An important goal for cardiac point-of-care ultrasound (POCUS) curricula is creating a straightforward method of remembering ultrasound probe orientation. This facilitates the acquisition of the standard clinical images needed for quality assurance (QA).
Proposal: To associate the cardiac images to the hours on a clock to enhance memorization and optimize image acquisition
5 Views
Five cardiac ultrasound views constitute a focused cardiac assessment. These include the parasternal long axis (PSL), parasternal short axis (PSS), apical four chamber (A4), subxiphoid (SX), and inferior vena cava (IVC) views.1–4
Obtaining all five views helps to assess for effusion, contractility, and relative chamber size.3,4
The five views are critical in assessing the 5 E’s: Effusion, Ejection, Equality, Exit, and Entrance.4
- Effusion: Assesses for effusion and tamponade physiology
- Ejection: Assesses left ventricular ejection fraction
- Equality: Assesses for a normal RV:LV size ratio, which is typically less than 0.6:1. An equal 1:1 ratio would be concerning for right heart strain.
- Exit: Evaluates the aorta for abnormal enlargement of the aortic root
- Entrance: Evaluates the IVC for plethora. High IVC collapsibility is present in hypovolemia, while plethora is present in congestive heart failure and obstructive conditions such as tamponade.4
Convention
There are 2 accepted methods of cardiac ultrasound orientation.
- Cardiology specialty convention: Has the indicator on the right of the screen, and achieves PSL by pointing the probe indicator to the right shoulder2,4
- Emergency medicine (EM) convention: Has the indicator on the left of the screen, and achieves PSL by pointing the probe indicator to the left hip. The EM convention achieves all cardiac views by pointing the probe indicator 180 degrees from the cardiology convention views.2,4
In the cardiology convention:
- PSL and PSS views are in the 2nd to 5th intercostal spaces, left of the sternum.
- PSL: Probe indicator points to the right shoulder.
- PSS: Probe indicator points to the left shoulder.
- A4: View is inferior to the left nipple, in the inframammary fold, with the indicator pointing laterally to the left trunk.
- SX: View is acquired by utilizing the liver as an acoustic window, and placing the probe inferior to the xiphoid process, with the probe indicator pointing laterally to the left trunk.
- IVC: View is inferior to the xiphoid, with the probe indicator pointing caudally to the feet.3
This proposal utilizes the cardiology convention of ultrasound orientation.
Clockwise Approach
A clockwise approach is mentioned in multiple ultrasound references for 2 of the cardiac views. The recommendation is to start at the PSL view and turn clockwise 90 degrees to achieve the PSS view.2,3,5
However, a direct comparison to an analog clock as a guide for all 5 cardiac views is less common. Some POCUS teaching resources do utilize the hands of the clock to guide the cardiac views, although these sources have differing recommendations about optimal hour times for each cardiac view.6,7
There is not yet a proposed standard clock guide that has been integrated into multiple teaching references and widely incorporated into academic curricula.
Utilizing the cardiology convention for ultrasound orientation, a clock guide is proposed here to achieve the 5 cardiac views.
Proposed Clock Guide to the 5 Views
Achieving the 5 views requires multiple changes in the probe position and indicator orientation on the anterior torso.
Learning the probe positions and indicator orientations by rote without a memorization tool can pose a significant obstacle to obtaining clinical views. An incorrectly placed probe leads to off axis and flipped images, which can cause substandard cardiac images and prevent clinical diagnoses.
The proposed clock guide utilizes an analog clock superimposed over the anterior torso of a human model. 12 o’clock is to the head, 3 o’clock to the left arm, 6 o’clock to the feet, and 9 o’clock to the right arm (Figure 1). Learners are asked to imagine a clock on the chest of the patient.

Figure 1: Analog clock superimposed on a human torso
Question: What if learning the probe indicator orientations could be straightforward, like clockwork?
Approach: There are 2 integrated concepts to memorize, to achieve great resolution cardiac views. The 2nd concept utilizes the clock guide.
- Anatomic sites: The 3 anatomic sites to place the probe (Figure 2).
a. Site 1: PSL and PSS in the 2nd-5th intercostal spaces, left of sternum
b. Site 2: A4 in left inframammary fold, inferior to nipple or inferolateral
c. Site 3: SX and IVC inferior to the xiphoid process. - Probe indicator orientations: There are 4 probe indicator orientations to achieve the 5 cardiac views.
a. The cardiac views are achieved by rotating the probe clockwise, with the probe indicator orientation following the hours of the clock, while achieving the 5 views in order: PSL, PSS, A4, SX, IVC.
b. Probe indicator orientations for PSL, PSS, A4, SX, IVC: 10:30, 1:30, 3, 3, 6 (Figure 3)
c. The probe must be positioned on the appropriate anatomic location of the torso for each view, while utilizing the clock to guide the indicator orientation.
