Although cervical spine injuries are rare among the pediatric population, when you do see a child with a spinal injury, there's a 60-80% likelihood the c-spine is involved.
Case Presentation
Case 1: A 6-year-old girl is brought in via EMS to your level 1 Trauma as a bicycle vs. car. It is approximated the car was traveling approximately 25 mph. During your initial examination: the patient is crying, equal and bilateral breath sounds, tachypneic and tachycardic with a GCS of 15. She is in a cervical collar and after exposing her you appreciate left shoulder, back, and left leg abrasions. Upon log-roll, it is difficult to appreciate if the patient is having any cervical/thoracic or lumbar spine tenderness as she is intermittently crying, but no step offs are appreciated. What would be your next step? Would you image her C-spine? If so, what type of imaging would you get? Can you apply the same clinical tools for cervical spine injury imaging in adults to pediatric patients?
Case 2: A 2-year-old boy is brought in by mom after her car was rear-ended by another car going 30 mph while she was parked and breastfeeding him in the back seat. Mom states the patient has not wanted to move his neck and has been breathing “funny”. Prior to the exam, the child was placed in a C-collar due to high suspicion of C-spine injury (CSI). During the exam, the patient does not speak to you, has irregular breathing, tachycardic, avoiding moving his neck, and has minimal movement of his extremities. The patient was immediately intubated. What is your next step? Do you go straight to CT or MRI as you are worried about a CSI?
Background
Cervical spine injuries (CSIs) are fortunately very rare in the pediatric population. Of all pediatric patients admitted for blunt injuries, only 1.3% are diagnosed with a CSI.1 However, when examining pediatric spinal injuries overall, CSIs account for the majority, occurring in 60-80%.2
Mechanisms of Injury
The most common mechanisms of injury include motor vehicle collisions (MVC), falls, diving accidents, acceleration-deceleration forces, or a clotheslining force.3 Depending on the patient’s age group, certain mechanisms of injuries are noted to be more common than in others. MVC and falls are most common in children less than 2 years old; MVC, falls, and pedestrians struck by motor vehicle in children 2 to 7 years old; and sports injuries and MVC in children 8 to 15 years old.4 In a cohort of 540 children with CSIs, 1% had injuries due to assault, of which half were attributed to child abuse.4 Although non-accidental trauma appears to be a rare cause of CSIs, clinicians must be vigilant in their assessment of a patient, looking for other locations of questionable injuries and reporting any suspicions that a CSI was non-accidental.
Common Sites of Injury
The probable location of a CSI can vary among age groups. Injuries to the axial region (C1-C3) were seen in 74% of CSIs in children less than 2 years old and 78% of CSIs in children 2 to 7 years old.4 In children 8 to 15 years old, however, subaxial injuries were more prevalent, accounting for 53% of CSIs.4 In the same cohort of 540 children mentioned previously, only 1% had dislocations at more than one cervical level and 3% had fractures of more than one cervical vertebra.4
Anatomy and Physiology of Pediatric Patients with Suspected CSI
Children's anatomic development increases their susceptibility to CSI. Compared to adults, children have larger heads relative to their bodies, their spinal column is more elastic, and their cervical spine muscles are weaker.5 Further, there is greater ligamentous laxity in their spine.5 In addition, the atlas (C1) and axis (C2) have ossification centers that do not complete fusion until up to 7 years of age.5 This may explain why children are 2.5x more likely to sustain atlantoaxial injuries than adults.5 This not only places children at increased risk for CSI, but also can make interpreting imaging more difficult for clinicians. Ossification centers can appear widely different between patients, leaving room for the possibility of misdiagnosing fusion lines as vertebral fractures.5 Despite all these inherent risk factors, the incidence of CSIs is still low in children. However, there should be increased suspicion of CSI in multisystem trauma and patients with a head injury.
Work-Up
One should first immobilize the neck based on suspicion of CSI and then follow the guidelines established by the Advanced Trauma Life Support beginning with the primary assessment and management (ie, ABCDEs). Once the patient has been stabilized during the primary evaluation, then the secondary exam involving palpation of the neck and cervical spine, focused neurologic examination, and history-taking can occur. This process may be challenging with younger patients or those who are unable to fully provide a history and cooperate with the examination. For these patients, it’s prudent to understand the mechanism of injury to determine whether a CSI may be present and utilize this information for further management.
Examination
In patients with suspected CSIs, the examination should focus on vital signs, neck examination, and neurologic evaluation. Upper CSIs may result in patients with arrested respiration, hypotension, or altered mental status, and injuries to C3-C5 may result in apnea or hypoventilation due to loss of diaphragmatic control.6 Upon neck examination, CSIs present more commonly as midline cervical tenderness, though a triad of neck symptoms including cervical pain, muscle spasm, and decreased range of motion should prompt suspicion for a CSI.7 If there is midline tenderness to palpation, ROM testing should be deferred, and the patient should be re-immobilized in a C-collar. In combination with the initial assignment of the Glasgow Coma Scale score, the neurologic examination must evaluate the patient’s tone, strength, sensation, and reflexes, since approximately 53% of children with cervical cord injuries have neurologic deficits.8 However, pediatric patients who are asymptomatic or are able to walk should not have a CSI ruled out if the mechanism of injury suggests the possibility of one. Among children with diagnosed CSIs, a study found that 18% were asymptomatic at presentation although their mechanism of injury was high-risk.7 Patients with a concerning history or any of these presentations on the exam require continued cervical spine immobilization and further evaluation.
