This original research, funded through an EMRA Simulation Grant, offers insight on training in procedural sedation with emphasis on patient safety, especially in the pediatric population.
In EDs where pediatric volume is low, pediatric sedation is a low-frequency, high-consequence procedure, in which the nature of the medications and procedure are all the risks of airway management and medication reactions. In 2006, a large multicenter retrospective review on pediatric sedations demonstrated that significant complications such as development of stridor, laryngospasm, wheezing, or apnea occurred in 1 out of 400 pediatric sedation cases, with 1 out 200 sedations requiring immediate airway management such as bag valve mask, oral airway, or intubation.1 The probability of adverse reactions increases significantly with an upper respiratory tract infection, which are ubiquitous in pediatric patients.2,3 Advances in airway management, namely end tidal CO2, have been shown to improve detection of apnea and hypoxic events prior to oxygen desaturation. This allows for quick airway management, including physical stimulation, airway manipulation, nasal or oral airway, oxygen supplementation, and positive pressure ventilation for the mitigation of life threatening situations.4,5 For the inexperienced operator, failure to recognize these impending complications allows for degeneration into life-threatening situations if not managed appropriately. Safety checklists and procedural skills are imperative to ensure operator competency and patient safety. In this grant-funded study, the investigators created a multi-phase module at an academic 3-year EM residency program to train all active EM residents in procedural sedation with emphasis on patient safety, especially in the pediatric population.
Methods
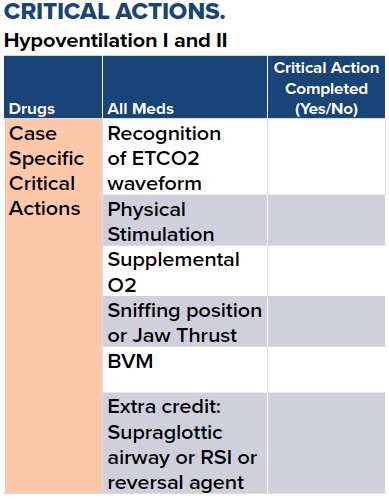
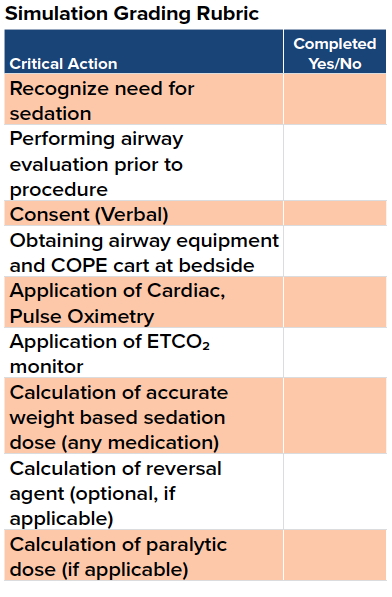
All EM residents at Thomas Jefferson University, excluding the principal investigator, were asked to participate in the study with N=36 (out of 38) enrolled. The participants first completed a pre-test on medical knowledge of sedation protocol, and were then assigned to 4 separate groups (2 control, 2 experimental) for regularly scheduled pediatric sedation didactics at the institutional simulation center. Each group underwent a structured simulation exercise in the simulation center with emphasis on sedation techniques, medical management, and technical skills using a Sim Man 3G model, with each session concluding with a preceptor-led review of relevant rescue airway management techniques and medication reactions. The control groups experienced the simulation without the aid of a developed procedural checklist; the intervention groups were given the procedural checklist to guide procedure flow. At the end of the course, all participants were tasked to perform a simulated pediatric procedural sedation graded based on achieving specific critical actions and a post-simulation written test on sedation protocol.
