Seizures account for about 1% of all ED visits for children younger than 18, and at least 5% of pediatric patients will experience a seizure by the time they are 16 years old. Treating the condition in the ED poses myriad challenges.
You are working in the pediatric emergency department (PED) when a 9-month-old girl is rushed into the resuscitation room unresponsive and actively seizing. You perform a brief survey of ABCs and attempt to obtain IV access. Patient suddenly stops seizing, but is otherwise unresponsive. You instruct the nurse to obtain a rectal temperature while you
obtain a point-of-care glucose.1,2
Introduction
Seizures account for about 1% of all ED visits for children < 18 years old, and at least 5% of pediatric patients will have a seizure by the time they are 16 years old.1,2 The highest incidence of new, unprovoked seizures is in those younger than age 1.1
Treating pediatric seizures in the emergency department poses myriad challenges for the ED physician. Parents are frightened and frantic, and those involved in the care of the child may also be anxious. Seizures range from benign to life-threatening, and while some resolve rapidly, others progress to status epilepticus requiring airway and circulatory management.1
Emergency physicians must be able to diagnose and treat life-threatening causes of seizures, avoid unnecessary testing and radiation in those without emergent pathology, and choose medications that appropriately terminate the seizure while reducing potential consequences.1 How can we best approach the seizing child — and with what evidence?
How do you distinguish seizures from seizure mimics?
Taking a proper history is essential to distinguish between true seizures and seizure mimics. Use a stepwise approach to obtain the exact timeline of events. Witnesses should be asked about the onset, duration, nature of movements, and recovery phase. Specifics such as eye movements, tongue biting, urinary incontinence in children who are toilet trained, and presence of aura in children who are able to describe the event are also helpful.
What elements are highly suggestive of true seizures?3
- Lateralized tongue biting (high specificity)
- Flickering eyelids, deviation of gaze
- Dilated pupils with a blank stare
- Lip smacking
- Increased heart rate and blood pressure, desaturations in pulse oximetry during event
What should I look for in my seizing patient?
Compared to unprovoked seizures, which usually occur in structural neurological abnormalities such as hypoxic ischemic encephalopathy, provoked seizures occur in the presence of brain insult (trauma, toxins, fever/ infections, electrolyte disturbances/
metabolic derangements). Regardless of the cause, look for altered level of consciousness, autonomic activity, movement, and behavior.2
Generalized seizures involve both hemispheres, so look for convulsive bilateral motor involvement, but don't be surprised if there are no convulsions present. Partial seizures can be simple (think of a fully alert child with arm twitch) or complex (the child with impairment of consciousness and automatisms +/- aura). Around 30% of patients with partial seizures will progress to generalized seizures.2
When should I worry?
While older guidelines define status epilepticus as any continuous seizure lasting longer than 30 minutes or any intermittent seizures without full recovery/return to baseline status in 30 minutes,1,2 ACEP and other current guidelines define status epilepticus as any seizure lasting 5 minutes or longer, or any repeated seizure activity without regaining consciousness between episodes.3 Mortality and morbidity associated with prolonged seizures are secondary to metabolic derangements and hypoxemia1, so think and act fast!
Mimics — How do you distinguish breath holding spells from seizures?
Breath holding spells can happen to children anywhere from 6 months to 6 years old, but are most common in younger patients. The spells are characterized by a clear trigger that upsets the child, followed by crying, pallor, and a brief syncopal activity secondary to decreased cerebral blood flow. A history of iron deficiency anemia might indicate breath holding spells.
Recovery, however, is rapid and without the post-ictal phase. Seizures typically do not involve these precipitants.3
Mimics — Psychogenic Non-Epileptic Seizures (PNES) vs. true seizures
PNES are epileptic seizure mimics that present with side-to-side head, leg, or arm movements with closed eyes. If the eyes are open, they appear normal rather than deviated. Bicycling movement of the legs is highly suggestive of PNES. Also, PNES are suppressible and activity is reduced with distraction techniques. Usually there is a history of an inciting event (emotional triggers, stress, etc.). These are more common in the adolescent population since the younger pediatric patient cannot feign seizure activity.3
Mimics — Syncope vs. Seizure
Loss of consciousness always precedes perceived seizure activity with syncope. Although some brief twitching episodes may be noted as opposed to a true tonic clonic seizure, recovery is usually rapid.
Did the patient have a fever?