Clinical Tools
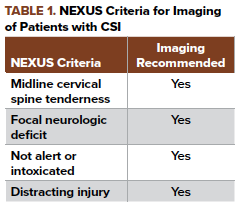
Unfortunately, clinical decision tools such as the Canadian C-Spine Rule and the Nexus criteria have not been well validated in the pediatric population. The Canadian C-Spine study has not been validated for pediatric patients since it did not include patients under the age of 16.9 In contrast, the NEXUS (Table 1) study contained 3,065 patients under the age of 18 years. However, only 30 of these patients were found to have CSIs. Almost all of the injured patients were older patients, with just four patients being under the age of 9 and no patients under the age of 2.10 One study demonstrated that the NEXUS criteria has a 100% sensitivity and a 19.9% specificity for diagnosing cranial spine injuries in pediatric patients aged 9-17 years old.11 Despite this study, the NEXUS criteria should only be used as an aid to the overall clinical gestalt as it has yet to be validated as a tool in pediatric trauma.
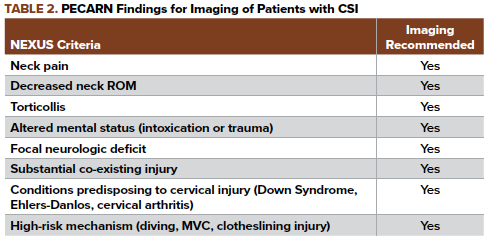
Another study conducted in the Pediatric Emergency Care Applied Research Network (PECARN) compared pediatric patients from the ages of 0 to 15 years with CSIs to control patients. The study determined that there were 8 findings, as illustrated in Table 2, that could be used to recommend imaging and detect CSIs. The findings listed in the study had a 98% sensitivity and 26% specificity.6 Unfortunately, these risk factors have yet to be fully validated. Therefore, we are currently limited to only using the NEXUS criteria and PECARN findings as clinical assessment guides along with our clinical gestalt in deciding C-spine imaging.
Imaging
Once the patient warrants further evaluation to rule out a CSI, an imaging modality must be chosen. With increasing awareness of the impact of radiation, medical costs, and practicality, the decision for one form of imaging over the other depends on the patient’s circumstances. For most pediatric patients with a normal mental status and benign mechanism of injury, plain cervical spine radiographs are reasonable to exclude significant CSIs with 2-3 views (anteroposterior, lateral ± open-mouth odontoid views) being standard. The use of a cross-table lateral view radiograph provides a 79% sensitivity; the addition of the AP and odontoid views increases sensitivity to 94%.7 However, the biggest pitfall in using plain radiographs is obtaining a series that adequately evaluates the cervical spine. Complete evaluation of the cervical spine requires that all seven vertebrae, including the C7/T1 junction, be visualized. Furthermore, interpreting cervical spine radiographs can be quite challenging, especially since normal anatomic variants of children, such as ligamentous laxity and incomplete ossification of the posterior elements, must be distinguished from pathological findings.12
Therefore, CT should be utilized if inadequate plain radiographs were obtained, there were suspicious findings on plain radiograph, the patient has a GCS less than 9, and with patients with a mechanism of injury and/or physical exam findings that are suspicious for CSI.13,14 The sensitivity and specificity of CT for detecting cervical spine osseous injury is about 98%.15,16 In making the decision to utilize CT imaging, the recommended study of choice is multidetector CT with sagittal and coronal reconstructions. You can also consider a limited CT up to C3 in patients less than 8 years old. However, when deciding to utilize CT one must be aware of the risks, specifically to the pediatric population, in terms of radiation exposure. CT delivers a 50% higher mean radiation dose relative to conventional radiography.17
Magnetic resonance imaging (MRI) has slowly become the imaging modality of choice, sometimes even before plain radiography and CT. However, the current practice guidelines still recommend plain radiographs and CT imaging prior to the use of MRI. MRI can be exceptionally useful for patients that have neurologic dysfunction but normal plain radiograph and CT imaging, also known as SCIWORA (Spinal Cord Injury without Radiographic Abnormality).18 This is mainly due to the fact that MRI is significantly more sensitive in visualizing soft tissues, intervertebral disk herniation, ligamentous injuries, and spinal cord damage. Unfortunately, limited access, cost, time to obtain the study, and the possible need for sedation in younger children prevent the use of MRI from being readily utilized. Despite these challenges, the benefits outweigh the risks when it comes to diagnosing CSIs.
