Left ventricular free wall rupture (LVFWR) is a rare and usually fatal complication of myocardial infarction (MI).
Case
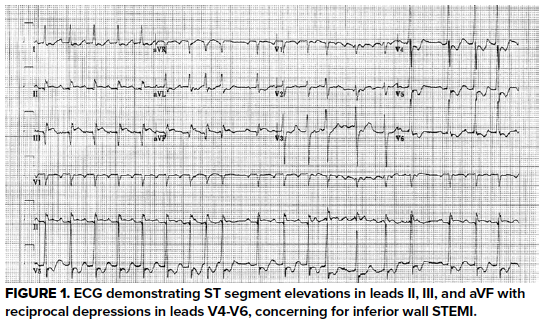
A 54-year-old male presented to the ED by EMS after being found unresponsive with GCS of 3 and irregular respirations. Narcan was given in the field with minimal improvement in the patient’s status. Upon arrival, respirations were assisted by BVM. Vital signs were HR 155, BP 111/75, RR 8, SpO2 100%. The patient was moaning incoherently, exhibiting sporadic movements, and pupils were 3 mm and reactive bilaterally. Naloxone was administered without further effect. While preparations were being made for intubation, an ECG and point-of-care (POC) echocardiogram were performed. Together they raised concern for an inferior wall STEMI with LVFWR evidenced by clotted blood in the pericardial sac and right atrial collapse suggesting cardiac tamponade (Figures 1-5).
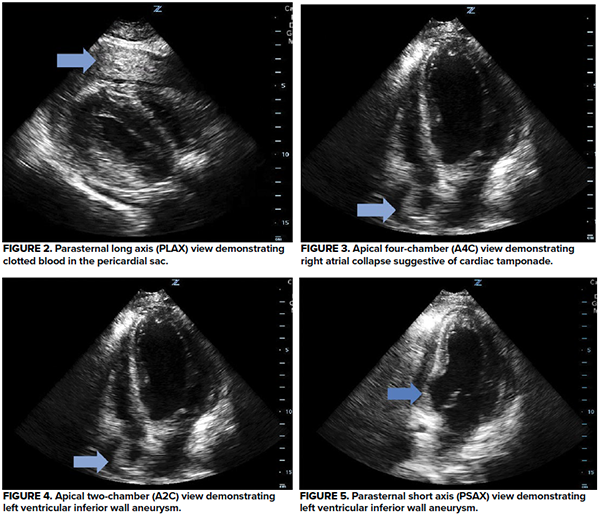
Shortly after making the correct diagnosis with POC echocardiography, the patient became significantly bradycardic. Fluid boluses had already been started. Pericardiocentesis was performed with in-line ultrasound guidance as the patient went into cardiac arrest. Though only 10 mL of blood was aspirated, ROSC was achieved after one round of CPR. The patient was stabilized and sent for CTA. The LVFWR was confirmed as contrast extravasation into the pericardial sac was demonstrated. Cardiology and cardiothoracic surgery were consulted. Unfortunately, the patient expired prior to definitive management.
Discussion
Observational studies estimate that LVFWR complicates between 1% to 4% of acute MIs.1-4 Approximately 70% of patients with LVFWR die within minutes.5 Few cases present subacutely and with enough time for surgical intervention. Survival depends on prompt diagnosis as cardiac tamponade and hemodynamic compromise will often develop within hours.6
The typical signs and symptoms of LVFWR include chest pain, syncope, hypotension, and cardiac arrest.7 Presentation varies and depends on the rate of blood accumulation in the pericardial sac and the development of cardiac tamponade.8
As in this case, EKG can suggest MI as a cause of LVWFR, though the EKG is more often nondiagnostic and does not aid in identifying LVWFR.9 Unfortunately, EKG has not been shown to reliably indicate the presence of pericardial effusion or cardiac tamponade, though low voltage and PR segment depression, and to a lesser extent electrical alternans, can be suggestive.10 Depending on the time since MI, the ECG may exhibit features suggestive of left ventricular aneurysm (LVA). Specifically, persistent and unchanging ST-segment elevations in the presence of prominent Q waves without reciprocal ST-segment depressions are classic for LVA.11,12 Q waves, which were seen in this case, can develop within hours after infarction, but the resolution of reciprocal ST-segment depressions may take up to two weeks.11,13
Fortunately, echocardiography is very sensitive and specific for LVFWR and emergency physicians have demonstrated the ability to diagnose the condition both rapidly and accurately with POC echocardiography.14 In one study of patients with acute MI, the identification of a pericardial effusion >5 mm was nearly 100% sensitive and nearly 93% specific for LVFWR.9 The additional finding of hyperechoic blood clots increased specificity to 98%, and if cardiac tamponade was also present, the specificity was greater than 99%.9 The specific area of wall rupture does not need to be visualized to clinch the diagnosis but can be more easily identified with doppler or contrast echocardiography.15
Once LVFWR is recognized, the patient must be quickly stabilized for definitive management. Isotonic fluid boluses should be administered to improve right heart preload.16 Identification of right atrial collapse during atrial diastole or right ventricular collapse during ventricular diastole should raise concern for cardiac tamponade and impending hemodynamic collapse. Pericardiocentesis is a life-saving procedure that should not be delayed. The procedure is best performed under ultrasound guidance by identifying the largest pocket nearest the body surface and using in-line needle visualization.17 Likely, less than 30 cc of blood will be aspirated due to clotting of the blood.14 Nevertheless, even small volume pericardiocentesis can have profound hemodynamic effects. After stabilization, the definitive management is the repair of the ruptured ventricle by a cardiothoracic surgeon, and operative mortality can be as high as 50%.9
Take-Home Points
- Point-of-care echocardiography is a valuable tool in undifferentiated patients and can be used to identify unexpected complications of acute myocardial infarction such as left ventricular free wall rupture with high sensitivity and specificity.
