POCUS for the Win is a case series for ultrasound enthusiasts to showcase the ability of ultrasound in making diagnoses at the bedside, often before formal imaging. In this case POCUS is used to diagnose popliteal artery occlusion.
If you have a case with accompanying imaging/video, please email pocusftw@gmail.com.
Case
A 45-year-old female with a history of peripheral artery disease and a stable abdominal aortic aneurysm presents to the Emergency Department for right leg pain. Patient notes sudden onset of right lower leg pain while walking at the grocery store several hours prior to arrival. She denies trauma to the leg. The review of systems is otherwise negative. The physical exam is significant for full strength and intact sensation to the right leg. Patient had decreased pulses in the dorsalis pedis but normal pulses in the posterior tibialis. At the community hospital where this patient presented, ultrasound was not available overnight. Ultrasound was brought in to perform at bedside to rule out DVT in the leg.
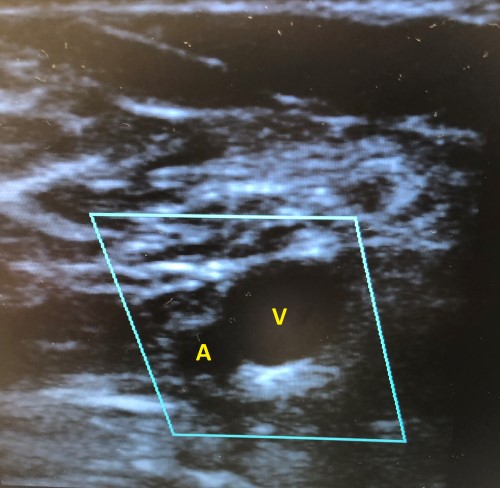
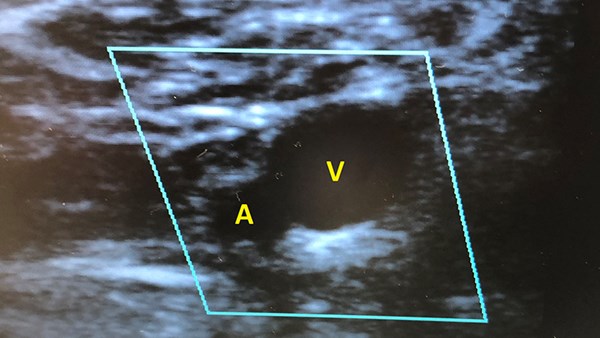
Figure 1. Bedside ultrasound of patient's right popliteal fossa with popliteal artery (A) and vein (V) visualized with color flow on.
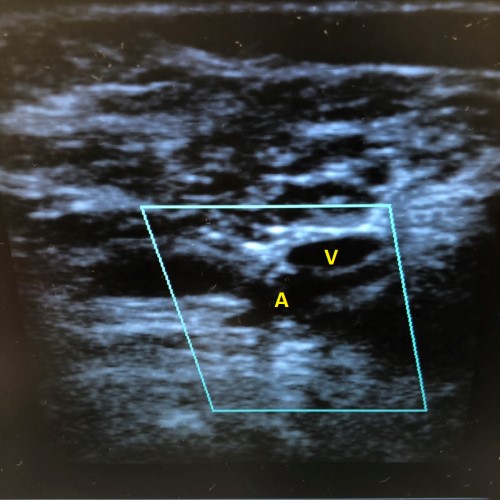
Figure 2. Bedside ultrasound of patient's right popliteal fossa while compressing popliteal artery (A) and vein (V) with color flow on.
Diagnosis: Acute right popliteal artery occlusion
In the ultrasound images above, the patient had a compressible popliteal vein but no color flow through the popliteal artery or vein. The patient was accepted for transfer to a tertiary care center based on the ultrasound imaging. The accepting hospital asked for a CT angiogram of the leg prior to transfer to begin focused interventional planning while the transfer process was initiated. The diagnosis of acute right popliteal artery occlusion was confirmed on CT angiogram. A heparin drip was started, and the patient was transferred out.
Ultrasound Review: DVT Exam
Deep Venous thrombosis (DVT) affects approximately 1 per 1,000 annually. Due to a combination of high disease incidence as well as the morbidity and mortality associated with the progression from DVT to pulmonary embolism (PE), it is important to be able to rule in or rule out a DVT in the emergency department.1 Learning how to perform a bedside DVT exam is essential, especially in the many facilities (such as the one described in the case above) that lack access to 24-hour ultrasound.2
Technique
To perform a lower extremity venous ultrasound, a high resolution (5-10 MHz) linear transducer is required. Physicians can quickly assess for a DVT by performing the 2-point compression technique. Performing the 2-point compression technique does not assess clots in the calf and ankle. Color and Doppler modes can be utilized to differentiate between vascular and non-vascular structures, and for blood flow - this feature was critical in making the correct diagnosis in the case above.
- Place the patient supine with 20-30° of reverse Trendelenburg position for maximal distension of the leg veins.
- Externally rotate the hip with the knee slightly flexed, to allow for optimal exposure of the junction of the common, deep, and superficial femoral veins as well as the popliteal fossa.1,2
- With the probe in transverse orientation, apply direct and even pressure at the anatomical positions depicted below in Figures 4 and 5 to assess for compressibility. The complete exam is described in further detail in the following section.
