We present the case of a 2-year-old male who was evaluated in the pediatric emergency department for acute onset, severe abdominal pain.
Point-of-care ultrasound demonstrated a large intraabdominal cystic mass at the level of the umbilicus, which was intraoperatively determined to be a fluid-filled Meckel’s diverticulum, with an associated partial small bowel obstruction.
Case
A 2-year-old male presented to the pediatric emergency department (ED) for severe abdominal pain that began one hour prior to presentation. Onset was acute, with the patient beginning to complain of pain while eating dinner, with localization to the right side of his abdomen. Review of systems was positive for increased urinary frequency on the day of presentation, and lack of bowel movements for 3 days. The family reported that he had been otherwise well. There was no associated fever, cough, congestion, polydipsia, vomiting, diarrhea, dysuria, hematuria, or rash. The family denied any preceding falls or other trauma. There were no known sick contacts, and the patient was fully immunized.
Vital signs at presentation to the ED demonstrated a temperature of 36.4°C, HR 100/min, RR 32/min, and BP 123/73 mmHg. The patient was alert and reclining on the gurney. Abdominal exam was significant for generalized moderate tenderness. Severe tenderness was localized to the periumbilical abdomen and right lower quadrant, with associated involuntary guarding. Bowel sounds were normal, and there was no abdominal distention or palpable hepatosplenomegaly. Genitourinary exam was unremarkable with no signs of inguinal hernia, testicular enlargement, or tenderness.
The initial differential diagnosis included intussusception, ileus, constipation, and appendicitis. An abdominal x-ray was obtained which showed a mildly prominent small bowel loop in the right mid abdomen, and no signs of free air or abnormal bowel gas pattern (Figure 1).

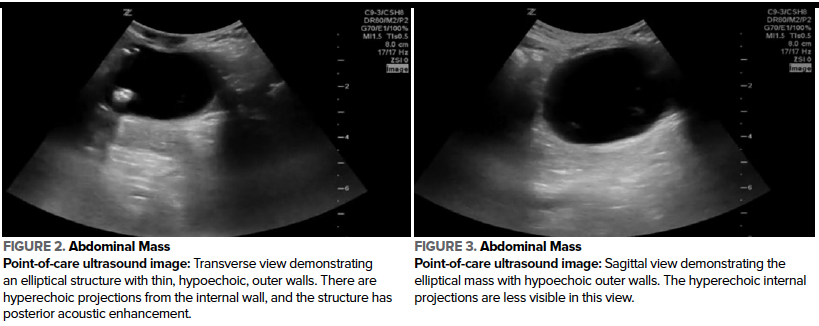
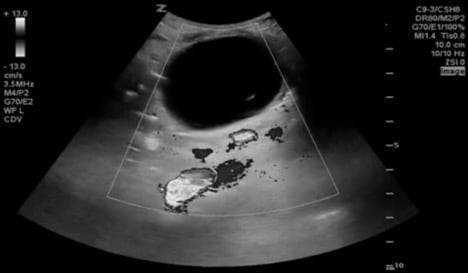
A radiology-performed ultrasound revealed a complex cystic structure with fluid levels and internal debris near the umbilicus, with a diameter of 4.6 cm. Point-of-care ultrasound by a third-year pediatric emergency fellow was performed to demonstrate the findings to the family and optimize understanding. A large, round, avascular mass was visualized in the medial abdomen, extending inferiorly from the level of the umbilicus. The contents of the mass were grossly anechoic, suggesting fluid, with hyperechoic elements on the internal walls, and there was posterior acoustic enhancement (Figure 2, 3, 4). The liver, spleen, kidneys, and bladder were visualized and were normal.
Figures 2, 3, 4. Abdominal mass
Laboratory evaluation included a complete blood cell count, C-reactive protein, and comprehensive metabolic panel that were unremarkable. Rapid testing for COVID-19, influenza, and respiratory syncytial virus was negative.
The patient was admitted to Pediatric Surgery and underwent surgical resection of the mass. Intraoperatively, the mass was found to be a fluid-filled Meckel’s diverticulum with a stalk to the mesentery of the terminal ileum. There was a partial small bowel obstruction proximal to the diverticulum, secondary to adhesions of the serosa to the small bowel. The affected bowel was resected from proximal to distal to the Meckel’s diverticulum, and end-to-end anastomosis was completed.
