Tuberculosis (TB) continues to be one of the leading causes of death worldwide, with an estimated 10 million new cases in 2019.
Forty-four percent of those cases occurred in Southeast Asia and 25% occurred in Africa.1 Recognition of risk factors for and classic signs and symptoms of pulmonary TB (prolonged cough, night sweats, fever, weight loss, travel to endemic areas, and contact with the disease), followed by prompt initiation of pharmacotherapy (usually with rifampin, isoniazid, pyrazinamide, and ethambutol, known as "RIPE" therapy) has helped save approximately 60 million lives since the early 2000s.1,2
Abdominal TB involves the gastrointestinal tract, peritoneum, abdominal viscera, or lymph nodes and makes up about 5% of TB cases worldwide.3 A subtype of abdominal TB is omental TB.4 It is characterized by "large omental masses, matted and tethered bowel loops and mesentery."4 Non-specific findings of ascites and lymphadenopathy make this diagnosis challenging to differentiate from other intra-abdominal pathologies.5 Here we present a case report in which point-of-care ultrasound (POCUS) was instrumental to diagnosing omental TB.
Case Report
A 19-year-old male presented to the emergency department from a United States Immigration and Customs Enforcement (ICE) detention center with subjective fevers, cough, and body aches for 12 days. He left his hometown in Punjab, India, and was detained a few days later by ICE in Texas, approximately 4 weeks before being seen. The accompanying transfer paperwork noted "pulmonary TB," but no additional medical information was provided. The patient denied abdominal pain, nausea, vomiting, diarrhea, shortness of breath, chest pain, recent weight changes, sore throat, or rashes/wounds. He denied any history of the human immunodeficiency virus (HIV), hepatitis, TB, malignancy, sexual activity, or use of drugs or alcohol.
Initial vital signs showed a temperature of 39.1°C, heart rate of 125 bpm, blood pressure of 89/50, respiratory rate of 21, and oxygen saturation of 96% on room air. On physical examination, he appeared alert, diaphoretic, and had notably dry mucous membranes. He showed no signs of respiratory distress, abdominal swelling, or tenderness to palpation.
A rapid ultrasound for shock and hypotension (RUSH) exam was performed to evaluate for undifferentiated hypotension. POCUS showed free fluid in the pelvis and in the right and left upper quadrants (Image 1), a flat inferior vena cava, and hyperdynamic left ventricle but no other concerning findings. Due to concern for sepsis, the patient was started on intravenous (IV) vancomycin and ceftriaxone along with IV fluid boluses, which led to improvement of his heart rate and blood pressure.
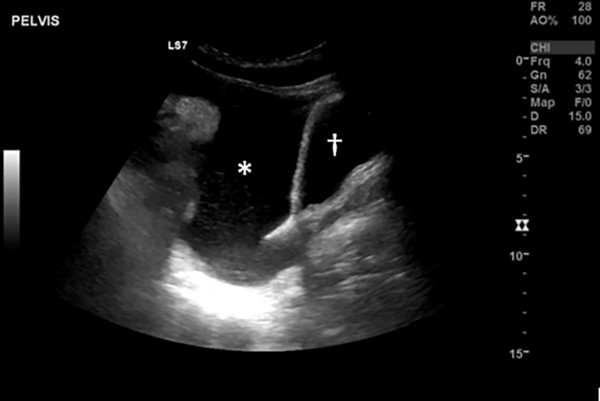
Image 1: Pelvic ultrasound, sagittal view. A large amount of free fluid(*) is seen between the bowel (left of screen) and bladder(†).
Initial work-up was notable for a negative chest radiograph, a normal white blood cell count (7.2), microcytic anemia (Hg 10.7, MVC 56), normal lactate at 1.4, and a C-reactive protein (CRP) elevated to 133. A computerized tomography (CT) scan of the abdomen and pelvis with IV contrast demonstrated a large volume of simple-appearing ascites of uncertain origin along with hepatosplenomegaly. Pending labs included blood cultures, urine culture, HIV antibodies, thick and thin malaria smears, hepatitis antibody panel, and QuantiFERON-TB Gold. The pediatric infectious disease service was consulted, and their primary concern was for dengue viral infection and typhoid fever. The patient was admitted to the pediatric intensive care unit for further evaluation and treatment.
Additional labs for Epstein-Barr, dengue, toxoplasma, leishmania, and schistosoma were negative, but the patient's QuantiFERON-TB Gold test returned positive. On day 4 of admission, the patient continued to be febrile, tachycardic, and intermittently hypotensive despite receiving broad-spectrum IV antibiotics.
A repeat CT of the abdomen and pelvis with IV contrast showed persistent large-volume ascites with mild diffuse peritoneal enhancement. A thickened/edematous omentum was also noted. The persistent hepatosplenomegaly and findings of omental and peritoneal inflammation raised concern for TB peritonitis (Images 2 and 3).