- If the vein fully compresses, then a DVT can be ruled out. An appropriate amount of pressure will result in complete collapse of the vein and only a slight change in the caliber of the artery. If the vein does not fully compress, a DVT is most likely present.2 The lumen of the vein must disappear completely in order to exclude the presence of a clot. While a clot may be seen as echogenicity within the lumen, in many cases the only evidence of DVT will be the inability to compress the vein fully.1 See Figure 3 below for an example of a positive DVT study.
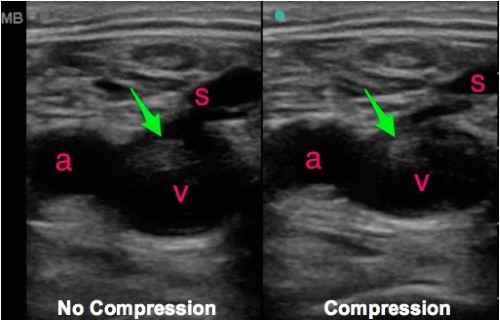
Figure 3: Positive DVT study that shows a thrombus (indicated by the green arrow) in the femoral vein (V). The femoral artery (a) is seen adjacent to the vein (v) and also the greater saphenous vein (s) is in view. The image on the right demonstrates that the vein does not collapse with compression which indicates a positive DVT study.3
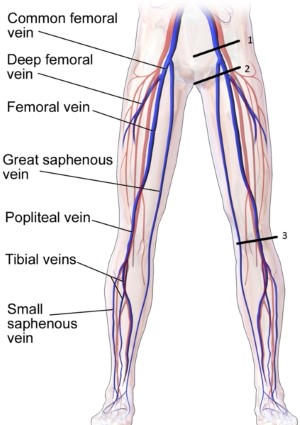
Figure 4. Lower extremity venous vasculature4
Femoral Vein
To begin examining the femoral vein, the linear probe is placed in the transverse plane at the level of the inguinal ligament. The probe indicator should be pointed to the patient’s right. In this orientation, the vein will be imaged in cross-section with the femoral artery lateral to the femoral vein. Fan the probe proximally or distally until the confluence of the femoral vein and greater saphenous is visualized. Then advance the probe up to 5 cm distal from the confluence of the greater saphenous and common femoral veins until the common femoral vein gives rise to the deep and superficial femoral veins. Both are considered deep veins and should be evaluated.2

Figure 5. Transducer location to evaluate the femoral artery and vein. Normal ultrasound images showing common femoral artery (A) and femoral vein (V) as well as a fully compressible femoral vein (V).3
Popliteal Vein
The probe is again placed in a transverse plane relative to the long axis of the popliteal veins. Starting at the posterior medial aspect of the knee, first locate the superficial popliteal artery and vein. Due to the posterior location of the probe, the popliteal vein sometimes will appear more superficial than the popliteal artery. Once the structures are in view, direct pressure should be applied to assess the compressibility of the popliteal vein. The probe then should be fanned through the popliteal vein until it gives rise to the anterior, posterior, and tibial veins. The compressibility of the proximal portion of each of the veins involved in the trifurcation must also be evaluated. Total collapse of the veins rule out the presence of a DVT.2
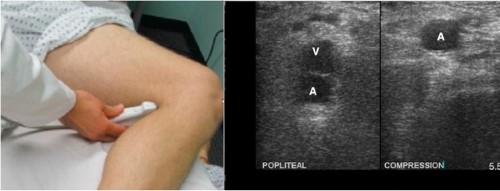
Figure 6: Transducer location to evaluate the popliteal vein. Normal image showing a popliteal artery (A) and vein (V) as well as a fully compressible vein (V).3
Check out this video for a walkthrough of the DVT exam: https://www.coreultrasound.com/dvt/
Take-Home Points
- DVT is a major cause of morbidity and mortality.
- Physicians can quickly assess for DVT by performing a 2-point compression test.
- Linear probe is used to assess the femoral and popliteal veins. Curvilinear probe may be used in obese or edematous patients.
- Assess for DVT in femoral vein at the confluence of the saphenous vein and femoral vein, compressing above and below the saphenofemoral junction.
- Assess for DVT in popliteal vein just posterior to the knee and superficial to the popliteal artery.
- Vein must fully collapse to rule out clot.2
- A non-compressible vein can be mistaken for an artery, leading to a false negative result. Conversely, a non-compressible artery may be mistaken for a vein, leading to a false positive result. The use of color Doppler can help mitigate these sources of error.
- Lymph nodes may be confused with noncompressible vein and if found, can be identified by moving up or down 1 cm.
References
- Rios D., Lewis S, et al. Emergency Ultrasound For Deep Vein Thrombosis. ACEP Now. Published February 3, 2015.
- Dawson M, Mallin M. Lung. Introduction to Bedside ultrasound: Volume 2. Emergency Ultrasound Solutions; 2013: 202-208
- Greenwood Erickson M, Rempell J, Stone M. Ultrasound DVT Assessment. ALiEM Cards. Published February 18, 2015.
- Schoeman D. DVT ultrasound. WikEM. Published December 31, 2019.