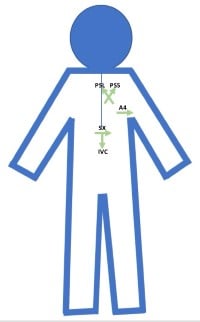
Figure 2: Three anatomic sites to place the probe to achieve the 5 cardiac views: PSL and PSS at site 1, A4 at site 2, SX and IVC at site 3
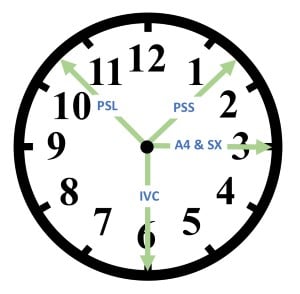
Figure 3: Five cardiac views by hour time, achieved by rotating clockwise, 10:30, 1:30, 3, 3, 6: PSL at 10:30, PSS at 1:30, A4 at 3, SX at 3, IVC at 6
The 5 Views by Rotating Clockwise
Parasternal Long
For PSL, the probe is located in the 2nd to 5th intercostal spaces, left of the sternum.
PSL axis is achieved by pointing the probe indicator to the right shoulder.
Orient the probe indicator to 10:30 o’clock (Figure 4) to achieve the PSL view (Figure 5).
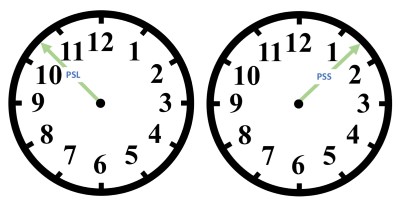
Figure 4: PSL at 10:30 and PSS at 1:30
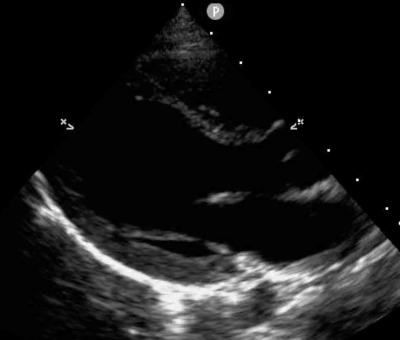
Figure 5: PSL ultrasound image
Parasternal Short
PSS is achieved by rotating 90 degrees clockwise from the PSL view, pointing the probe indicator to the left shoulder.
Orient the probe indicator to 1:30 o’clock (Figure 4) to achieve the PSS view (Figure 6).
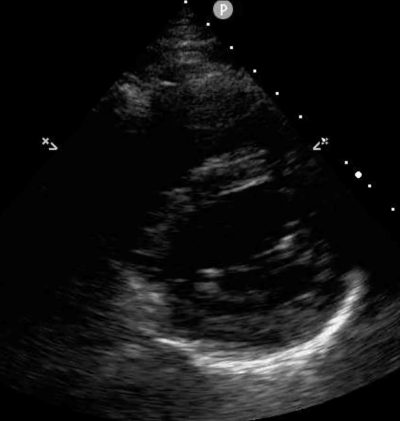
Figure 6: PSS ultrasound image
Apical Four
For A4, the probe is placed inferior to the left nipple in the left inframammary fold.
A4 view is achieved by rotating clockwise to 3 o’clock.
Orient the probe indicator to 3 o’clock (Figure 7) to achieve the A4 view (Figure 8).
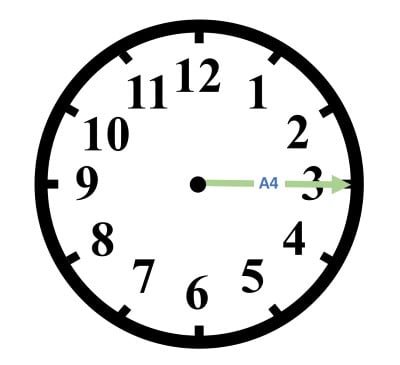
Figure 7: A4 at 3
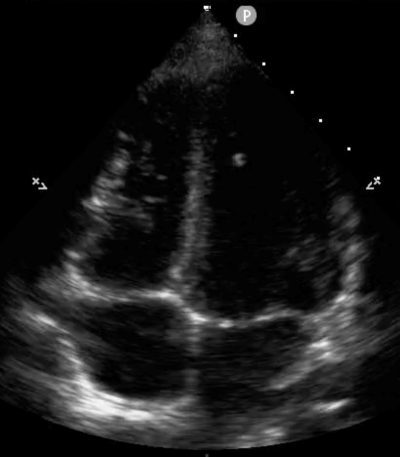
Figure 8: A4 ultrasound image
Optimizing the A4 view:
- Probe position: The probe may need to be maintained inferior to the left nipple, or slid laterally within the rib space (between the mid-clavicular line and the anterior axillary line) to achieve a classic 4 chamber view, depending on variations in anatomy.