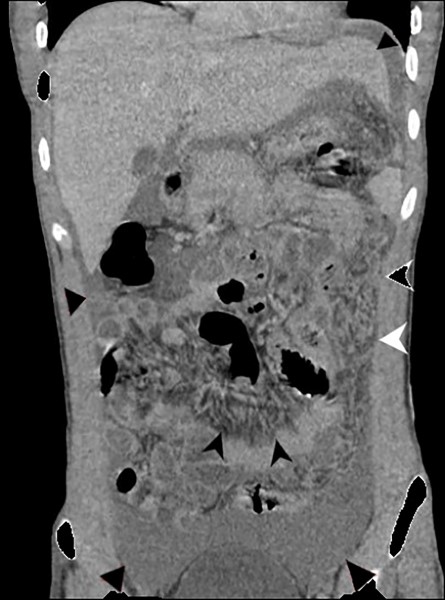
Images 2 and 3: Axial and Coronal CT abdomen/pelvis images showing diffuse ascites (black triangles), mesenteric edema (black arrows), and thickening of omentum (white arrows).
Case Conclusion
On day 6 of admission, the patient underwent a diagnostic laparoscopy, during which sampling of the ascites and biopsies of the omentum/peritoneum were performed. Necrotizing and non-necrotizing granulomas in addition to rare amounts of acid-fast bacilli were found, supporting the diagnosis of sepsis from peritoneal TB.
Treatment with RIPE therapy plus pyridoxine was initiated, leading to rapid resolution of the patient's sepsis. The patient was discharged to the ICE detention facility on day 13 of admission.
Discussion
TB most commonly presents as a pulmonary syndrome. However, the classical symptoms of pulmonary TB are not always observed in extrapulmonary TB cases. Only an estimated 15-25% of cases of abdominal TB have concomitant pulmonary TB findings.6
Abdominal involvement usually presents with nonspecific symptoms such as persistent fever and abdominal pain or swelling, which mimic many other intra-abdominal pathologies. For this reason, abdominal TB should be on the differential diagnosis for patients presenting with these symptoms who have epidemiological risk factors for TB, recent contact with the disease, or who are immunocompromised.
In this case, the patient's hypotension was evaluated using the RUSH (Rapid Ultrasound in Shock and Hypotension) protocol to evaluate the "pump, tank, and pipes."11 The pump refers to the heart, which is assessed by evaluating for gross left ventricular function and for the presence or absence of a pericardial effusion. The tank refers to intravascular volume status, which is assessed via two steps. First, the inferior vena cava is measured to evaluate the volume status of the patient. Second, the pleural and abdominal spaces are assessed for pathology that could compromise intravascular volume. "Pipes" refers to the large arteries and veins. The aorta is scanned for evidence of aneurysm or dissection. The femoral and popliteal veins are evaluated for lack of compressibility which may be suggestive of a deep venous thrombosis.11
In the setting of possible TB in this case, POCUS allowed for the evaluation of the patient's lungs in a negative pressure room, reducing the risk of exposure to the rest of the ED during transport to radiology. The remainder of the RUSH exam evaluated the heart and abdomen for potential causes of shock. Identifying large amounts of abdominal free fluid in this case was unexpected, especially since the patient had no signs of distention or tenderness. This helped to direct the team's attention towards intra-abdominal pathology.
POCUS Advancements
The use of POCUS to diagnose extrapulmonary TB is a novel area of research that has been conducted largely in areas where TB is highly endemic. Research performed in South Africa and India has used the Focused Assessment with Sonography for TB-HIV (FASH) protocol to investigate the effectiveness of POCUS in detecting positive findings of TB in HIV-positive patients.
The FASH protocol is based on the Focused Assessment with Sonography in Trauma (FAST) exam,12 with 6 additional probe positions to assess periportal/para-aortic lymph nodes, focal hepatic/splenic lesions, and pericardial/pleural effusion and ascites.8
One research study using the FASH exam for TB in HIV-positive and HIV-negative patients showed approximately one-third of all participants had positive findings.9 Abdominal lymphadenopathy and splenic microabscesses were strongly associated with the diagnosis of TB in HIV-positive patients. Additionally, in a subset of patients with negative chest radiography, POCUS provided sonographic evidence of extrapulmonary TB. Among HIV-negative patients, positive FASH exam findings did not correlate specifically to TB but provided the basis for further investigation into possible malignancy or other infectious disease.9
A different study with pediatric patients found that one-third of patients diagnosed with pulmonary TB also had evidence of extrapulmonary TB.10 Pleural effusions and abdominal lymphadenopathy were the most common findings, although splenic microabscesses had the strongest correlation with confirmed pulmonary TB. HIV-positive children with TB were more likely to have evidence of abdominal lymphadenopathy and splenic microabscesses compared to HIV-negative children with TB.10 These results support the use of the FASH exam in at-risk patients who have TB symptoms but do not have chest imaging findings of pulmonary TB.