Intravenous ceftriaxone and metronidazole were administered as surgical prophylaxis for 2 days. The patient was discharged on postoperative day 4, at which time his pain was significantly improved, he was ambulating independently, and he was tolerating an oral diet.
Ultrasound Findings
Point-of-care ultrasound revealed a large, round mass in the infraumbilical abdomen. In the transverse and sagittal views, an elliptical mass measuring 3.6 x 4.7 x 4.2 cm was visualized. The walls of the structure were thin and layered in appearance. The internal walls of the structure were hyperechoic with hyperechoic projections to the interior, and the surrounding wall was hypoechoic. The internal contents were grossly anechoic, suggestive of fluid, and the overall structure demonstrated posterior acoustic enhancement (Figure 2, 3). Using color Doppler, vascular flow was visualized to the surrounding tissue, and there was absent vascular flow within the mass (Figure 4).
Ultrasound Technique
Point-of-care ultrasound for pediatric abdominal evaluation is performed using the low frequency curvilinear and phased array transducers.1,2 The linear transducer includes higher frequencies and is preferred when evaluating superficial structures due to improved resolution.1,3,4 The curvilinear transducer is favored in patients of larger habitus and for structures at greater depths due to the transducer’s larger footprint and optimal tissue penetration.1–3 When evaluating the abdomen for pathology, the exam should start at the site of greatest pain or tenderness.4,5 For inspection of the target area, water-based gel is applied and the minimum pressure needed for visualization is utilized to maximize patient comfort.1,3,4
Graded compression is the recommended technique for evaluation of the bowels and lower abdomen for pathology. This technique displaces bowel gas and improves visualization of the evaluated intraabdominal structures.1,3–5 When an abnormality is visualized, the transducer should be rotated 90 degrees to evaluate the area in 2 planes.2,4,6 Any fluid-filled structures may demonstrate posterior acoustic enhancement.2,3
Ultrasound can optimally be used to reveal the Meckel’s diverticulum as a blind outpouching of bowel projecting from the small intestine.7,8 The appearance of Meckel’s diverticulum varies based on whether the structure is inflamed. In both cases, the diverticulum may contain visible fluid and gas.7,9 A gut signature, which refers to the multilayer appearance of bowel, is often appreciated.5,7,9,10 Ultrasound can be used to visualize the bowel layers surrounding the fluid-filled contents: a hyperechoic inner layer that is often irregular and represents the mucosa and submucosa, a hypoechoic intermediate muscular layer, and a hyperechoic outer serosal layer.8,10 Color Doppler should be used during the evaluation, as when the diverticulum is inflamed, the structure’s walls appear thickened and hyperemic in comparison to normal bowel wall.5,7,9,10
Discussion
Meckel's diverticulum is a true diverticulum and is a congenital remnant of the omphalomesenteric duct that is present in 2% of the general population. The structure is present in the ileum, 40 to 100 cm proximal to the ileocecal valve. Its diameter is typically reported as approximately 2 cm; however, cases have been described with diameters up to 10 cm.8,11 The majority of these diverticula are asymptomatic, with 4.2 to 9% of patients with Meckel’s diverticulum developing symptoms in their lifetime.12 46.7% of children present with small bowel obstruction as our patient did, including cases secondary to volvulus or intussusception, compared to 25.3% who present with painless rectal bleeding, and 19.5% who present with diverticulitis.7,8,11,12 Complications of Meckel’s diverticulum can present at any age; however, they more commonly present in pediatric patients, with the median age ranging from 4 to 5 years.12