- Orientation: A mild counterclockwise rotation from 3 o’clock may be required (5-10 degrees) to achieve a vertical septum when viewing the 4 chambers.
Subxiphoid
For SX, the probe is placed inferior to the xiphoid process, and the probe is angled so that it is viewing the heart in the left chest.
Orient the probe indicator to 3 o’clock (Figure 9) to achieve the SX view (Figure 10).
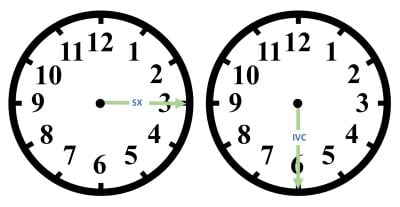
Figure 9: SX at 3 and IVC at 6
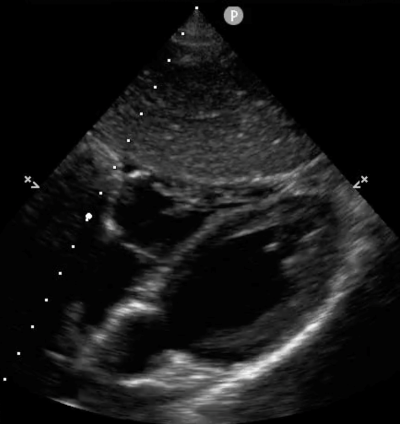
Figure 10: SX ultrasound image
Optimizing the SX view:
- In achieving an optimal SX view that shows all 4 chambers and includes the apex, the probe may need to be rotated mildly clockwise from the 3 o’clock position (5-10 degrees).
IVC
The IVC view is achieved by rotating the probe 90 degrees clockwise from the SX view, so that the probe indicator is oriented toward the feet.
Orient the probe indicator to 6 o’clock (Figure 9) to achieve the IVC view (Figure 11).

Figure 11: IVC ultrasound image
Conclusion
The cardiac clock method of ultrasound teaching can be used to facilitate both teaching and learning. It is currently in use for teaching at the author’s academic institution.
References
- Liu RB, Blaivas M, Moore C, et al. Emergency Ultrasound Standard Reporting Guidelines.; 2018. www.acep.org. Accessed October 28, 2021.
- Prats MI, Bahner DP. Echocardiography for Emergency Physicians. ACEP. https://www.acep.org/sonoguide/basic/cardiac/. Published 2020. Accessed September 20, 2022.
- Dawson M, Mallin M. Ch. 2: Basic Cardiac. In: Introduction to Bedside Ultrasound: Volume 1. Vol 1. ; 2013:25-48.
- Hall MK, Coffey EC, Herbst M, et al. The “5Es” of Emergency Physician-performed Focused Cardiac Ultrasound: A Protocol for Rapid Identification of Effusion, Ejection, Equality, Exit, and Entrance. Acad Emerg Med. 2015;22(5):583-593. doi:10.1111/acem.12652
- Baston CM, Moore C, Krebs EA, Dean AJ, Panebianco N. Chapter 8: Cardiac Ultrasound. In: Pocket Guide to POCUS: Point-of-Care Tips for Point-of-Care Ultrasound. McGraw Hill; 2018. https://accessmedicine-mhmedical-com.ezproxy.bu.edu/content.aspx?bookid=2544§ionid=210344444. Accessed September 20, 2022.
- Taeri RT. Point of Care UltraSound: Cardiac Ultrasound. POCUS BASICS. https://pocusbasics.org/. Published 2021. Accessed September 20, 2022.
- The Intensive Care Network. 4 Basic Cardiac Echo How To-Pre-Reading for FCUS Course. https://intensivecarenetwork.com/lesson/4-basic-cardiac-echo-how-to-pre-reading-for-fcus-course/. Published 2022. Accessed September 20, 2022.