- ECG is often not helpful in diagnosing pericardial effusion or cardiac tamponade, though low voltage and PR segment depressions, and to a lesser extent electrical alternans, can be suggestive.
- Pericardiocentesis is a life-saving procedure that emergency physicians need to be familiar with.
References
- Becker RC, Gore JM, Lambrew C, Douglas Weaver W, Michael Rubison R, French WJ, Tiefenbrunn AJ, Bowlby LJ, Rogers WJ. A composite view of cardiac rupture in the United States national registry of myocardial infarction. Journal of the American College of Cardiology. 1996; 27(6), 1321-1326. doi:10.1016/0735-1097(96)00008-3
- Nakatsuchi Y., Minamino T., Fujii K., Negoro S. Clinicopathological characterization of cardiac Free wall rupture in patients with acute myocardial infarction: Difference between early and late phase rupture. International Journal of Cardiology. 1994; 47(1), S33-S38. doi:10.1016/0167-5273(94)90324-7
- Pollak H., Nobis H., Mlczoch J. Frequency of left ventricular free wall rupture complicating acute myocardial infarction since the advent of thrombolysis. The American Journal of Cardiology. 1994; 74(2), 184-186. doi:10.1016/0002-9149(94)90098-1
- Yip HK, Wu CJ, Chang HW, Wang CP, Cheng CI, Chua S, Chen MC. Cardiac rupture complicating acute myocardial infarction in the direct percutaneous coronary intervention reperfusion era. Chest. 2003: 124(2), 565-571. doi: 10.1378/chest.124.2.565
- Núñez L, De la Liana R, López Sendón J, Coma I, Aguado MG, Larrea J. Diagnosis and treatment of subacute free wall ventricular rupture after infarction. The Annals of Thoracic Surgery. 1983. 35(5), 525-529. doi:10.1016/s0003-4975(10)60426-2
- Raposo L, Andrade MJ, Ferreira J, Aguiar C, Couto R, Abecasis M, Canada M, Jalles-Tavare N, Da Silva JA. Subacute left ventricle free wall rupture after acute myocardial infarction: Awareness of the clinical signs and early use of echocardiography may be life-saving. Cardiovascular Ultrasound. 2006; 4(1). doi:10.1186/1476-7120-4-46
- Purcaro A, Costantini C, Ciampani N, Mazzanti M, Silenzi C, Gili A, Belardinella R, Astolfi D. Diagnostic criteria and management of subacute ventricular free wall rupture complicating acute myocardial infarction. The American Journal of Cardiology. 1997; 80(4), 397-405. doi:10.1016/s0002-9149(97)00385-8
- Amir O, Smith R, Nishikawa A, Gregoric ID, Smart, FW. Left ventricular free wall rupture in acute myocardial infarction. Texas Heart Institute Journal. 2005; 32(2), 424-426. PMID: 16392235; PMCID: PMC1336725.
- López-Sendón J, González A, López de Sá E, Coma-Canella I, Roldán I, Domínguez F, Maqueda I, Martín Jadraque L. Diagnosis of subacute ventricular wall rupture after acute myocardial infarction: sensitivity and specificity of clinical, hemodynamic and echocardiographic criteria. Journal of the American College of Cardiology. 1992; 19(6):1145-53. doi: 10.1016/0735-1097(92)90315-e.
- Eisenberg MJ, de Romeral LM, Heidenreich PA, Schiller NB, Evans GT Jr. The diagnosis of pericardial effusion and cardiac tamponade by 12-lead ECG. A technology assessment. Chest. 1996; 110(2):318-24. doi: 10.1378/chest.110.2.318.
- Engel J, Brady WJ, Mattu A, Perron AD. Electrocardiographic ST segment elevation: left ventricular aneurysm. American Journal of Emergency Medicine. 2002; 20(3):238-42. doi: 10.1053/ajem.2002.32634.
- Oliva PB, Hammill SC, Edwards WD. Cardiac rupture, a clinically predictable complication of acute myocardial infarction: report of 70 cases with clinicopathologic correlations. Journal of American College of Cardiology. 1993; 22(3):720-6. doi: 10.1016/0735-1097(93)90182-z.
- Ba'albaki HA, Clements SD Jr. Left ventricular aneurysm: a review. Clinical Cardiology. 1989; 12(1):5-13. doi: 10.1002/clc.4960120102.
- Plummer D, Dick C, Ruiz E, Clinton J, Brunette D. Emergency department two-dimensional echocardiography in the diagnosis of nontraumatic cardiac rupture. Annals of Emergency Medicine. 1994; 23(6):1333-42. doi: 10.1016/s0196-0644(94)70361-2.
- Mittle S, Makaryus AN, Mangion J. Role of contrast echocardiography in the assessment of myocardial rupture. Echocardiography. 2003; 20(1):77-81. doi: 10.1046/j.1540-8175.2003.00012.x
- Reardon MJ, Carr CL, Diamond A, Letsou GV, Safi HJ, Espada R, Baldwin JC. Ischemic left ventricular free wall rupture: prediction, diagnosis, and treatment. Annals of Thoracic Surgery. 1997; 64(5):1509-13. doi: 10.1016/S0003-4975(97)00776-5.
- Tsang TS, Freeman WK, Sinak LJ, Seward JB. Echocardiographically guided pericardiocentesis: evolution and state-of-the-art technique. Mayo Clinical Proceedings. 1998; 73(7):647-52. doi: 10.1016/S0025-6196(11)64888-X.



