The pediatric ECG has numerous subtle and not-so-subtle differences when compared to the average adult ECG. Detecting these differences can focus your differential, impact your treatment, and most importantly provide you with solid footing in making a relevant consultation to pediatric cardiology.
This review will focus on the key differences in rate, axis, and intervals.
Rate
The foremost difference is rate. Unlike adults, children not only tolerate a much higher heart rate but depend on an increase in heart rate alone to increase cardiac output. The resting heart rate does not coincide with adult range until at least age 5 years.
Children can also have wider variation in heart rate associated with the respiratory cycle and changes in P-P interval. This phenomenon is termed sinus arrhythmia. Up to 50% of infants can have sudden prolongation of the P-P interval with no symptomatic or long-term effects.4
Axis
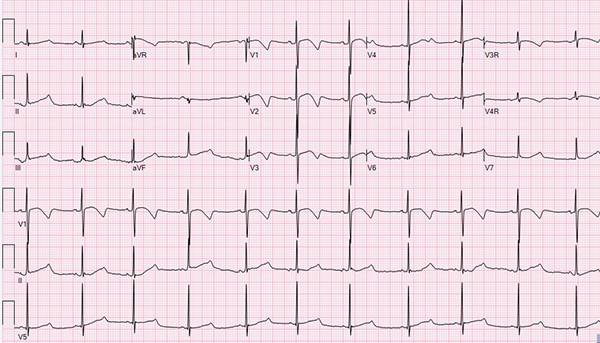
At birth, all neonates have a rightward axis because of relative right ventricular hypertrophy. Most pronounced at 1-2 months of age, the axis slowly migrates from right to left as the left ventricular myocardium hypertrophies to account for the postnatal increase in systemic vascular resistance and a concomitant decrease in pulmonary vasculature pressures. The normal adult ratio of right-to-left ventricle mass — and thus a normal axis — is expected to be seen by age 6 months. A persistent rightward axis can be indicative of congenital heart disease. Similarly, as the left ventricle grows during the first years of life, a decrease in the amplitude of the R waves and corresponding increase in the amplitude of S waves is seen in the right precordial leads.1,2,3
Precordial T Waves
A pediatric norm that can initially seem alarming to an adult practitioner is the “juvenile T-wave pattern.” The precordial leads have T-wave inversions that normally persists until age 10-12 years. Occasionally, this pattern can last later into adolescence and young adulthood. Presence of a positive T wave in V1-V3 past the first week of life is pathologic and warrants further investigation.2 The T waves in V5 and V6 should always be positive after the first 3 days of life.1
Q Waves
Young children can have a significant Q wave in the inferior and lateral leads from birth until age 3-5 years, when they recede. They can be as deep as 8 mm in lead III during childhood. These Q waves are expected, so much so that their absence in the lateral leads can be an indication of congenital heart disease. Other characteristics that would raise concern would be right precordial Q waves, wide Q waves, abnormally deep Q waves.1,3
Intervals
Children have shortened PR intervals and QRS complexes compared with adults. This is often overlooked because most of us have committed normal adult wavelength ranges to memory. It is important to remember that what may be a normal PR interval in an adult can be a manifestation of 1st degree block in a young child.
Additionally, a normal adult QRS could be a bundle branch block in a young child. The PR interval initially shortens in the first year of life before gradually widening to the adult range through childhood.2 Both P wave and QRS slowly widen to adult ranges as the child ages. Age-based charts are available and should be referenced when determining appropriate PR interval and QRS complex duration.
Of note, healthy teenagers can have significant abnormalities on ECG that are normal variants. Bradycardia at rest is often seen in young, healthy and mostly athletic teenagers. Additionally, these adolescents can have a prolonged PR interval at rest — some to the extent they have ongoing 1st degree block while sleeping. Around 10% can develop transient, asymptomatic Mobitz Type I 2nd degree AV block at rest. This percentage was shown to be higher when a group of teenagers in intensive physical training were analyzed.5,6
Long QT
Identification of differences in the pediatric and adult ECG aid in distinguishing potentially life-threatening abnormalities from a normal ECG, with one of the most notable and vastly overlooked conditions being prolonged QT interval.
Prolonged QT is perceived as a clinical specter that is transiently considered on an academic
basis when we approach a patient with syncope or order one of the many medications that can
elongate the interval. While seemingly rare, it is an important clinical consideration given the
correct circumstances and should not be overlooked in the emergency department.8 What makes assessment for prolonged QT especially important in children is symptoms may not manifest until they progress to life-threatening dysrhythmia, torsades de pointes, or sudden cardiac death.7
The identification of prolonged QT syndrome requires an index of suspicion enough to warrant a workup with ECG. Often symptomatic patients will present with syncope or presyncope manifesting as dizziness or lightheadedness. A small percentage of patients will present with seizure activity. In many cases, exercise, emotional stress, swimming/diving, and startle responses elicit these symptoms.