Disposition
With regard to the treatment options for these patients, it depends on the fracture stability and concomitant injuries of the patients. For all children with neurologic abnormalities or possible CSIs, it is best to consult neurosurgery/spine service. If unavailable, immediate transfer to a center with these services should be arranged. The treatment for children with unstable cervical fractures utilizes closed reduction under fluoroscopic guidance and halo-vest immobilization, which can be applied for cervical and even upper thoracic fractures and dislocations.19 For those with no neurologic deficits and minor spinal fracture patterns on imaging, outpatient management may be possible with analgesics and follow-up care being the main components of the plan.20
CASE RESOLUTIONS
Case 1
Utilizing clinical gestalt, NEXUS, and the unvalidated PECARN criteria you decide she is at high risk for sustaining CSI (MVC vs Bicycle) and get a cervical spine x-ray series, which were inadequate, so you get a CT which was normal. You perform a thorough neurologic exam which is negative for signs of neurologic deficits with no pain or impinged range of motion, so you clear the spine and take off the C-collar and discharge the patient home with instructions to follow up with her PCP and return precautions if she begins to have any neurologic symptoms.
Case 2
Due to clinical findings and history you promptly order a CT, call neurosurgery, and admit to the trauma service ensuring that everyone on your team knows there must be strict C-spine precautions and continued C-collar use.
Take-Home Points
- C-spine injuries are rare in children
- Children less than 8 years old: C2-C3 injuries; children greater than 8 years old: C5-C6 injuries
- Use physical exam to initially clear a patient but do not hesitate to obtain imaging
- If imaging is needed start with plain films
- CT in cases of high suspicion of CSI in the context of negative or inadequate plain films or high-risk mechanism
- Can consider limited CT to C3 in younger children (3-8 years old)
- MRI if pain or neurological deficits persist despite normal CT to assess for SCIWORA
References
- Mohseni S, Talving P, Branco BC, et al. Effect of age on cervical spine injury in pediatric population: A National Trauma Data Bank Review. J Pediatr Surg. 2011;46(9):1771-1776.
- Gopinathan N, Viswanathan V, Crawford A. Cervical spine evaluation in pediatric trauma: A review and an update of current concepts. Indian J Orthop. 2018;52(5):489-500.
- Peclet MH, Newman KD, Eichelberger MR, et al. Patterns of injury in children. J Pediatr Surg. 1990;25(1):85-90.
- Leonard JR, Jaffe DM, Kuppermann N, Olsen CS, Leonard JC. Cervical Spine Injury Patterns in Children. Pediatrics. 2014;133(5):e1179-1188.
- Fesmire FM, Luten RC. The pediatric cervical spine: Developmental anatomy and clinical aspects. J Emerg Med. 1989;7(2):133-142.
- Leonard JC, Kuppermann N, Olsen C, et al. Factors Associated With Cervical Spine Injury in Children After Blunt Trauma. Ann Emerg Med. 2011;58(2):145-155.
- Baker C, Kadish H, Schunk JE. Evaluation of pediatric cervical spine injuries. Am J Emerg Med. 1999;17(3):230-234.
- Finch GD, Barnes MJ. Major Cervical Spine Injuries in Children and Adolescents. J Pediatr Ortho. 1998 Nov-Dec;18(6):811-814.
- Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001 Oct 17;286(15):1841-8.
- Hoffman R, Mower WR, Wolfson AB, et al. Validity of a Set of Clinical Criteria to Rule Out Injury to the Cervical Spine in Patients with Blunt Trauma. N Engl J Med. 2000;343(2):94-99.
- Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR, et al. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):E20.
- Ehara S, El-Khoury G, Sato Y. Cervical spine injury in children: Radiologic manifestations. Am J Roentgenology. 1988;151(6):1175-1178.
- Borock EC, Gabram SG, Jacobs LM, Murphy MA. A prospective analysis of a two-year experience using computed tomography as an adjunct for cervical spine clearance. J Trauma. 1991 Jul;31(7):1001-5.
- Hockberger RS, Kirshenbaum KJ, Doris PE. Spinal Injuries. In: Emergency medicine: concepts and clinical practice, 4th edition. Edited by Rosen, P. St. Louis (MO): Mosby-Year Book; 1998, p. 462.
- McCulloch PT, France J, Jones DL, et al. Helical computed tomography alone compared with plain radiographs with adjunct computer tomography to evaluate the cervical spine after high-energy trauma. J Bone Joint Surg Am. 2005 Nov;87(11):2388-2394.
- Sanchez B, Waxman K, Jones T, et al. Cervical spine clearance in blunt trauma: evaluation of a computed tomography based protocol. J Trauma. 2005 Jul;59(1):179-83.
- Adelgais M, Grossman DC, Langer SG, Mann FA. Use of helical computed tomography for imaging the pediatric cervical spine. Acad Emerg Med. 2004;11(3):228-236.
- American College of Radiology. Appropriateness criteria for imaging and treatment decisions. American College of Radiology, Reston, VA, 1995.
- Botte MJ, Byrne TP, Abrams RA, Garfin SR. Halo Skeletal Fixation: Techniques of Application and Prevention of Complications. J Am Acad Orthop Surg. 1996;4(1):44–53.
- Bradley LH, Paullus WC, Howe J, Litofsky NS. Isolated Transverse Process Fractures: Spine Service Management not Needed. J Trauma. 2008;65(4):832-836.