Simple febrile seizures are a unique pediatric entity and are characterized by:
- Temp ≥ 100.4°F or 38°C
- Ages 6 mo – 5 yrs
- Seizure activity < 15 min
- Single seizure in 24 hrs
There is good evidence to show that in an otherwise healthy, well-appearing child, any further work-up of the seizure is unnecessary and management should focus on the underlying febrile illness (UTI, viral syndrome, etc.)4 However, if the child is unvaccinated, shows meningeal signs, or is being treated with antibiotics, an intracranial infection should be considered.4,5-7
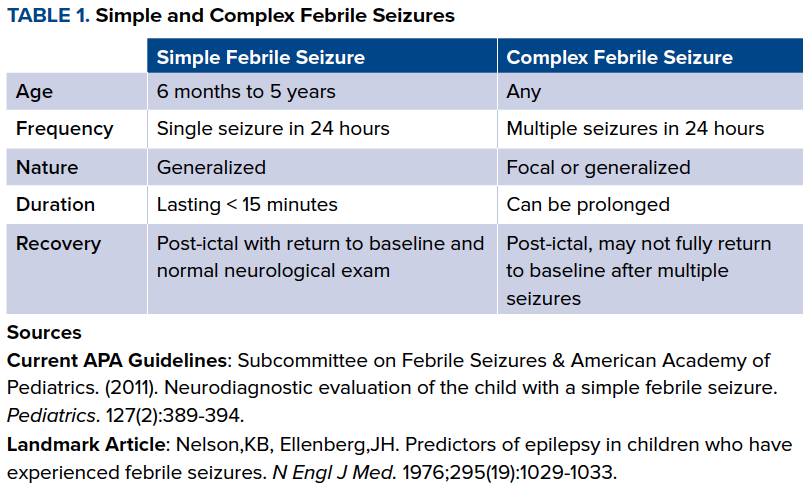
Complex febrile seizures are those that do not meet the previously mentioned criteria and are much more difficult to evaluate. Currently, there are no consensus guidelines for the treatment of these seizures, and inter-physician management varies widely.12 (See Table 1)
Febrile seizures are the most common convulsive events in pediatrics, occurring in 2-5% of children and accounting for the most common cause of provoked seizures.1
Pearl. Simple Febrile Seizures tend to occur early, within 24 hours of fever onset. If seizure occurs > 24 hours after fever onset, suspect a bacterial cause.
When do we LP?
Lumbar punctures (LPs) can be painful and challenging, so be prudent in performing them. Current evidence and AAP guidelines are clear that LPs are not to be routinely performed on healthy, well-appearing children with simple febrile seizures.7 Unfortunately, data regarding the need of LPs in complex febrile seizures, non-febrile/unprovoked seizures, or status epilepticus13-15 is lacking and inconclusive. The general consensus is that LPs should be reserved for patients who are too young or delayed to assess mental status, those with risk factors for or clinical signs/symptoms of meningitis/encephalitis, or those with unexplained
status epilepticus (especially in febrile patients with ongoing seizure activity or altered mental status). In any of these cases, an LP should be performed as soon as possible if the patient is
hemodynamically stable and if clinically feasible. However, if you are unable to obtain LP, antibiotics and/or antivirals should not be delayed and should be started at meningitic doses — NOT bacteremic doses.
Negative LP... no meningitis?
Initial LP may be negative in those who develop meningitis later.2
Does my patient need labs?
Infants < 6 months are at increased risk for hyponatremia from excessive dilution of formula. A temperature < 36.5 C is the best predictor of these hyponatremic seizures. The verdict is still out for those > 6 months. Based on the available data, routine labs are unlikely to change management in patients with recurrent seizures in the absence of a suggestive history, or potentially young age.2
When do I need to get a CT?
Avoid unnecessary radiation. First-time simple febrile seizures do not warrant a head CT, and clinical judgement should guide the need to CT a child with a complex febrile seizure.
First-time, non-febrile, unprovoked seizures generally do not need scanning. The Sharma study guides recommendations for obtaining a head CT in this group and is reserved for those who are high-risk: focal seizure in those < 33 months and those with predisposing condition such as focal or persistent seizure, ventriculoperitoneal shunts, focal neurological deficits, travel to region endemic for cysticercosis, HIV, sickle cell, malignancy, vomiting, altered mental status, and closed head injury associated with LOC are among other high-risk patients.2
PEARL. What appears as a first-time seizure may not actually be a patient's first seizure. Diagnosis of epilepsy is made after 2 unprovoked seizures or 1 unprovoked with an abnormal EEG.2
Intubation
Airway is a priority in the seizing patient. There is poor evidence about when to intubate a patient with status epilepticus, but if your first- and secondline seizure abortive therapies fail, and you consider using barbiturates or propofol, think about intubating16,17 in addition to assessing the patient's clinical status (O2 sat and ability to protect airway).
