Case.
An otherwise healthy 35-year-old male presents with 1 week of intermittent palpitations associated with substernal chest discomfort and dyspnea.
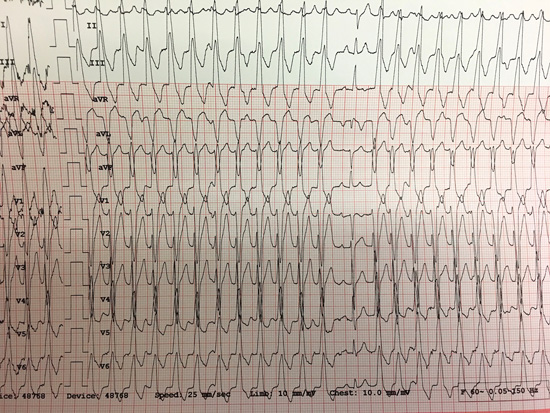
What is your interpretation of the following 12-lead ECG rhythm strip?
ANSWER
The ECG shows a regular wide complex tachycardia with a ventricular rate of ~165 bpm and left axis deviation. The important question is whether this is VT or SVT with aberrant conduction. Although there is a LBBB pattern (which supports the likelihood of SVT with aberrant conduction), there are 2 findings with high specificity for VT:
- AV dissociation (there are intermittent identifiable P-waves with no consistent relationship with the QRS complexes).
- The 13th beat is a capture beat.
Differentiating VT from SVT with aberrant conduction can be challenging. There are multiple algorithms for VT that have good specificity, but none of them have great sensitivity for VT. This EKG has multiple findings supporting VT, but in the absence of any features supporting VT, it is best to assume VT as erroneously treating VT as SVT with aberrant conduction could be clinically disastrous. It is important to note that response to treatment with nodal blockers does not rule out VT. “Idiopathic VT,” a general term for various forms of VT in structurally normal hearts, often looks like SVT with aberrant conduction and responds to nodal blockers. It is also important to note that the findings specific for VT are not sensitive for VT, and the absence of these findings isn’t specific for SVT with aberrant conduction.
LEARNING POINTS
Regular WCT
- Ventricular rate >100 bpm, QRS >120 ms, and constant RR interval
- DDx includes:
- Monomorphic ventricular tachycardia
- SVT with aberrant conduction
- Antidromic SVT (WPW)
- Any SVT (sinus tach, AVNRT, atrial flutter, etc.) with fixed or rate-related BBB
- Any SVT with metabolic abnormalities
- Any SVT with sodium channel blocking toxicity
Monomorphic VT
- ≥3 consecutive, regular, wide complex beats with rate >100
- Non-sustained: <30 sec duration with no hemodynamic instability
- Sustained: ≥ 30 sec duration OR causes hemodynamic instability
SVT with aberrant conduction
- Aberrant conduction can be due to BBB (rate related or pre-existing), bundle dysfunction (metabolic or toxicologic), or accessory pathway
- Baseline QRS morphology due to pre-existing BBB can change in the setting of tachycardia
EKG Features that increase likelihood of VT in WCT
- QRS >200 ms is almost always VT or hyperkalemia with aberrancy
- AV dissociation (note that AV association isn’t specific for SVT as VT can have 1:1 retrograde conduction)
- Positive or negative QRS concordance in leads V1-V6 (entirely or predominantly positive or negative QRS complexes from V1 to V6)
- Extreme axis deviation (“northwest axis”)
- If BBB pattern is present, the absence of typical RBBB or LBBB pattern suggests VT (i.e., normal RBBB or LBBB pattern makes SVT with aberrant conduction more likely)
- Fusion beats- hybrid QRS complex formed by both supraventricular and ventricular focus
- Capture beats- sinus QRS formed by transient normal conduction amid AV dissociation
- Brugada’s sign- time from the onset of the QRS complex to the nadir of the S-wave is >100 ms
- Josephson’s sign- notching near the nadir of the S-wave
Algorithms for VT
- Includes Wellens, Kindwall, Brugada, Verekei (aVR), Becker & Crijns
- No algorithm is diagnostically superior
- Assume VT if uncertain



