 e461.
- Oxford CM, Ludmir J. Trauma in pregnancy. Clin Obstet Gynecol. 2009;52(4):611-629.
- Blackbourne LH, Soffer D, McKenney M, et al. Secondary ultrasound examination increases the sensitivity of the FAST exam in blunt trauma. J Trauma. 2004;57(5):934-938.
- Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010;17(1):11-17.
- Hellgren M, Blomback M. Studies on blood coagulation and fibrinolysis in pregnancy, during delivery and in the puerperium. I. Normal condition. Gynecol Obstet Invest. 1981;12(3):141-154.
- James D, Steer P, Weiner C, et al. Pregnancy and laboratory studies: a reference table for clinicians. Obstet Gynecol. 2010;115(4):868; author reply 868-869.
- Kim YA, Makar RS. Detection of fetomaternal hemorrhage. Am J Hematol. 2012;87(4):417-423.
- Fernandes BJ, von Dadelszen P, Fazal I, Bansil N, Ryan G. Flow cytometric assessment of feto-maternal hemorrhage; a comparison with Betke-Kleihauer. Prenat Diagn. 2007;27(7):641-643.
- Porra V, Bernaud J, Gueret P, et al. Identification and quantification of fetal red blood cells in maternal blood by a dual-color flow cytometric method: evaluation of the Fetal Cell Count kit. Transfusion. 2007;47(7):1281-1289.
- Bushman ET, Theilen LH, Monson M, Hammad I, Esplin I, Esplin MS. Effect of blood contamination on amniotic fluid detection in vitro using immunoassays. J Matern Fetal Neonatal Med. 2019:1-4.
- Surgeons ACo. In: American College of Surgeons, Committee on Trauma. Advanced Trauma Life Support Student Course Manual. 10 ed. Chicago, IL2018.
- Fung KFK, Eason E. No. 133-Prevention of Rh Alloimmunization. J Obstet Gynaecol Can. 2018;40(1):e1-e10.
- Committee on Obstetric P. Committee Opinion No. 713: Antenatal Corticosteroid Therapy for Fetal Maturation. Obstet Gynecol. 2017;130(2):e102-e109.
- Haram K, Mortensen JH, Nagy B. Genetic aspects of preeclampsia and the HELLP syndrome. J Pregnancy. 2014;2014:910751.
- Greco PS, Day LJ, Pearlman MD. Guidance for Evaluation and Management of Blunt Abdominal Trauma in Pregnancy. Obstet Gynecol. 2019;134(6):1343-1357.
- Collaborators WT. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105-2116.
- collaborators C-t, Shakur H, Roberts I, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376(9734):23-32.
- collaborators C-, Roberts I, Shakur H, et al. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet. 2011;377(9771):1096-1101, 1101 e1091-1092.
- Morrison JJ, Dubose JJ, Rasmussen TE, Midwinter MJ. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) Study. Arch Surg. 2012;147(2):113-119.
- Kadasne AR, Mirghani HM. The role of ultrasound in life-threatening situations in pregnancy. J Emerg Trauma Shock. 2011;4(4):508-510.
- Myers SP, Kutcher ME, Rosengart MR, et al. Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism. J Trauma Acute Care Surg. 2019;86(1):20-27.
- Lucia A, Dantoni SE. Trauma Management of the Pregnant Patient. Crit Care Clin. 2016;32(1):109-117.
- Kaur K, Bhardwaj M, Kumar P, Singhal S, Singh T, Hooda S. Amniotic fluid embolism. J Anaesthesiol Clin Pharmacol. 2016;32(2):153-159.
- Sperry JL, Casey BM, McIntire DD, Minei JP, Gentilello LM, Shafi S. Long-term fetal outcomes in pregnant trauma patients. Am J Surg. 2006;192(6):715-721.
- Einav S, Kaufman N, Sela HY. Maternal cardiac arrest and perimortem caesarean delivery: evidence or expert-based? Resuscitation. 2012;83(10):1191-1200.
- Benson MD, Padovano A, Bourjeily G, Zhou Y. Maternal collapse: Challenging the four-minute rule. EBioMedicine. 2016;6:253-257.
- Katz V, Balderston K, DeFreest M. Perimortem cesarean delivery: were our assumptions correct? Am J Obstet Gynecol. 2005;192(6):1916-1920; discussion 1920-1911.
- Eldridge AJ, Ford R. Perimortem caesarean deliveries. Int J Obstet Anesth. 2016;27:46-54.
- Parry R, Asmussen T, Smith JE. Perimortem caesarean section. Emerg Med J. 2016;33(3):224-229.
- Cheung KL, Lafayette RA. Renal physiology of pregnancy. Adv Chronic Kidney Dis. 2013;20(3):209-214.
- Croles FN, Nasserinejad K, Duvekot JJ, Kruip MJ, Meijer K, Leebeek FW. Pregnancy, thrombophilia, and the risk of a first venous thrombosis: systematic review and bayesian meta-analysis. BMJ. 2017;359:j4452.
- Gomes CF, Sousa M, Lourenco I, Martins D, Torres J. Gastrointestinal diseases during pregnancy: what does the gastroenterologist need to know? Ann Gastroenterol. 2018;31(4):385-394.
- Hegewald MJ, Crapo RO. Respiratory physiology in pregnancy. Clin Chest Med. 2011;32(1):1-13.
- Mackersie RC. Pitfalls in the evaluation and resuscitation of the trauma patient. Emerg Med Clin North Am. 2010;28(1):1-27, vii.
- Petrone P, Asensio JA. Trauma in pregnancy: assessment and treatment. Scand J Surg. 2006;95(1):4-10.
- Rasmussen PE, Nielsen FR. Hydronephrosis during pregnancy: a literature survey. Eur J Obstet Gynecol Reprod Biol. 1988;27(3):249-259.
- Rybstein MD, DeSancho MT. Risk factors for and clinical management of venous thromboembolism during pregnancy. Clin Adv Hematol Oncol. 2019;17(7):396-404.
- Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014;130(12):1003-1008.
- Tan EK, Tan EL. Alterations in physiology and anatomy during pregnancy. Best Pract Res Clin Obstet Gynaecol. 2013;27(6):791-802.
- Townsley DM. Hematologic complications of pregnancy. Semin Hematol. 2013;50(3):222-231.