Anticonvulsants
Next, stop the seizure. The first line is benzodiazepines, with lorazepam having the highest potency. Benzodiazepines are best administered intravenously but can also be given intraosseously, intranasally (lorazepam and midazolam), intramuscularly (midazolam) and rectally (diazepam)17 if IV access is difficult to obtain in pediatric patients. If seizing continues, try one more dose of benzodiazepines. Then turn to hydantoins (phenytoin and
fosphenytoin). IV fosphenytoin is preferred given that fosphenytoin is the water-soluble pro-drug of phenytoin and can be infused faster intravenously with less tissue irritation and fewer
cardiovascular effects such as a drop in blood pressure.18
![]()
Is the patient still seizing?
Next options would be phenobarbital (20 mg/kg), valproic acid (20-40 mg/kg), or levetiracetam (20-60 mg/kg).24 Phenobarbital is most commonly used in the developed world, although this has been declining because of its cognitive and behavioral adverse effects. It can
also cause sedation, hypotension, and respiratory depression necessitating intubation, especially if you start a continuous infusion.19
Special Considerations
Consider non-accidental trauma in infants and pregnancy in adolescent females. Patients with a known seizure disorder should also have their medications reviewed for any recent changes and have drug levels in blood checked if applicable.
PEARL. Don't forget that older teenagers may drive. Some states have mandated reporting laws. It is important to know whether your state is one of them and for what period they need to be seizurefree before driving again.
Pyridoxine and When To Use It
Pyridoxine-dependent seizures are a diagnosis unique to pediatric patients. Administer pyridoxine (100 mg IV) to infants with seizures unresponsive to conventional anticonvulsants (defined as unresponsive to first and second line antiseizure medications). 24
If an accidental ingestion or suicide attempt is suspected, ask parents about the availability of isoniazid in the house, as overdose is a possible cause of seizures resistant to conventional anticonvulsants. Pyridoxine administration is the antidote; recommended dosing is 1 g for every gram of isoniazid ingested (common pediatric dosage is 70 mg/kg).24
Disposition
ACEP policy states that adult patients with normal neurologic exam can be safely discharged with outpatient followup.26 While it's reasonable to extend this to children who have brief unprovoked seizures, those < 1 year old should be admitted, as they are more likely to have recurrent seizures. All patients with first-time non-febrile seizure should have an outpatient EEG. Patients with status epilepticus should be admitted for observation.2
Patients can be discharged after simple febrile seizures unless admission is needed for management of the infection.2 Complex febrile seizures are more likely to recur, especially if
prolonged or associated with focality, so these patients should, at the minimum, be observed for longer periods of time based on the underlying pathology, if any.24
Patients with known seizure disorder can be considered for discharge if they have reliable caregivers. These patients should avoid swimming and being in a bathtub unsupervised.2
PEARL. One unprovoked seizure doesn't equal seizure disorder. One pediatric prospective study of 407 patients demonstrated that 5-year recurrence rate was only about 42%.25
CUTTING EDGE
Cannabinoids for pediatric epilepsy: Up in smoke or real science?
Despite current enthusiasm for the use of "medical marijuana" in treating epilepsy, specifically CBD (cannabidiol) among parents of children with intractable epilepsy,26-28 the evidence is inconclusive at best. 28
Case Conclusion
Since hypoglycemia is a reversible cause of status epilepticus, POC glucose was obtained and was 120. Patient was febrile to 40 C. Patient stopped seizing but remained in a postictal state that lasted for 15 minutes. Rectal acetaminophen was given. During this time, she remained hemodynamically stable with an oxygen saturation of 100%. A urinalysis was obtained because the patient is a young female, and it was positive for a urinary tract infection. Mom endorsed patient was back to baseline and smiling. Patient was observed in the ED and discharged home with antibiotics.
References
1. Santillanes G, Luq Q. Emergency Department Management of Seizures in Pediatric Patients. EB Medicine. 2015;12(3):1-28.
2. Berg CD, Schumann H. An Evidence- Based Approach to Pediatric Seizures in the Emergency Department. EB Medicine. 2009;6(2):1-26.