Point-of-care ultrasound has been described as a viable first-line imaging modality used for the detection of Meckel’s diverticulum in symptomatic patients.5,9 The presentation of appendicitis and symptomatic Meckel’s diverticulum can be similar, in particular with cases of diverticulum-associated obstruction and inflammation, which may present with fever, nausea, vomiting, and right lower quadrant pain.5,6,9 Like appendicitis, focal pain for a symptomatic Meckel’s diverticulum may also be reported as periumbilical.5,13
The sonographic commonalities of the appendix and Meckel’s diverticula can further hinder differentiation, including the gut signature created by the multiple bowel layers, as well as the non-compressibility, thickened hyperemic walls, and lack of peristalsis appreciated in both appendicitis and inflamed Meckel’s diverticula.5,6,8,9 However, visualization of the normal compressible appendix with point-of-care ultrasound assists with narrowing the differential, when considering small bowel abnormalities such as Meckel’s diverticulum.5 Additionally, Meckel’s diverticulum is typically larger than the non-compressible structure seen with appendicitis and is located in a different site. Meckel’s diverticulum is approximately 2 cm in diameter by 5 cm in length and is located a greater distance from the cecum than the appendix. In comparison, the appendix is attached directly to the cecum, and the defining diameter of appendicitis is greater than 0.6 cm.5,8,13 As in our case, the Meckel’s diverticulum can sometimes be visualized in the area of the umbilicus, or it may be visible in the lower abdomen or right lower quadrant.5,6,9,10
Conclusion
Point-of-care ultrasound can be used to detect Meckel’s diverticulum as the underlying etiology of lower abdominal pain in pediatric patients. In our case, bedside family-centered teaching and demonstration of the findings was a direct benefit of point-of-care ultrasound. Expedited management is an associated potential benefit of point-of-care ultrasound to evaluate abdominal pain by experienced providers.
References
- Ma OJ, Mateer JR, Reardon RF, Byars D V., Knapp BJ, Laudenbach AP. Ma and Mateer’s Emergency Ultrasound. 4th ed. McGraw-Hill; 2020.
- Dawson M, Mallin M. Introduction to Bedside Ultrasound: Volume 1. Emergency Ultrasound Solutions; 2013.
- Mallin M, Dawson M. Introduction to Bedside Ultrasound: Volume 2. Emergency Ultrasound Solutions; 2013.
- Katz Lavine E, Saul T, Frasure SE, Lewiss RE. Point-of-Care Ultrasound in a Patient With Perforated Appendicitis. Pediatr Emerg Care. 2014;30(9):665-667. doi:10.1097/PEC.0000000000000219
- Kornblith AE, Doniger SJ. Point-of-Care Ultrasonography for Appendicitis Uncovers Two Alternate Diagnoses. Pediatr Emerg Care. 2016;32(4):262-265. doi:10.1097/PEC.0000000000000623
- Choi J, Dorinzi N, Pagenhardt J, Steratore A, Sharon M, Minardi J. Sonographic Detection of a Torsed Meckel’s Diverticulum Misinterpreted as Acute Appendicitis. Clin Pract Cases Emerg Med. 2019;3(3):278-281. doi:10.5811/cpcem.2019.5.42976
- Elsayes KM, Menias CO, Harvin HJ, Francis IR. Imaging manifestations of Meckel’s diverticulum. Am J Roentgenol. 2007;189(1):81-88. doi:10.2214/AJR.06.1257
- Francavilla ML, Anupindi SA, Kaplan SL, Biko DM. Ultrasound assessment of the bowel: inflammatory bowel disease and conditions beyond. Pediatr Radiol. 2017;47(9):1082-1090. doi:10.1007/s00247-017-3877-y
- Friedman N, Gauthey M, Lee MS. Young Male With Abdominal Pain. Ann Emerg Med. 2019;73(1):e7-e8. doi:10.1016/j.annemergmed.2018.07.015
- Baldisserotto M. Color Doppler Sonographic Findings of Inflamed and Perforated Meckel Diverticulum. J Ultrasound Med. 2004;23(6):843-848. doi:10.7863/jum.2004.23.6.843
- Srisajjakul S, Prapaisilp P, Bangchokdee S. Many faces of Meckel’s diverticulum and its complications. Jpn J Radiol. 2016;34(5):313-320. doi:10.1007/s11604-016-0530-x
- Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Med (United States). 2018;97(35):1-9. doi:10.1097/MD.0000000000012154
- Rentea RM, St Peter SD, Snyder CL. Pediatric appendicitis: state of the art review. Pediatr Surg Int. 2017;33(3):269-283. doi:10.1007/s00383-016-3990-2