Prolonged QT is identified via ECG. A good way to screen for a prolonged QT is to draw a line in the middle of an R-R interval. If the T wave occurs after the dividing line or that line bisects part of the T wave, investigate the QT interval further. The most reliable measurement is the QTc or the corrected QT interval, which reflects the QT interval corrected for heart rate. Normal range for the QTc is generally accepted as < 0.44 sec or 440 msec. QTc from 0.44-0.46 sec is considered borderline and only significant if symptomatic. Anything greater than 0.46 sec is prolonged QT.
Most ECG machines provide a QTc on the computer interpretation. The machines use the default Bazett formula, which is useful when the heart rate is within the normal adult range but is inaccurate when the rate is < 60 or >100. There are several other formulas that are more accurate for calculating QTc for heart rates outside of normal adult range (eg, Fredericia, Framingham, Hodges). The ECG computer tends to overestimate the QTc, especially if the heart rate is outside the normal range. When you receive an ECG that lists the QTc as borderline or prolonged, the first step should be to look at the heart rate and calculate the QTc manually using a formula that accounts for heart rate < 60 or >100 if applicable. The computer-generated QT and RR measurement has been found to be consistently accurate in most ECG computers and thus can be used to manually calculate the QTc.9
Prolonged QT interval can be caused by numerous factors. The most concerning in an otherwise healthy child is congenital Long QT syndrome. Family history is one of the most important aspects of the patient’s history because inherited conduction abnormalities are the leading causes of persistently prolonged QT interval.7 There are numerous inherited mutations that fall under the classification of Long QT syndrome; luckily, they tend to present similarly and treatment is often uniform. Other causes include electrolyte abnormalities (hypocalcemia, hypomagnesemia, hypokalemia), hypothermia, increased ICP, and medications. While these other causes typically have additional findings on exam and ECG, familial Long QT syndromes and medications often manifest as prolonged QT alone.
Symptomatic prolonged QT syndrome may require emergent cardiology assessment and intervention depending on degree of prolonged QT. In severe cases, rate control either by medication or pacing can be initiated in the emergency department. Prolonged QT with mild or no symptoms requires a more extensive outpatient workup by a cardiologist, but identification in the ED can be life-saving. These patients should be counseled to avoid certain medications and strenuous activity until they can be evaluated by a cardiologist; this includes exemption for sports (especially swimming or diving) and PE in school. The extended workup includes serial ECGs, stress testing, and potential genetic testing for familial long QT.
Conclusion
Being familiar with measuring the QT interval and identifying a prolonged QT is important for the ED provider because outcomes are good if long QT is detected early. These patients can lead normal lives with appropriate treatment, which may include pharmacologic rate control, AICD placement, or operative sympathetic ganglionectomy.
Acknowledgments
Special thanks to Dr. Bianca Castellanos and Dr. Kelly Gajewski from the LSUHSC Department of Pediatric Cardiology for their contributions.
References
1. Dickinson DF. The Normal ECG in Childhood and Adolescence. Heart. 2005. 91(12):1626-1630.
2. Goodacre S, McLeod K. ABC of paediatric electrocardiography. BMJ. 324(7350):1382-1385.
3. Burns E. Paediatric ECG Interpretation. Life in the Fast Lane. April 2017.
4. Southall DP, Richards J, Mitchell P, Brown DJ, Johnston PG, Shinebourne EA. Study of cardiac rhythm in healthy newborn infants. Br Heart J. 1980;43(1):14-20.
5. Vitasalo MT, Kala R, Eisalo A. Ambulatory electrocardiographic findings in young athletes between 14 and 16 years of age. Eur Heart J. 1984;5(1):2-6.
6. Dickinson DF, Scott O. Ambulatory electrocardiographic monitoring in 100 healthy teenage boys. Br Heart J. 1984;51(2):179-183.
7. Ackerman MJ. Consultation with the Specialist: The Long QT Syndrome. Ped Rev. 1998;19(7).
8. Van Dorn CS, Johnson JN, Taggart NW, Thorkelson L, Ackerman MJ. QTc Values Among Children and Adolescents Presenting to the Emergency Department. Pediatrics. 2011;128(6):e1395-e1401.
9. Charbit B, Samain E, Merckx P, Funck-Brentano C. QT Interval Measurement: Evaluation of Automatic QTc Measurement and New Simple Method to Calculate and Interpret Corrected QT Interval. Anesthesiology. 2006;104(2):255-260.