3. Kimia A, Ben-Joseph EP, Rudlow T, et al. Yield of lumbar puncture among children presenting with their first complex febrile seizure. Pediatrics. 2010;126(1):62-69.
4. Subcommittee on Febrile Seizures, American Academy of Pediatrics. Neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics. 2011;127(2):389-394.
5. Peltola H, Kilpi T, Anttila M. Rapid disappearance of Haemophilus influenzae type b meningitis after routine childhood immunisation with conjugate vaccines. Lancet. 1992;340(8819):592-4.
6. Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348(18):1737-1746.
7. Kyaw MH, Lynfield R, Schaffner W, et al. Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae. N Engl J Med. 2006;354(14):1455- 1463.
8. Lowenstein DH, Bleck T, Macdonald RL. It’s time to revise the definition of status epilepticus. Epilepsia. 1999;40(1):120- 122.
9. Guidelines for epidemiologic studies in epilepsy. Commission on Epidemiology and Prognosis, International League Against Epilepsy. Epilepsia. 1993;34(4):592-596.
10. Shinnar S, Berg AT, Moshe SL, Shinnar R. How long do new-onset seizures in children last? Ann Neurol. 2001;49(5):659-664.
11. Subcommittee on Febrile Seizures, American Academy of Pediatrics. Neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics. 2011;127(2):389-394.
12. Carreno M. Recognition of nonepileptic events. Semin Neurol. 2008;28(3):297-304.
13. Sales JW, Bulloch B, Hostetler MA. Practice variability in the management of complex febrile seizures by pediatric emergency physicians and follows. CJEM. 2011;13(3):145-149.
14. Riviello JJ Jr, Ashwal S, Hirtz D, et al. Practice parameter: diagnostic assessment of the child with status epilepticus (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2006;67(9):1542-1550.
15. Chin R, Neville B, Peckham C, et al. Incidence, cause, and short-term outcome of convulsive status epilepticus in childhood: prospective population based study. Lancet. 2006;368(9531):222-229.
16.* Singh RK, Stephens SM, Berl M, et al. Prospective study of new onset seizures presenting as status epilepticus in childhood. Neurology. 2010;74(8):636-642.
17. Treatment of convulsive status epilepticus. Recommendations of the Epilepsy Foundation of America’s Working Group on Status Epilepticus. JAMA. 1993;270(7):854-859.
18. Appleton R, Choonara I, Martland T, et al. The treatment of convulsive status epilepticus in children. The Status Epilepticus Working Party, Members of the Status Epilepticus Working Party. Arch Dis Child. 2000;83(5):415-419.
19. Fischer JH, Patel TV, Fischer PA. Fosphenytoin: clinical pharmacokinetics and comparative advantages in the acute treatment of seizures. Clin Pharmacokinet. 2003;42(1):33-58.
20. Brodie MJ, Kwan P. Current position of phenobarbital in epilepsy and its future. Epilepsia. 2012;53
21. Medical Services Commission. Febrile seizures. Victoria (BC): British Columbia Medical Services Commission. 2010 Sept 1. Accessed September 25, 2014.
22. Capovilla G, Mastrangelo M, Romeo A, et al. Recommendations for the management of “febrile seizures”: ad hoc task force of LICE Guidelines Commission. Epilepsia. 2009;50(Suppl 1):2-6.
23. Warden CR, Zibulewsky J, Mace S, et al. Evaluation and management of febrile seizures in the out-of-hospital and emergency department settings. Ann Emerg Med. 2003;41(2):215-222.
24. Oluwabusi T, Sood SK. Update on the management of simple febrile seizures: emphasis on minimal intervention. Curr Opin Pediatr. 2012;24(2):259-265.
25. Wilfong A, Nordli DR Jr, Dashe JF. Management of Convulsive Status Epilepticus in Children. UpToDate. 2018.
26. Shinnar S, Berg AT, Moshe SL, et al. The risk of seizure recurrence after a first unprovoked afebrile seizure in childhood:an extended follow-up. Pediatrics. 1996;98(2 Pt 1):216-225.
27. Maa E, Figi P. The case for medical marijuana in epilepsy. Epilepsia. 2014;55:783-6.
28. Welty TE, Luebke A, Gidal BE. Cannabidiol: promise and pitfalls. Epilepsy Curr. 2014;14:250-2.
29. Bostwick JM. Blurred boundaries: the therapeutics and politics of medical marijuana. Mayo Clin Proc. 2012;87:172-86.