Results
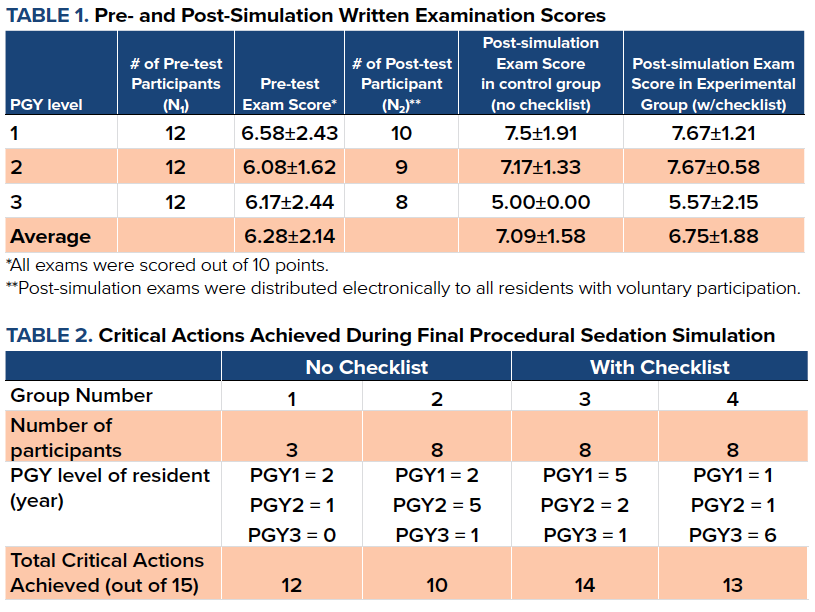
Residents scored together an average of 70% on the pre-test. The most commonly missed questions involved pediatric endotracheal tube size, depth of insertion for intubation, and performing Larson’s maneuver (18/36 correct). Recognition of hypopnea on an end tidal CO2 tracing was marked correct by a majority of learners (32/36). Comparison between pre- and post-didactic tests demonstrated higher scores for residents across all PGY levels with PGY-2 residents experiencing the highest increase in their exam score when provided with a checklist. The most frequently missed question included evaluation of Mallampati (6/11 control, 8/16 experiment); however the learners improved on recognizing appropriate pediatric endotracheal tube and depth of insertion. Residents in the experimental group achieved at least 3 more critical actions than the lowest scoring control group. The most frequently missed critical action in both control and intervention groups was termination of the procedure once respiratory distress was detected.
Discussion
The experimental groups who received a checklist in addition to standardized procedural sedation didactic obtained several more critical actions than the control group. While both groups demonstrated improvement in post-didactic test scores, the largest increase in exam scores was noted from the checklist group.
There are numerous limitations to this study. The sample is small; more study is needed to elucidate if this improvement in critical actions is sustained in simulation samples. The groups were also not randomized due to scheduling conflict; however, a majority of the junior learners present (PGY1 and PGY2) were coincidentally distributed in roughly even numbers across control and intervention groups. Of note, the authors did not notice a correlation between group seniority and achieving higher examination scores or more critical action items. Interestingly, the group with majority PGY1 residents scored the highest number of critical actions out of all groups with the checklist. The cause of this unique finding may be multifactorial. The study occurred during the second half of the academic year, in which senior residents may not have been as enthusiastic as their junior counterpart. This was reflected with sample survey responses from senior residents consistently selecting the same answer choice to all questions.
Conclusion
Pediatric sedation is a low frequency procedure for many adult EDs, therefore requiring frequent review of rescue techniques and medication considerations. This study is preliminary data demonstrating that a safety checklist may reinforce safe pre-procedural techniques and setup and allow for review of critical actions in crisis. Future studies should attempt to evaluate longitudinal improvement in resident performance after repeated trainings with the checklist.
In addition, this training program has great potential to be developed as an in situ, just-in-time-training module for pediatric procedural sedation, to take place in the clinical environment, just prior to application.
Disclosures
Human subjects: This study was exempt from IRB review according to the Thomas Jefferson University IRB criteria for research subjects involved in normal educational practices. As part of the didactic curriculum, all human residents gave implied consent for participation in an educational activity. Animal subjects: All authors have confirmed this study did not involve animal subjects or tissue. Conflicts of interest: According to the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: EMRA provided a scholarship of $500 for the development of this project and purchase of materials relevant to the completion of the study. Financial relationships: All authors have declared no financial relationships at present or within the previous 3 years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
1. Cravero JP, Blike GT, Beach Ml, Gallagher SM, Hertzog JH, Havidich JE, Gelman B. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: Report from the pediatric sedation research consortium.(anesthesia for pediatrics). Pediatrics. 2006;18(3):1087-1096.
2. Mallory MD, Travers C, McCracken C, Hertzog J, Cravero JP. Upper Respiratory Infections and Airway Adverse Events in Pediatric Procedural Sedation. Pediatrics. 2017;140(1):e20170009.
3. Al-alami AA, Zestos MM, Baraka AS. Pediatric laryngospasm: Prevention and treatment. Curr Opin Anaesthesiol. 2009; 22(3):388-395.
4. Burton JH, Harrah JD, Germann CA, Dillon DC. Does end-tidal carbon dioxide monitoring detect respiratory events prior to current sedation monitoring practices? Acad Emerg Med. 2006;13(5):500-504.
5. Deitch K, Miner J, Chudnofsky CR, Dominici P, Latta D. Does end tidal CO2 monitoring during emergency department procedural sedation and analgesia with propofol decrease the incidence of hypoxic events? A randomized, controlled trial. Ann Emerg Med. 2010;55(3):258-264.
6. Emergency Medicine Milestone Project. Accreditation Council for Graduate Medical Education and American Board of Emergency Medicine. https://www.acgme.org/Portals/0/PDFs/Milestones/EmergencyMedicineMilestones.pdf. Published July 2015. Accessed December 2017.