POCUS may also be used to identify peritoneal, omental, or bowel wall thickening with no additional radiation exposure.6 On ultrasound, omental TB is seen as a hyperechoic mass located anterior to the intestines. In retrospective studies reviewing ultrasound imaging of patients diagnosed with omental TB, a hyperechoic mass was able to be distinguished from the intestines and/or anterior abdominal wall 14-55% of the time.3,6 Therefore, ultrasound may be used as an aid to guide further workup but lacks specificity. Computed tomography is the best test for omental TB.
Summary
Diagnosing extrapulmonary TB is difficult; it is characterized by non-specific symptoms and diverse patient presentations. Using POCUS in the diagnosis is novel and may not translate well where TB has low prevalence, such as the U.S. However, in the setting of suspicious epidemiological factors, unusual abdominal findings, and undifferentiated hypotension, a RUSH and/or FASH exam may provide evidence for extrapulmonary TB. Additionally, in patients with significant risk factors, a positive RUSH exam can warrant further investigation with a FASH exam.
Take-Home Points
- In the setting of possible TB, the RUSH exam allowed evaluation of the lungs and undifferentiated hypotension in a negative pressure room, mitigating the risk of exposure.
- Abdominal TB should be on the differential for patients with nonspecific symptoms (persistent fever, abdominal pain, distension) who have epidemiological risk factors for TB, recent disease contacts, or immunocompromised.
- In this context, a positive RUSH exam can trigger further investigation with a FASH exam.
REFERENCES
- Global tuberculosis report 2020. World Health Organization. https://www.who.int/tb/publications/global_report/en/. Published October 26, 2020. Accessed October 28, 2020.
- Bernardo J. (2020) Diagnosis of pulmonary tuberculosis in adults. In C. F. von Reyn, & E. Baron (Eds.) UpToDate. Available from: https://www.uptodate.com/contents/diagnosis-of-pulmonary-tuberculosis-in-adults.
- Vineet, A. (2019) Abdominal Tuberculosis. In S. Chopra, J. Bernardo, & E. Baron (Eds.) UptoDate. Available from: https://www.uptodate.com/contents/abdominal-tuberculosis
- Dhiman DS, Goyal D, Prakash S, et al. Omental tuberculosis. Indian Journal of Radiology and Imaging. http://www.ijri.org/article.asp?issn=0971-3026;year=2004;volume=14;issue=2;spage=191;epage=192;aulast=Dhiman. Published 2004. Accessed December 23, 2019.
- Gökten B, Dilara, Bilal, et al. A Case Report of Peritoneal Tuberculosis: A Challenging Diagnosis. Case Reports in Infectious Diseases. https://new.hindawi.com/journals/criid/2018/4970836/. Published January 11, 2018. Accessed December 24, 2019.
- Debi U, Ravisankar V, Prasad KK, et al. Abdominal tuberculosis of the gastrointestinal tract: revisited. World journal of gastroenterology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4209546/. Published October 28, 2014. Accessed December 23, 2019.
- Demirkazik FB, Akhan O, Ozmen MN, et al. CT findings in the diagnosis of tuberculous peritonitis. Acta radiologica (Stockholm, Sweden : 1987). https://www.ncbi.nlm.nih.gov/pubmed/8688233. Published July 1996. Accessed January 11, 2020.
- Heller T, Wallrauch C, Goblirsch S, Brunetti E. Focused assessment with sonography for HIV-associated tuberculosis (FASH): a short protocol and a pictorial review. Crit Ultrasound J. 2012;4(1):21. Published 2012 Nov 21. doi:10.1186/2036-7902-4-21
- Weber SF, Saravu K, Heller T, et al. Point-of-Care Ultrasound for Extrapulmonary Tuberculosis in India: A Prospective Cohort Study in HIV-Positive and HIV-Negative Presumptive Tuberculosis Patients. Am J Trop Med Hyg. 2018;98(1):266–273.
- Bélard S, Heuvelings CC, Banderker E, et al. Utility of Point-of-care Ultrasound in Children With Pulmonary Tuberculosis. Pediatr Infect Dis J. 2018;37(7):637–642.
- Perera P, Mailhot T, Riley D, et al. The RUSH Exam: Rapid Ultrasound in Shock in the Evaluation of the Critically Ill. Emergency Medicine Clinics of North America. 2010;28(1):29-56.
(12) Richards JR, Mcgahan JP. Focused Assessment with Sonography in Trauma (FAST) in 2017: What Radiologists Can Learn. Radiology. 2017;283(1):30-48.



